
In a healthcare system often dominated by rushed visits, complex technology, and high burnout rates, lifestyle medicine offers something refreshingly different: a way to practice evidence-based, relationship-centered care that prioritizes preventive care, holistic health, and physician well-being.
For medical students and residents exploring specialties—especially those interested in the most lifestyle-friendly specialties—lifestyle medicine represents not just a clinical approach, but a philosophy of care that can be integrated across disciplines: internal medicine, family medicine, pediatrics, PM&R, endocrinology, cardiology, and even psychiatry.
Below, we’ll deepen the original discussion of lifestyle medicine, explore why it’s so attractive to both physicians and patients, and outline practical ways to bring these principles into your training and future practice.
Understanding Lifestyle Medicine: Foundation of Preventive and Holistic Care
Lifestyle medicine is a clinical discipline that uses evidence-based lifestyle interventions to prevent, treat, and often reverse chronic disease. It centers on addressing modifiable behaviors and social determinants of health that drive the majority of morbidity and mortality worldwide.
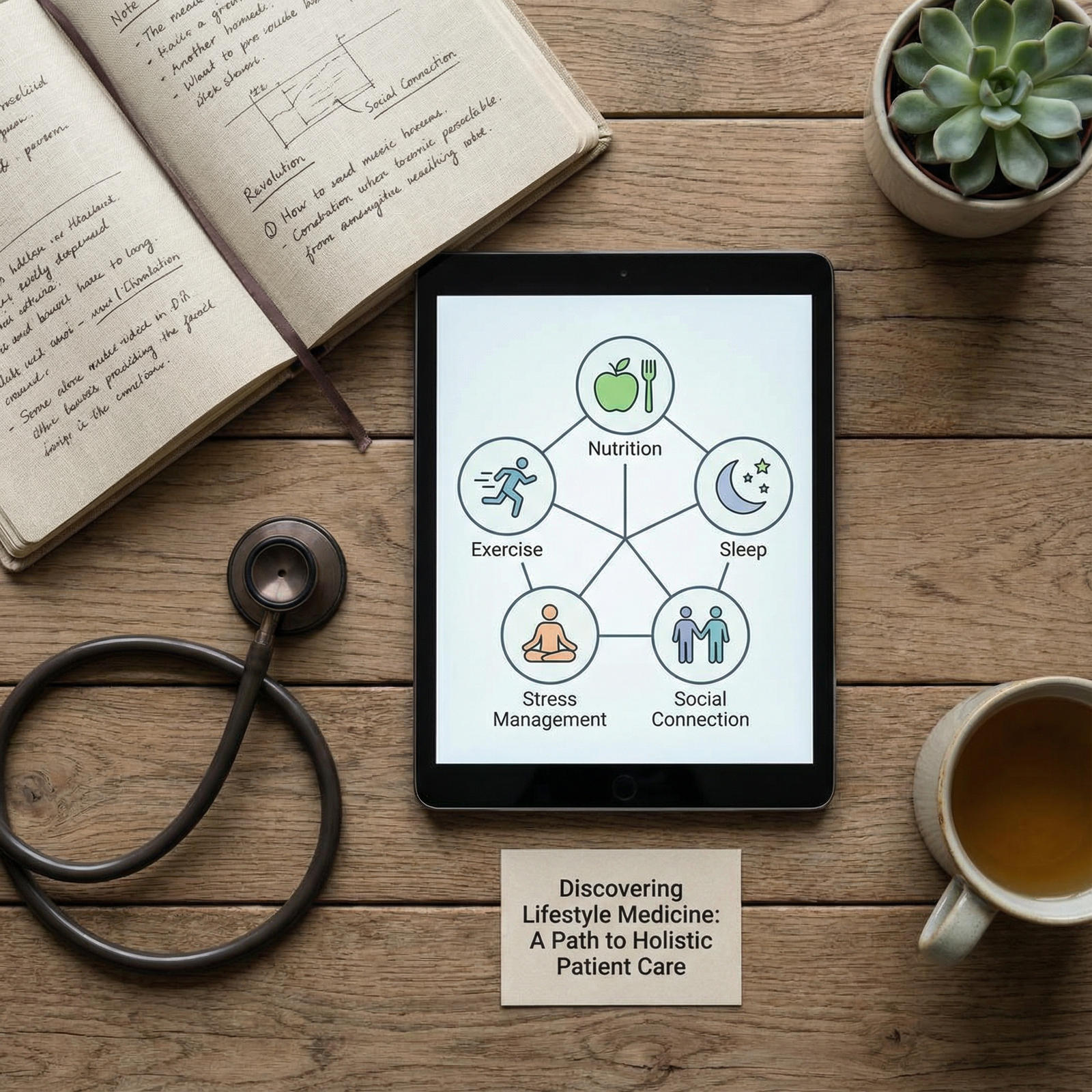
Core Pillars of Lifestyle Medicine
Most frameworks highlight six foundational domains:
- Nutrition
- Physical activity
- Sleep health
- Stress management and mental well-being
- Avoidance of risky substances
- Healthy relationships and social connection
Let’s briefly expand each:
Nutrition: Food as a Therapeutic Tool
Lifestyle medicine emphasizes a nutrition pattern rich in:
- Whole, minimally processed foods
- Vegetables, fruits, whole grains, legumes, nuts, and seeds
- Healthy fats (e.g., olive oil, avocado, nuts, fatty fish)
- Limited added sugars, refined grains, and ultra-processed foods
For example:
- Patients with prediabetes may see A1c reductions by adopting a predominantly plant-based diet.
- Hypertensive patients often improve blood pressure with DASH- or Mediterranean-style eating patterns, sometimes reducing medication burden.
As a trainee, you might not practice as a registered dietitian, but understanding basic nutritional counseling and knowing when to refer is central to lifestyle medicine.
Physical Activity: Movement as Medicine
Exercise prescriptions are as vital as pharmacologic ones. Typical goals:
- Aerobic activity: ~150–300 minutes/week of moderate intensity or 75–150 minutes/week of vigorous intensity
- Strength training: At least 2 days/week involving major muscle groups
