
The most common weakness in premed applications is not GPA or MCAT—it is lopsided, shallow, or late clinical experience.
You can have a 520 MCAT and a 3.9 GPA and still get screened out because your clinical exposure does not show that you understand, or can handle, real patient care. The good news: this is fixable, even if you are close to applying. The bad news: you must fix it intentionally, not by randomly adding more hours.
This guide gives you a stepwise repair protocol for uneven clinical experience before you apply MD or DO.
Step 1: Diagnose Your Clinical Experience Problem Precisely
“Uneven clinical experience” can mean very different things. You cannot fix what you have not defined.
Start by categorizing your current experience across four axes:
(See also: Reapplying to Med School: A Systematic Audit and Repair Checklist for more details.)
- Depth – How involved are you with actual patient care?
- Breadth – How many different clinical environments and populations have you seen?
- Consistency – Are your activities sustained or just short bursts?
- Recency – Are you still clinically active now?
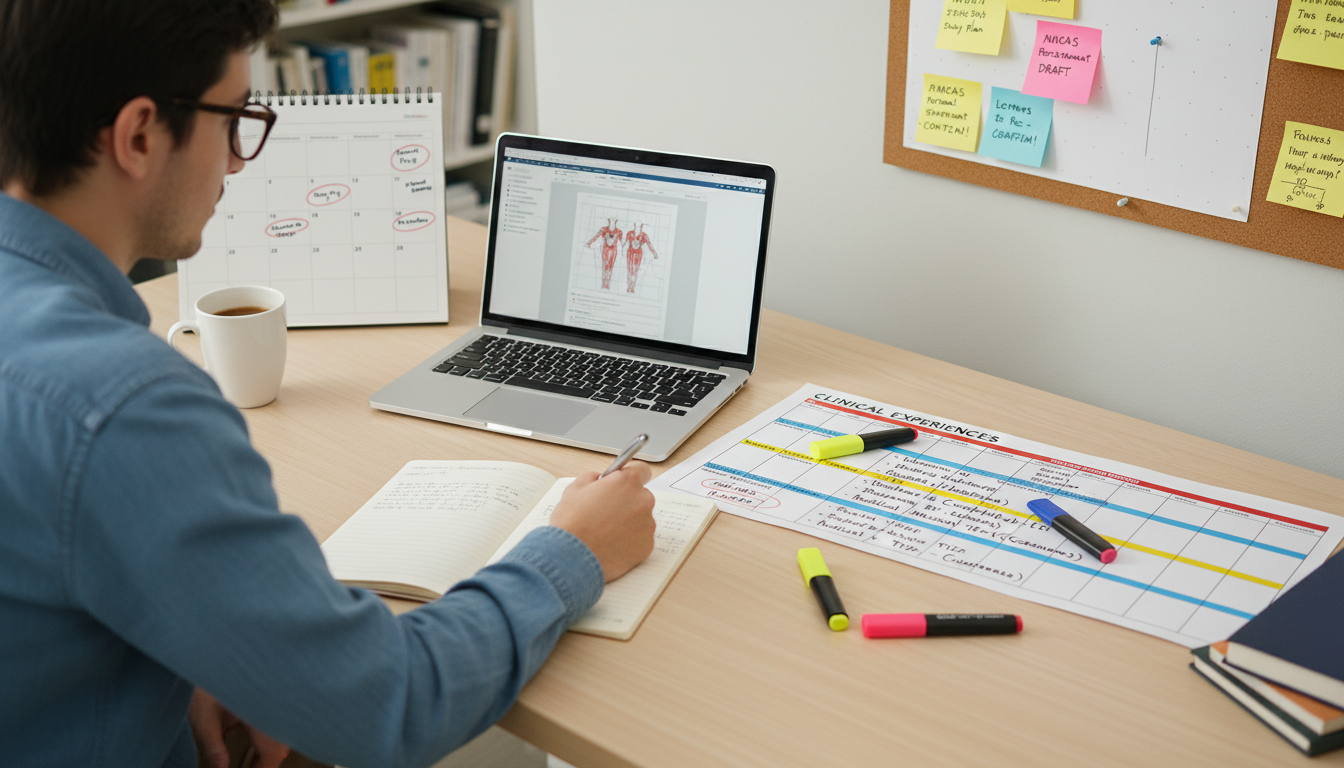
Create a simple one-page inventory. Use a table like this:
| Activity | Role | Setting | Start–End Dates | Total Hours | Patient Contact Type |
|---|---|---|---|---|---|
| Hospital volunteer, front desk | Volunteer | Academic hospital | 01/2023 – 12/2023 | 80 | Minimal, indirect |
| ER scribe | Paid job | Community ED | 05/2024 – Present | 120 | Direct, observed only |
| Free clinic translator | Volunteer | Free clinic | 02/2024 – Present | 40 | Direct, conversational |
Now identify which problem(s) you actually have:
- Problem A – Low total hours
- Less than ~75–100 hours of meaningful clinical exposure by the time you apply.
