
Understanding the Fine Print: Key Contract Clauses Every Doctor Must Comprehend
Entering practice is one of the biggest transitions in a physician’s life. Years of training in diagnosis, procedures, and patient care rarely include formal education in Physician Contracts, Employment Law, or the legal considerations that shape your first (and subsequent) jobs. Yet the contract you sign at the end of residency or fellowship can have more impact on your long-term Career Development than almost any single decision you make.
This guide breaks down the key contract clauses every physician should understand before signing. Whether you’re a new graduate evaluating your first offer or an experienced attending considering a new opportunity, knowing what to look for—and what to question—will help you protect your interests, align your work with your priorities, and avoid costly surprises down the road.
1. Compensation, Benefits, and the True Value of Your Offer
Compensation is often the first thing physicians focus on, but the salary number alone rarely tells the whole story. You need a detailed understanding of how you’ll be paid, what’s guaranteed, what’s at risk, and which benefits meaningfully affect your finances and lifestyle.
Base Salary and Compensation Structure
Your contract should clearly state:
- Base salary: The guaranteed amount, usually expressed as an annual figure.
- Pay frequency: Monthly, biweekly, etc.
- Duration of the guarantee: One year? Two years? Longer?
- Review schedule: When and how compensation will be reassessed.
Common compensation models:
- Straight salary: Predictable but may be lower than production models.
- Salary + productivity bonus: Based on RVUs, collections, or net income.
- Pure productivity: Typically in independent or highly entrepreneurial settings.
Key questions to ask and clarify:
- How is productivity measured (wRVUs vs collections)?
- When does the productivity component start (immediately or after a ramp-up period)?
- Is there a clawback if I fail to meet certain thresholds?
- Are there caps on bonuses?
Actionable tip: Compare the offer against national benchmarks (e.g., MGMA, AAMC, specialty society data) adjusted for region, practice type, and call responsibilities. This is critical Healthcare Advice for understanding whether your offer is competitive.
Bonuses and Incentive Pay
Your contract may include:
- Signing bonuses
- Retention bonuses
- Quality or value-based incentives (e.g., patient satisfaction, readmission rates)
- Leadership stipends (medical director roles)
Ensure that:
- Conditions for earning and keeping the bonus are clearly spelled out.
- You understand repayment obligations if you leave before a specified period.
- Quality metrics are objective, achievable, and within your control.
Benefits Package: Beyond the Paycheck
Benefits can significantly increase the total value of your compensation:
- Health, dental, and vision insurance: Confirm employer/employee premium split, deductibles, and coverage tiers.
- Retirement plans: 401(k), 403(b), 457(b), or pension plans.
- Employer match percentage and vesting schedule.
- Eligibility timeline (some plans have a waiting period).
- Paid time off (PTO): Vacation, sick time, holidays, and CME days.
- Disability and life insurance: Short-term and long-term disability; employer-paid vs optional.
- Professional expenses: Licensing, DEA, board certification, society dues, journal subscriptions.
- Relocation assistance: Repayment obligations if you leave early.
- Student loan assistance: Terms, duration, and any clawback provisions.