- Movement throughout the day: Reducing sedentary time (e.g., standing/walking breaks during long charting sessions)
Practically, a 10-minute walk after meals for a patient with insulin resistance, or tailored strength exercises for an older adult with frailty, can be as impactful as medication adjustments.
Sleep: The Overlooked Vital Sign
Sleep is foundational to metabolic, cardiovascular, and mental health. Lifestyle medicine emphasizes:
- Consistent sleep-wake times
- Screen-free wind-down periods before bed
- Sleep-conducive environments (quiet, dark, cool)
- Screening for sleep disorders like sleep apnea or insomnia
For residents, applying sleep hygiene to your own life—even in modified form—is crucial for physician well-being and resilience.
Stress Management and Mental Well-Being
Chronic stress contributes to hypertension, depression, anxiety, and cardiovascular disease. Lifestyle medicine includes:
- Mindfulness practices
- Cognitive-behavioral strategies
- Breathing techniques
- Yoga, tai chi, or other mind–body exercises
- Behavioral activation and positive psychology frameworks
Importantly, stress management is not just advice for patients—it’s a survival skill for clinicians navigating training and early practice.
Avoiding Harmful Substances
Lifestyle medicine integrates classic preventive care:
- Tobacco cessation and nicotine dependence treatment
- Reducing harmful alcohol use
- Counseling on vaping, recreational drug use, and prescription misuse
These interventions are woven into every visit rather than treated as separate or secondary concerns.
Social Connection and Purpose
Evidence increasingly supports that social isolation, lack of purpose, and loneliness are major health risks. Lifestyle medicine approaches may include:
- Encouraging participation in community groups, volunteer work, or group classes
- Exploring meaning, values, and purpose in patients’ lives
- Connecting patients with peer support or group medical visits
This is at the heart of holistic health—recognizing patients as whole people, not just diagnoses.
Why Lifestyle Medicine Appeals to Physicians and Trainees
For residents and medical students, lifestyle medicine intersects powerfully with career satisfaction, work-life balance, and long-term sustainability in practice.

1. Work-Life Balance and Physician Well-Being
Many physicians are seeking not just a specialty, but a career that allows them to thrive as whole people. Lifestyle medicine can support that in several ways:
- Visit structure: Many lifestyle-focused practices build in longer visits or group sessions, allowing more meaningful interactions and less “assembly-line” care.