- Problem B – All passive / observational
- Shadowing only, or mostly sitting at a desk away from patients.
- Problem C – All in one setting or population
- Only pediatrics, only orthopedics, or only telehealth scribes.
- Problem D – Gaps or “bursts” of experience
- 200 hours over one summer, then nothing for a year.
- Problem E – No current clinical activity
- Nothing active within the last 6–9 months at the time of application.
- Problem F – Looks transactional or last-minute
- Suddenly 150+ hours all within 3–4 months before submission.
Be ruthless. Label your application honestly. For many premeds, two or three of these apply at once.
Your next steps will differ based on this diagnosis.
Step 2: Establish Target Benchmarks (MD vs DO Realities)
You do not need thousands of hours, but you do need enough of the right kind of exposure to show informed commitment.
General benchmarks (not strict cutoffs):
MD programs:
- Clinical exposure: 100–250+ hours total.
- At least 50–75 hours should be direct, in-person patient interaction.
- Shadowing: 20–60 hours across 2–3 specialties is usually sufficient.
- Timeline: Ongoing involvement over at least 6–12 months.
- Clinical exposure: 100–250+ hours total.
DO programs:
- Clinical exposure: 150–300+ hours total is often advantageous.
- Shadowing: 40–80 hours, including at least 1 DO physician (many schools strongly prefer or require this).
- Timeline: Same principle—sustained, recent clinical involvement.
If you are significantly below these numbers, you have a structural issue.
If you are near or above these numbers but still feel weak, your problem likely lies in quality, diversity, or narrative, not raw hours.
Step 3: Identify Your Primary Gap Type and Fix Strategy
Use this quick mapping:
- If you have <75 total clinical hours → You have a quantity and narrative crisis.
- If you have 150+ hours but mostly shadowing / scribes not interacting with patients → You have a depth problem.
- If all experience is >1 year old → You have a recency and commitment problem.
- If your hours clustered into one short period → You have a consistency and motivation problem in the eyes of committees.
- If all your work is in one narrow specialty or setting → You risk an exposure bias problem (do you really understand medicine beyond that niche?).
The fix for each is different. You will waste time if you treat them the same.
Step 4: Fast-Track Clinical Depth: Move From Observer To Participant
Admissions committees are not impressed by proximity alone. They care about whether you have been directly involved with patients in a way that exposes you to:
- Suffering and uncertainty
- Communication challenges
- Health system constraints
- Emotional fatigue
To fix a depth problem, prioritize roles where you do something for or with patients, even if the tasks are basic.
High-Impact Direct Clinical Roles (Often Obtainable Within Weeks)
Certified Nursing Assistant (CNA)
- Settings: Nursing homes, rehab centers, hospitals.
- Typical tasks: Vital signs, bathing, feeding, mobility assistance, toileting.
- Pros:
- Extremely direct care.
- Shows comfort with bodily fluids, physical labor, and vulnerable patients.
- Fix strategy:
- Enroll in a CNA course (4–10 weeks in many states).
- Aim for part-time shifts (8–16 hours per week) for 3–6+ months.
Medical Assistant (MA)
- Settings: Outpatient clinics, urgent care, specialty offices.
- Tasks: Rooming patients, vitals, EKGs, injections, chart prep.