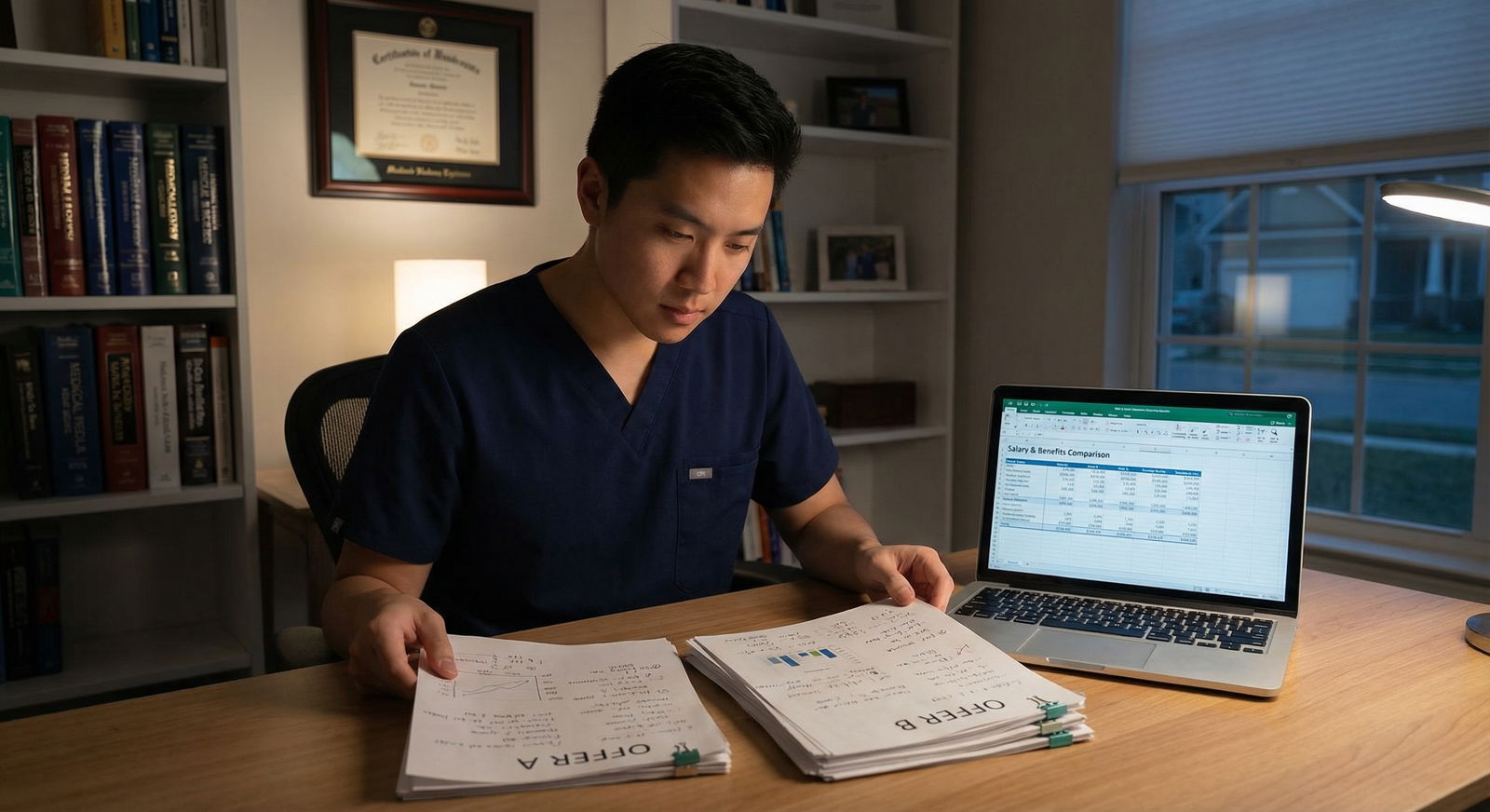
Actionable tip: Create a simple spreadsheet to compare offers, assigning realistic financial values to benefits. This clarifies which offer truly supports your long-term Career Development—especially when comparing academic vs private practice settings.
2. Employment Status, Duties, and Workload Expectations
Your legal relationship to the practice affects everything from taxes and benefits to malpractice liability and autonomy. Equally important is clarity about what, exactly, you’re being hired to do and under what conditions.
Employment Status and Legal Considerations
Common statuses include:
W-2 Employee (most hospital/large group jobs)
- Employer withholds taxes.
- Typically eligible for benefits.
- Employment Law protections usually clearer and more robust.
1099 Independent Contractor
- You handle your own taxes, benefits, and sometimes malpractice.
- Potentially higher headline compensation but more risk and fewer protections.
- May allow more flexibility but requires meticulous financial planning.
Partner/Shareholder Track
- Often begins as an employee with the option to buy into the practice.
- Partnership terms should be outlined or referenced (buy-in amount, timing, governance rights, and buy-out formula).
Key Physician Contract questions:
- What is my exact legal status?
- Am I eligible for benefits, and when?
- If there is a partnership track, is it guaranteed or discretionary?