- Shared responsibility: Because patient empowerment is central, patients share ownership of health outcomes, reducing the feeling that everything depends solely on the clinician.
- Alignment with personal values: Physicians who value fitness, nutrition, and mental health often find deep congruence between how they live and how they practice.
For residents, integrating lifestyle medicine concepts early can shape how you approach your schedule, boundaries, and self-care. Even within demanding specialties, you can:
- Model realistic wellness strategies (e.g., micro-workouts, planning meals, brief mindfulness on call).
- Advocate for more prevention-focused workflows in your teams.
- Incorporate lifestyle discussions into routine visits rather than as optional add-ons.
2. Deeply Patient-Centered and Relationship-Focused Care
Lifestyle medicine naturally supports patient-centered care:
- Collaborative goal setting: Instead of dictating a plan, you co-create realistic changes with the patient.
- Narrative medicine overlap: Understanding a patient’s life story—work, family, culture, barriers—directly informs their lifestyle plan.
- Motivational interviewing: Techniques like open-ended questions, reflective listening, and affirmation enhance adherence and respect autonomy.
This stronger therapeutic alliance can transform what it feels like to practice medicine. Many lifestyle medicine physicians report:
- Greater satisfaction from seeing meaningful, long-term change.
- Fewer adversarial conversations about medications and more teamwork around shared goals.
- A sense of impact beyond episodic, problem-based visits.
3. Diverse and Flexible Practice Opportunities
Lifestyle medicine is not a single specialty; it’s a lens you can apply to numerous practice settings and lifestyle-friendly specialties:
- Primary care (IM/FM/Pediatrics): Longitudinal relationships are ideal for preventive care and habit change.
- Endocrinology and cardiology: Lifestyle interventions are core to managing diabetes, dyslipidemia, hypertension, and CAD.
- PM&R and sports medicine: Exercise prescriptions and functional restoration overlap strongly with lifestyle medicine principles.
- Psychiatry: Nutrition, sleep, exercise, and mindfulness are powerful adjuncts to psychopharmacology.
You can adapt your practice:
- Traditional clinic visits with lifestyle integration
- Group medical visits or shared appointments
- Corporate or occupational health programs
- Telehealth lifestyle coaching or virtual group programs
- Concierge or direct primary care models that emphasize preventive care and holistic health
For trainees, an elective or scholarly project in lifestyle medicine can strengthen residency applications, particularly if you’re aiming for specialties known for a lifestyle-friendly culture.
4. Intellectual Engagement, Innovation, and Research Opportunities
Lifestyle medicine offers rich areas for academic exploration:
- Comparative effectiveness of diet patterns or exercise prescriptions
- Health equity and access to healthy food and safe spaces for exercise
- Behavior change science and digital tools (apps, wearables, AI coaching)
- Longitudinal outcomes of lifestyle group visits versus usual care
Residents can:
- Design QI projects (e.g., integrating physical activity vital signs into clinic notes).
- Develop patient education resources.
- Partner with dietitians, behavioral health specialists, or physical therapists to study integrated care models.
This keeps clinical practice intellectually stimulating and positions you at the forefront of evolving care models.
Why Lifestyle Medicine Resonates Deeply with Patients
Lifestyle medicine’s appeal to patients goes beyond “eat better and exercise more.” It touches autonomy, identity, finances, and long-term quality of life.
1. Patient Empowerment and Shared Decision-Making
Patients increasingly want to be active participants, not passive recipients of care. Lifestyle medicine explicitly fosters:
- Education: Patients learn the “why” behind their conditions and treatments.
- Skills: They practice label reading, meal planning, stress techniques, or building activity into daily life.
- Agency: They experience direct control over their trajectory, which can be motivating and protective against hopelessness.
For example, a patient with newly diagnosed hypertension may feel helpless at first. But when you teach them how specific changes—such as sodium reduction, weight loss, and daily walking—can reduce or even eliminate their medication, they often feel more hopeful and engaged.
2. A Truly Holistic Health Vision
Lifestyle medicine explicitly addresses the whole person:
- Physical health (metabolic, cardiovascular, musculoskeletal)
- Mental health (depression, anxiety, burnout)
- Emotional well-being (resilience, coping, meaning)
- Relationships and social support
- Work and environment
Patients who feel fragmented by multiple specialists often find this integrative approach more coherent and aligned with their experience of illness.