- Caution: Many practices require prior training or experience.
- Fix strategy:
- Look for “MA trainee” or “on-the-job training” roles in smaller private practices or community clinics.
- Leverage any previous basic clinical training (EMT, phlebotomy).
Emergency Medical Technician (EMT)
- Settings: Ambulance services, ED tech roles.
- Tasks: Basic life support, transport, patient assessments.
- Good if:
- You have 6–12 months before applying.
- Fix strategy:
- EMT-B course (often 3–4 months part-time).
- Commit to at least one full application cycle of work if possible.
Hospice Volunteer
- Settings: Home hospice, inpatient hospice centers.
- Tasks: Companionship, caregiver support, light tasks, presence at end of life.
- Pros:
- Deep exposure to mortality, family dynamics, emotional conversations.
- Fix strategy:
- Many hospices offer structured volunteer programs with training in 4–8 weeks.
- Target 2–4 hours per week consistently.
Free Clinic or Student-Run Clinic Volunteer
- Settings: Underserved communities, urban clinics, mobile clinics.
- Tasks: Intake, translation, patient navigation, health education.
- Pros:
- Direct interaction and real-world barriers to care.
- Fix strategy:
- If your university has a student-run clinic, join now, do not wait.
- Aim to take on progressively more responsibility (intake lead, coordinator).
If you are within 6–9 months of applying, prioritize roles that:
- You can start within 4–6 weeks.
- Offer predictable weekly hours to build a narrative of consistency.
Do not rely on:
- Occasional “clinical mission trips” that last 1–2 weeks.
- Sporadic volunteer events labeled “health fair” with minimal patient interaction.
- Remote scribe work as your only direct experience.
Those can supplement. They cannot substitute.
Step 5: Fix Consistency and Recency: Build a Visible Clinical Timeline
Committees do not just ask “how many hours?” They ask:
- Are you involved now?
- Have you stayed involved over time?
- Do your activities show that medicine is a central priority, not a short-term project?
Build a Clinical Continuity Plan
Use this structure:
Pick 1–2 anchor activities that you will keep active from now until application:
- Example:
- Hospital volunteer (4 hours/week, weekends).
- Free clinic translator (2–3 hours/week, one weekday evening).
- Example:
Add 1 role with high emotional intensity if lacking:
- Example: Hospice volunteer, inpatient psych unit volunteer, ED volunteer with patient interaction.
Document clearly on your timeline:
- Start dates and “Present”.
- Increasing responsibility or leadership, if any.
Your goal: When an admissions reader looks at your primary application, they should see at least one clinically related entry marked as ongoing (“MM/YYYY – Present”).
If you already have:
- 150–200 hours from previous years but nothing recent, then:
- Solution: Add 50–100 hours of current clinical work over 4–6 months before you apply.
- You are not trying to erase your past gap. You are showing that you are back in the clinical world with intention.
If you are applying this cycle and currently have:
- Very few clinical hours but several months until submission (say, January to May):
- Commit to 8–10 hours per week of high-yield clinical volunteering.
- That can produce 120–160 hours of experience by June, which changes your narrative from “almost no exposure” to “rapid, but now substantive and clearly ongoing” experience.
Step 6: Rebalance Shadowing The Smart Way (Especially For DO)
Shadowing is overrated when overdone and disastrous when absent.
You need enough to:
- Show you understand physician workflow and decision-making.
- Demonstrate you have observed the real daily grind, not just TV-drama medicine.
- Satisfy DO-specific expectations.
Target Shadowing Distribution
- Total: 30–80 hours is usually enough.
- MD-only applicant:
- 2–3 physicians, 1 primary care strongly recommended.
- 10–30 hours per physician.
- MD + DO applicant:
- At least 1 DO physician.
- 20–40 hours with that DO, especially in primary care, family med, or IM.
Fix Strategy For Weak Or Absent Shadowing
If you currently have:
- 0 shadowing hours, start with:
- Reach out via:
- Your PCP.
- Family or friend connections.
- Hospital volunteer office asking about shadowing channels.