Defined Duties and Scope of Practice
Your contract should clearly describe:
- Clinical responsibilities: Inpatient vs outpatient, procedures, call coverage.
- Administrative duties: Committee work, quality projects, EMR implementation.
- Teaching/research expectations in academic positions.
- Patient panel expectations: Target volumes and ramp-up expectations.
Ambiguous language like “other duties as assigned” is common but should be reasonable in scope. Ask that any major non-clinical responsibilities (e.g., program leadership roles) be named and, ideally, separately compensated.
Work Hours, Call, and Work–Life Balance
A comprehensive Work Hours section should specify:
- Typical clinic hours and number of sessions per week.
- Inpatient weeks or shifts per month.
- Call schedule: frequency, type (home vs in-house), and compensation.
- Expectations for weekend/holiday coverage.
- Telemedicine responsibilities, if applicable.
Clarify:
- Is call equitably distributed among physicians?
- Can call responsibilities change over time, and how is that decided?
- How is overtime or extra call compensated?
These details strongly influence burnout risk and overall job satisfaction, particularly in the early post-residency years.
3. Restrictive Covenants: Non-Compete and Non-Solicitation Clauses
Restrictive covenants are among the most consequential parts of any physician contract. They shape your future mobility and options if the job doesn’t work out.
Non-Compete Agreements (Restrictive Covenants)
A non-compete clause typically limits:
- Where you can practice (geographic radius or defined area).
- For how long after leaving (e.g., 1–2 years).
- In what capacity (any practice of medicine vs specific specialty).
Key Legal Considerations:
- Non-compete enforceability varies widely by state.
- Some states restrict or prohibit non-competes for physicians entirely.
- Courts often look at whether the scope is reasonable (geographically and temporally).
Questions to ask:
- What is the exact radius and how is it measured (from one office or multiple sites)?
- Does it apply if the employer terminates you without cause?
- Is the restriction specialty-specific or any medical practice?
Negotiation strategies:
- Narrow the radius or exclude certain locations.
- Shorten the time period (e.g., 6–12 months instead of 24).
- Ask for the non-compete to be void if you are terminated without cause.
- Limit the restriction to specific clinical activities (e.g., interventional cardiology but not general cardiology).
Non-Solicitation Clauses
Non-solicitation typically prohibits you from:
- Actively encouraging patients to follow you to a new practice.
- Recruiting staff or other physicians from your former employer.
These clauses are generally more enforceable and considered more reasonable than non-competes, but they still deserve careful review.
Clarify:
- Does it prohibit you from treating patients who independently seek you out?
- How is “solicitation” defined?
- Does it prevent you from contacting colleagues socially about opportunities, or only active recruiting?
For Career Development planning, consider how these restrictions would impact your ability to build a practice if you needed to leave after a few years.
4. Termination, Malpractice Coverage, and Liability Protection
Many physicians focus heavily on starting a job but give less attention to how it might end. Yet the termination and malpractice provisions often determine how smoothly you can exit and how protected you are during and after your employment.
Termination Clauses: With and Without Cause
Most Physician Contracts include:
Termination with cause
- Based on defined serious issues (e.g., loss of license, fraud, substance abuse, patient safety concerns).
- Should be specific and not overly broad or vague.
Termination without cause
- Either party can end the relationship without a specific reason.
- Requires a notice period, commonly 60–180 days.
Ensure:
- The notice period is practical and not excessively long.
- You have protection from immediate termination without cause (except under serious “for cause” conditions).
- There is clarity on what happens to bonuses, tail coverage, and benefits upon termination.
Malpractice Insurance: Claims-Made vs Occurrence
Your contract must explain:
Type of malpractice coverage:
- Claims-made: Covers claims made while the policy is active (you may need tail coverage when leaving).
- Occurrence: Covers incidents that occurred during the policy period, regardless of when the claim is filed (no tail needed).
Who pays for what:
- Is malpractice fully employer-funded?
- Are there deductibles or self-insured retention (SIR) amounts?
- Who pays for tail coverage (and under what circumstances)?
Tail coverage can cost 1–3 times your annual premium and is a major financial risk if not addressed. This is a critical Healthcare Advice point for any physician changing jobs.