3. Preventive Care and Long-Term Risk Reduction
Lifestyle medicine makes preventive care tangible and personalized:
- Patients at risk of type 2 diabetes may join structured programs focused on weight management, physical activity, and nutrition.
- People with strong family histories of heart disease can take proactive steps decades before a cardiac event.
- Survivors of cancer can adopt lifestyle changes to reduce risk of recurrence and improve function and fatigue.
Importantly, this approach emphasizes sustainability—small, consistent habits over time instead of drastic, short-lived changes.
4. Reduced Healthcare Costs and Treatment Burden
For many patients, lifestyle medicine can:
- Delay or reduce the need for expensive medications
- Lower likelihood of hospitalization or invasive procedures
- Decrease indirect costs (time off work, caregiving burdens, transportation)
For instance, a patient with well-controlled diabetes through intensive lifestyle modification may need fewer medications, fewer specialist visits, and fewer lab tests—an enormous relief both financially and emotionally.
Lifestyle Medicine in Action: Practical Clinical Scenarios
It’s helpful to visualize how lifestyle medicine looks in daily practice. Here are expanded, realistic scenarios you might encounter as a resident or early-career physician.
1. Nutrition Intervention for Metabolic Disease
Scenario: A 52-year-old with obesity, type 2 diabetes (A1c 8.5%), and fatty liver disease.
Lifestyle medicine approach:
Take a detailed dietary history (schedule, budget, cooking skills, cultural foods).
Provide education on:
- Swapping sugar-sweetened beverages for water or unsweetened tea
- Increasing non-starchy vegetables and fiber-rich foods
- Choosing whole grains over refined grains
Set one or two manageable goals:
- “Replace soda with water 5 days/week.”
- “Add one serving of vegetables to lunch and dinner.”
Partner with a dietitian for a more comprehensive plan.
Follow-up in 4–6 weeks focusing on what worked, what didn’t, and adjusting accordingly.
Over several months, you might see weight loss, improved A1c, and better liver enzymes—with potential to taper medications over time.
2. Movement Prescription for Chronic Pain
Scenario: A 60-year-old with chronic low back pain and deconditioning, fearful of exercise.
Lifestyle medicine approach:
Validate the pain and address fear of movement.
Collaborate with PT to design a graded activity program:
- Begin with 5–10 minutes of walking daily.
- Add core strengthening and flexibility exercises several times per week.
- Incorporate posture, ergonomics, and body mechanics education.
Introduce mind–body practices (e.g., yoga, tai chi, breathing exercises) to address both physical and emotional aspects of pain.
Reassure that mild soreness may occur but distinguish it from harmful pain.
Over time, improved function, decreased reliance on opioids or NSAIDs, and enhanced quality of life are common outcomes.
3. Stress Management for Anxiety and Sleep Problems
Scenario: A 35-year-old resident with insomnia, palpitations, and work-related anxiety.
Lifestyle medicine approach:
Screen for depression, anxiety disorders, and burnout.
Collaboratively plan:
- Brief nightly wind-down routine (screen-free 30–60 minutes).
- 5–10 minutes/day of guided mindfulness (apps or brief exercises between patients).
- Caffeine cutoff time and moderate alcohol use.
- Scheduling “non-negotiable” micro-breaks during call shifts.
Integrate basic cognitive-behavioral strategies (e.g., journaling thoughts before bed, challenging catastrophic thinking).
Consider referring to CBT-I (cognitive behavioral therapy for insomnia) or counseling if symptoms are significant.
This example highlights how lifestyle medicine supports both patient and physician well-being—you can authentically share strategies you use yourself.
4. Building Community and Support
Scenario: A clinic with high rates of obesity, type 2 diabetes, and depression among patients.
Lifestyle medicine approach at the system level:
Develop group visits for:
- Diabetes self-management
- Weight management
- Stress reduction and mindfulness
Include interdisciplinary team members: dietitian, behavioral health, pharmacist, physical therapist.
Foster peer support: patients share challenges and successes, reducing isolation.
Connect patients with community resources (walking groups, cooking classes, faith-based health programs).
These support communities create accountability and sustained motivation, often with lower clinician burden per patient due to shared visits.