- Aim for:
- 4–6 half-days (4–6 hours each) with your first physician.
- Then branch to:
- One different specialty or setting for 10–20 hours.
- Reach out via:
If you are DO-focused but have:
- No DO shadowing:
- Use state osteopathic association websites to locate DOs.
- Email template basics:
- Brief intro (major, year, school).
- One sentence about your interest in osteopathic medicine.
- Specific ask: “Would you be open to me shadowing you for X half-days over Y weeks?”
- Consider spreading 20–30 hours over a 1–2 month window.
Remember: Shadowing does not need to be long-term, but it must be realistic and recent enough that your reflections about it sound authentic in your essays and interviews.

Step 7: Strengthen Your Narrative: Turn Uneven Experience Into A Coherent Story
You cannot pretend your past inconsistency did not happen. You can, however, frame it with maturity and growth.
Admissions committees are asking:
- Do you now clearly understand what physicians actually do?
- Have you confronted the harder side of medicine and still want in?
- Can you explain your choices without sounding defensive?
Common Narrative Problems And Repairs
Problem: “All my hours came from one summer and then nothing.”
- Weak version:
- “I volunteered in the ED for one summer and really enjoyed it, but I became busy with school and research.”
- Stronger repair:
- Add current clinical work (e.g., free clinic, hospice).
- Reflect in your personal statement or activity description:
- Briefly acknowledge the earlier limitation.
- Emphasize what you learned from returning to clinical work.
- Example angle:
- “I initially treated clinical volunteering as something to ‘fit in’ around my schedule. As I took on more responsibility in research, I realized how distant I had become from patients. Returning to the free clinic this year has forced me to balance both worlds and reminded me that the human stories behind the data are what draw me to medicine.”
- Weak version:
Problem: “I have 200 hours of scribing but barely spoke to patients.”
- You must show you still gained:
- Insight into diagnostic reasoning.
- Exposure to a wide range of patient conditions.
- Fix:
- Add at least one direct-contact role, even if for fewer hours (e.g., hospital or hospice volunteer).
- In your activity descriptions:
- Highlight specific patient encounters you observed.
- Pair it with newer direct-contact stories.
- You must show you still gained:
Problem: “My experience is late and looks rushed.”
- If you are starting heavy clinical involvement within 6–9 months of application:
- Do not oversell the duration. Focus on:
- Intensity.
- Specific challenges.
- Concrete lessons.
- Consider briefly explaining your late pivot if there was a real reason (caring for family, financial constraints, COVID limitations), but never blame circumstances alone.
- Do not oversell the duration. Focus on:
- If you are starting heavy clinical involvement within 6–9 months of application:
Use Activity Descriptions To Show Depth, Not Just Duties
For each major clinical activity, structure your description (in AMCAS/AACOMAS) like this:
- 1–2 lines: What you actually did (duties).
- 1–2 lines: What you saw that challenged or changed you.
- 1–2 lines: How this shaped your understanding of being a physician.
Example (hospital volunteer, 175 characters truncated style):
- “Volunteered on medical-surgical floors, delivering meals, assisting with transport, and sitting with patients awaiting tests. Witnessed how small acts—warming blankets, listening to a confused patient—significantly changed their perception of care. Learned that presence, not just procedures, defines patients’ experience of hospitalization.”
Step 8: Decide Whether To Delay Your Application
Sometimes the most powerful fix is not creative scheduling. It is waiting one cycle.
This decision should be strategic, not emotional.
You Should Seriously Consider Delaying If:
- You have <50 clinical hours and <6 months until submission.
- You have no direct patient contact of substance.
- You are targeting highly competitive MD programs with no meaningful clinical continuity.
- Your letters of recommendation will come mostly from:
- Non-clinical faculty.
- Supervisors who barely know your clinical work.
In those cases, a rushed application often leads to:
- Rejection or waitlist without clarity.
- Lost time and money.
- Needing to reapply with the “reapplicant” label, which raises the bar further.
What To Do With A Gap Year (Or Extra Year Pre-Application)
If you decide to delay, design a purposeful clinical-heavy year, not a random assortment of gigs.