Actionable tip: Negotiate for:
- Employer-paid tail coverage if they terminate you without cause.
- Shared responsibility or prorated tail cost if you leave voluntarily.
- Written confirmation of coverage limits (e.g., $1M/$3M) and carrier quality.
Indemnification and Limitations of Liability
Indemnification clauses define who is financially responsible if a lawsuit arises from your work. Be cautious with:
- Broad indemnification requiring you to cover the employer’s costs for certain claims.
- Unbalanced clauses that shift unreasonable risk to you.
You should:
- Understand your personal exposure.
- Seek to limit indemnification to conduct that is clearly negligent, intentional, or outside the scope of your employment.
- Avoid personally guaranteeing practice debts or liabilities unrelated to your own practice of medicine.
If the language is confusing or feels one-sided, consult an attorney experienced in healthcare Employment Law before signing.
5. CME, Credentialing, Policies, and Practice Infrastructure
Your contract also shapes how you maintain your competence, remain compliant, and function effectively within the healthcare system.
Continuing Medical Education (CME) Support and Requirements
Important CME elements include:
- Annual CME allowance: Dollar amount and number of days off.
- Covered expenses: Conference fees, travel, lodging, board review courses, online modules.
- Required CME topics: E.g., opioid prescribing, ethics, quality improvement.
Clarify:
- Can unused CME funds roll over?
- Is conference time counted separately from vacation?
- Are there must-attend internal meetings or retreats?
Strong CME support is not just a perk; it’s part of sustainable Career Development and helps you remain competitive in your field.
Credentialing, Licensing, and Practice Policies
Your contract should address:
Licensing and certification:
- Who pays for state licenses, DEA registration, board certification, and renewals?
- Who manages the credentialing process with hospitals and insurers?
Practice policies and procedures:
- Reference to an employee handbook or medical staff bylaws is common.
- You should have the right to review these documents before signing or at least before starting.
Quality metrics and documentation expectations:
- EMR templates, coding requirements, productivity reporting.
- Time expectations for chart completion and compliance audits.
Understanding the operational environment is a crucial aspect of practical Healthcare Advice—especially if prior physicians have struggled with unrealistic documentation or metric requirements in the same setting.

6. Retirement, Exit Strategy, and Long-Term Career Planning
Your first job may not be your last, and your contract should support—not obstruct—your long-term goals.
Retirement Plans and Long-Term Financial Security
Review in detail:
Retirement plan options (401(k), 403(b), 457(b), defined benefit plans):
- Employer contribution/match.
- Vesting schedule (how long until employer contributions are fully yours).
- Investment options and fees.
Profit sharing or equity opportunities in private practices:
- How and when these are allocated.
- Whether they depend on production, seniority, or other factors.
Solid retirement benefits can substantially increase the real value of a slightly lower salary offer, especially over a multi-decade career.
Exit Strategy: Planning for Change
Even in a great position, circumstances change—leadership turnover, new ownership, personal moves, or family needs. A thoughtful exit strategy is a key part of Career Development.
Key items:
Notice requirements and how to deliver notice correctly (written, to whom, by what method).
Post-termination obligations:
- Return of property and patient lists.
- Completion of charts and billing documentation.
- Cooperation with ongoing legal matters.
Financial wrap-up:
- Final payment of bonuses or productivity compensation.
- Handling of accounts receivable in productivity or partnership models.
- Timing of last paycheck and payout of unused PTO (if allowed by state law and employer policy).
Actionable tip: Ask for an explicit description of what happens if:
- You choose to leave voluntarily.
- You are terminated without cause.
- The practice is sold or merges with another entity.
This protects you from surprise non-competes activating under new ownership or losing expected benefits after a change in control.
Real-World Case Example: How Contract Review Changed a Career
Consider Dr. Emily, a recent graduate who received an attractive hospital-employed offer in a mid-sized city where she hoped to settle long-term.
On initial review, the offer seemed excellent:
- Competitive starting salary.
- Signing bonus.
- Reasonable call schedule.