Integrating Lifestyle Medicine into Your Training and Career
Lifestyle medicine is especially relevant if you’re exploring specialties known to be lifestyle-friendly, but it can add value in any field.
During Medical School
- Seek electives or rotations in lifestyle, integrative, or preventive medicine clinics.
- Join or help establish a lifestyle medicine or wellness interest group.
- Practice taking lifestyle-focused histories in OSCEs and clinical rotations.
- Start small personal wellness experiments (e.g., 10-minute daily walk) to empathize with patient behavior change.
During Residency
- Incorporate lifestyle questions into your standard H&P (diet pattern, physical activity, sleep, stress).
- Use every chronic disease follow-up as an opportunity for 1–2 targeted lifestyle goals.
- Develop handouts or EHR templates to streamline counseling.
- Consider certification in lifestyle medicine (e.g., American Board of Lifestyle Medicine) if available and relevant to your specialty.
Early Career and Beyond
- Decide how prominently lifestyle medicine will feature in your practice model.
- Advocate for system-level changes—longer visits, group appointments, team-based care.
- Continue your own growth in nutrition, motivational interviewing, and behavior change science.
Lifestyle medicine not only improves patient outcomes—it can sustain your sense of purpose and help protect against burnout.
FAQ: Lifestyle Medicine for Patients and Physicians
What is lifestyle medicine in simple terms?
Lifestyle medicine is the use of evidence-based lifestyle changes—such as improving diet, increasing physical activity, sleeping better, managing stress, avoiding harmful substances, and strengthening social connections—to prevent, treat, and sometimes reverse chronic disease. It does not replace necessary medications or procedures, but it often reduces dependence on them and addresses root causes rather than only symptoms.
How is lifestyle medicine different from traditional preventive care?
Traditional preventive care often focuses on screenings, vaccines, and risk factor checks (e.g., blood pressure, cholesterol). Lifestyle medicine goes a step further by actively treating the behavior and environmental drivers of disease. It emphasizes:
- Structured nutrition and exercise prescriptions
- Behavior change strategies (e.g., motivational interviewing)
- Ongoing coaching and follow-up
- Group visits and community-based interventions
In short, preventive care identifies risk; lifestyle medicine is designed to actively change it.
Why are more physicians and residents interested in lifestyle medicine?
Many physicians are drawn to lifestyle medicine because it:
- Aligns with their personal values around holistic health and wellness
- Supports more meaningful relationships with patients
- Can be integrated into many lifestyle-friendly specialties
- Offers diverse practice options, including telehealth, group visits, and corporate wellness
- May improve physician well-being by reducing the sense of futility and burnout associated with purely reactive care
For residents, early exposure to lifestyle medicine can shape a more fulfilling, sustainable career trajectory.
Can lifestyle medicine really reverse chronic diseases?
In some cases, yes—particularly for conditions like early type 2 diabetes, metabolic syndrome, and mild hypertension. Intensive lifestyle changes can:
- Normalize or significantly improve blood glucose and A1c
- Reduce or eliminate medications for some patients
- Improve blood pressure, cholesterol, and inflammatory markers
Not every disease can be fully reversed, but lifestyle medicine often improves function, reduces symptom burden, slows progression, and enhances quality of life—even in advanced conditions.
How can I start incorporating lifestyle medicine into my practice or training right now?
You can begin with small, practical steps:
- Add 2–3 lifestyle questions (diet, activity, sleep) to every routine visit.
- Use brief motivational interviewing techniques to set one realistic goal per visit.
- Create or use existing handouts and reputable online resources to support patient education.
- Partner with dietitians, behavioral health, or physical therapists where available.
- Model behavior change yourself—patients often respond well when physicians share their own realistic wellness strategies.
Over time, these incremental changes can transform both your patients’ outcomes and your own experience of practicing medicine.
By elevating lifestyle medicine within your clinical toolkit, you are aligning with the future of healthcare: a system that values prevention, holistic health, patient empowerment, and physician well-being as much as it values technology and pharmacology. For residents seeking both meaningful work and a sustainable life outside the hospital, lifestyle medicine offers a compelling, evidence-based path toward achieving that balance.






