Aim for:
- One full-time clinical role (CNA, MA, EMT, scribe with real exposure, medical interpreter).
- One consistent volunteer activity that addresses:
- Underserved populations.
- Hospice/end-of-life.
- Chronic disease management.
Example year:
- 32–36 hours/week as a CNA in a skilled nursing facility.
- 4 hours/week at a free clinic.
- 2–3 hours/week shadowing across 2–3 specialties over several months.
By the next cycle, your “uneven” experience becomes:
- A story of growth and correction.
- A portfolio showing:
- Direct care.
- Emotional resilience.
- Commitment through sustained work.
Step 9: Optimize Clinical Experience For MD vs DO Nuances
You do not need two totally different clinical portfolios. However, you should subtly tune them.
For MD-Focused Applicants
Emphasize:
- Breadth of settings (inpatient, outpatient).
- Exposure to complex decision-making (scribing, shadowing in IM, ED, surgery).
- Reflection on systems-level issues (access to care, health disparities).
Useful combinations:
- Scribe in ED or hospitalist service + free clinic volunteer.
- Hospital volunteer with patient contact + hospice volunteer.
For DO-Focused Or MD+DO Applicants
Ensure:
- At least one DO letter if your target schools prefer it.
- Clear engagement with primary care and community-based medicine.
Emphasize:
- Continuity of care.
- Whole-person, biopsychosocial understanding of patients.
- Any experiences in:
- Rural medicine.
- Underserved urban clinics.
- Rehabilitation, pain management, OMT clinics (if available).
The same volunteer role can be framed differently depending on emphasis:
- MD essay angle:
- How free clinic work exposed you to system inefficiencies and documentation burdens.
- DO essay angle:
- How that same free clinic work showed the impact of addressing social, emotional, and physical factors together.
Step 10: Create A 12-Week “Clinical Fix” Action Plan
To make this concrete, here is a model plan if you are 12–16 weeks from application and your clinical experience is weak or uneven.
Week 1–2: Rapid Assessment And Enrollment
- Audit your current hours and gaps using the four-axis method (depth, breadth, consistency, recency).
- Apply to:
- Hospital volunteer programs (look for short onboarding timelines).
- Free clinic or student-run clinic roles.
- Hospice volunteer programs.
- Begin outreach for 1–2 shadowing opportunities (1 MD, 1 DO if possible).
Week 3–4: Start Direct Patient Contact
- Begin at least one role with direct interaction:
- Free clinic intake.
- Hospital unit volunteer with patient visits.
- Hospice volunteer training if already accepted.
- Schedule:
- 1–2 shadowing days with your first physician.
- Log your hours meticulously from day one.
Week 5–8: Build Volume And Consistency
- Increase to 6–10 clinical hours/week between all roles.
- Distribute:
- 4–6 hours direct patient contact.
- 2–4 hours shadowing or other observational roles.
- Start a brief reflection journal after each shift:
- One case that stood out.
- One thing that surprised you.
- One thing that reinforced or challenged your view of medicine.
This journal becomes gold for your activity descriptions and secondary essays.
Week 9–12: Solidify Narrative And Prepare For Application
- Maintain clinical hours steadily.
- Draft activity descriptions that:
- Move beyond task lists.
- Highlight emotional and cognitive growth.
- If possible:
- Secure at least one letter of recommendation that reflects:
- Reliability.
- Empathy.
- Professionalism in clinical settings.
- Secure at least one letter of recommendation that reflects:
By the time you apply, you may not have massive hours, but you will have:
- A clear upward trajectory.
- Recent, active clinical involvement.
- Concrete stories that show why you belong in medicine.
Key Takeaways
- Fix the right problem, not just the visible one. Identify whether your clinical weakness is about depth, breadth, consistency, recency, or narrative—and then target that specifically.
- Prioritize real patient contact and continuity over inflated hour counts. A few hundred hours of hands-on, sustained experience beats scattered shadowing or one intense summer.
- When necessary, delay strategically rather than apply weakly. A focused year of clinical work can transform an uneven profile into a compelling, credible application for both MD and DO schools.






