However, a closer look at the Physician Contract revealed several issues:
Non-compete
She would be barred from practicing within a 30-mile radius for two years after leaving—for any reason, including termination without cause. Given that most neighboring hospitals and clinics were within that radius, this would effectively force her to relocate if the job ended prematurely.Malpractice and tail coverage
The contract stated that the hospital provided claims-made coverage but was silent on who paid for tail insurance. For her specialty, tail coverage could easily reach six figures if she left after several years.Termination notice
Dr. Emily would be required to give 180 days’ notice if she wished to resign, while the employer could terminate her without cause with only 60 days’ notice—a stark imbalance.
Recognizing the stakes, Dr. Emily consulted an attorney specializing in physician Employment Law and contracts. With guidance, she successfully negotiated:
- A reduced non-compete radius and shorter duration.
- Employer-funded tail coverage if she was terminated without cause or the position was eliminated.
- A symmetrical notice period of 90 days for both parties.
These changes did not alter her day-to-day clinical work but dramatically improved her long-term security and flexibility. By investing time upfront and seeking expert Healthcare Advice, she positioned herself for a more stable and adaptable career.
FAQs: Physician Contracts, Legal Issues, and Career Decisions
Q1. When should I hire an attorney to review my physician contract?
It’s wise to involve a healthcare-focused attorney before you sign anything—ideally as soon as you receive the written offer. While not every contract needs exhaustive revision, a brief review can:
- Flag problematic non-compete or indemnification clauses.
- Suggest targeted edits that are standard in your specialty and region.
- Help you prioritize changes worth negotiating.
For high-stakes Physician Contracts (e.g., partnership tracks, large systems, or complex compensation models), professional review is strongly recommended.
Q2. Are non-compete clauses for physicians always enforceable?
No. Enforceability depends heavily on state law and the specifics of the clause. Some states restrict or ban physician non-competes altogether, while others uphold them if they are reasonable in:
- Geographic scope
- Duration
- Relation to a legitimate business interest
Because this is a nuanced Legal Consideration, you should:
- Learn your state’s stance on physician non-competes.
- Ask for narrowing or modification of overly broad restrictions.
- Seek legal counsel if there is any doubt about the potential impact.
Q3. What contract elements should I prioritize in negotiations?
While every situation is unique, most physicians should focus on:
- Non-compete and restrictive covenants (long-term mobility).
- Malpractice and tail coverage (financial and legal protection).
- Compensation structure and transparency (fair pay, realistic targets).
- Termination terms and notice periods (security and planning).
- Call, workload, and schedule expectations (burnout risk and work–life balance).
Once those are solid, you can fine-tune secondary items like CME dollars, signing bonus terms, and specific benefit details.
Q4. What happens if I start working without a fully executed contract?
Starting work without a signed contract is risky. You may fall back on default state Employment Law (which is often “at-will”) and have little protection regarding:
- Non-compete or non-solicitation obligations.
- Malpractice coverage details and tail.
- Compensation disputes or changes to your schedule.
If circumstances require you to start quickly, at minimum ensure you have a signed offer letter or interim agreement that clearly spells out key terms (compensation, malpractice, termination, and restrictive covenants) while the final contract is completed.
Q5. How can I tell if a contract offer is fair for my specialty and location?
Use a combination of data and peer input:
- Benchmark data: MGMA, AAMC, specialty society surveys, and regional salary reports.
- Colleagues and mentors: Ask recent graduates or attendings in similar practices what they are seeing.
- Professional advisors: Attorneys or consultants who regularly work on Physician Contracts in your region.
Look beyond the base salary; evaluate:
- Total compensation (including bonuses and benefits).
- Call burden and schedule.
- Non-compete severity.
- Malpractice and tail responsibilities.
A “fair” contract balances reasonable compensation with sustainable working conditions and preserves your ability to grow and adapt throughout your career.
Navigating your first—or next—physician contract can feel overwhelming, but you don’t need to become a lawyer to protect yourself. By understanding these core clauses, asking focused questions, and seeking targeted legal and career guidance when needed, you transform your contract from a stack of fine print into a powerful tool for long-term Career Development and professional security.





















