
Introduction: Why Note‑Taking Can Make or Break Your Medical School Experience
Medical school demands that you absorb, integrate, and apply an overwhelming volume of information—from molecular pathways and pharmacology to clinical reasoning and patient communication. Yet many students approach lectures and readings passively, transcribing everything without a strategy and then feeling lost when it’s time to review.
Effective Note-Taking Strategies are not just about writing faster; they are about thinking better. When you design how you capture information, you also shape how you understand, store, and retrieve it later. The right Study Techniques and Learning Methods can dramatically improve your retention, exam performance, and confidence on the wards.
This guide will walk you through high‑yield note-taking systems specifically adapted for medical education. You’ll learn how to choose the best approach for different types of content (e.g., pathways, guidelines, differentials), how to integrate digital tools, and how to turn notes into powerful Retention Strategies that work with, not against, your brain.
The Role of Note-Taking in Medical Education Success
Before choosing a method, it helps to understand what effective note-taking should accomplish for a medical student.
How Note-Taking Supercharges Learning
Deeper processing, better retention
Writing or actively organizing content forces you to decide what matters and how it fits with what you already know. This active processing creates stronger memory traces than passively listening or reading.Structured knowledge, not random facts
Medical curricula are dense and interconnected. Effective notes support schema building—organizing information into patterns (e.g., “all the causes of hypercalcemia” or “approach to chest pain”). This is how experts think and how you should train yourself to think.Efficient exam preparation
Well-designed notes become your personal “mini-textbooks” that you can quickly review before block exams, the USMLE/COMLEX, shelf exams, and OSCEs. Good notes reduce last‑minute chaos and allow targeted review of weak areas.Bridging preclinical to clinical
Thoughtful notes (especially on clinical pearls, patterns, and red flags) make it easier to connect preclinical science to patient care later. Adding examples from cases or simulated patients is an underrated but powerful Learning Method.
Principles of High-Quality Medical Notes
Regardless of the specific format you choose, your notes should aim to be:
Selective, not stenographic
Capture the most testable and clinically relevant points, not every word spoken.Organized for retrieval
Structure your notes so you can quickly find “antibiotic choice in pneumonia” or “features of nephrotic vs nephritic syndrome” without scrolling endlessly.Integrated with other tools
Your notes should feed into flashcards, question banks, and spaced repetition systems, not exist in isolation.Regularly reviewed and refined
Notes are living documents. As your understanding deepens, returning to your notes to update, condense, or reorganize is a powerful Retention Strategy.
Core Note-Taking Methods for Medical Students
There is no single “best” method. The key is to choose a system that fits:
- the type of material
- the format of teaching (lecture, small group, clinical)
- and your personal learning style
Most successful students use a hybrid approach.
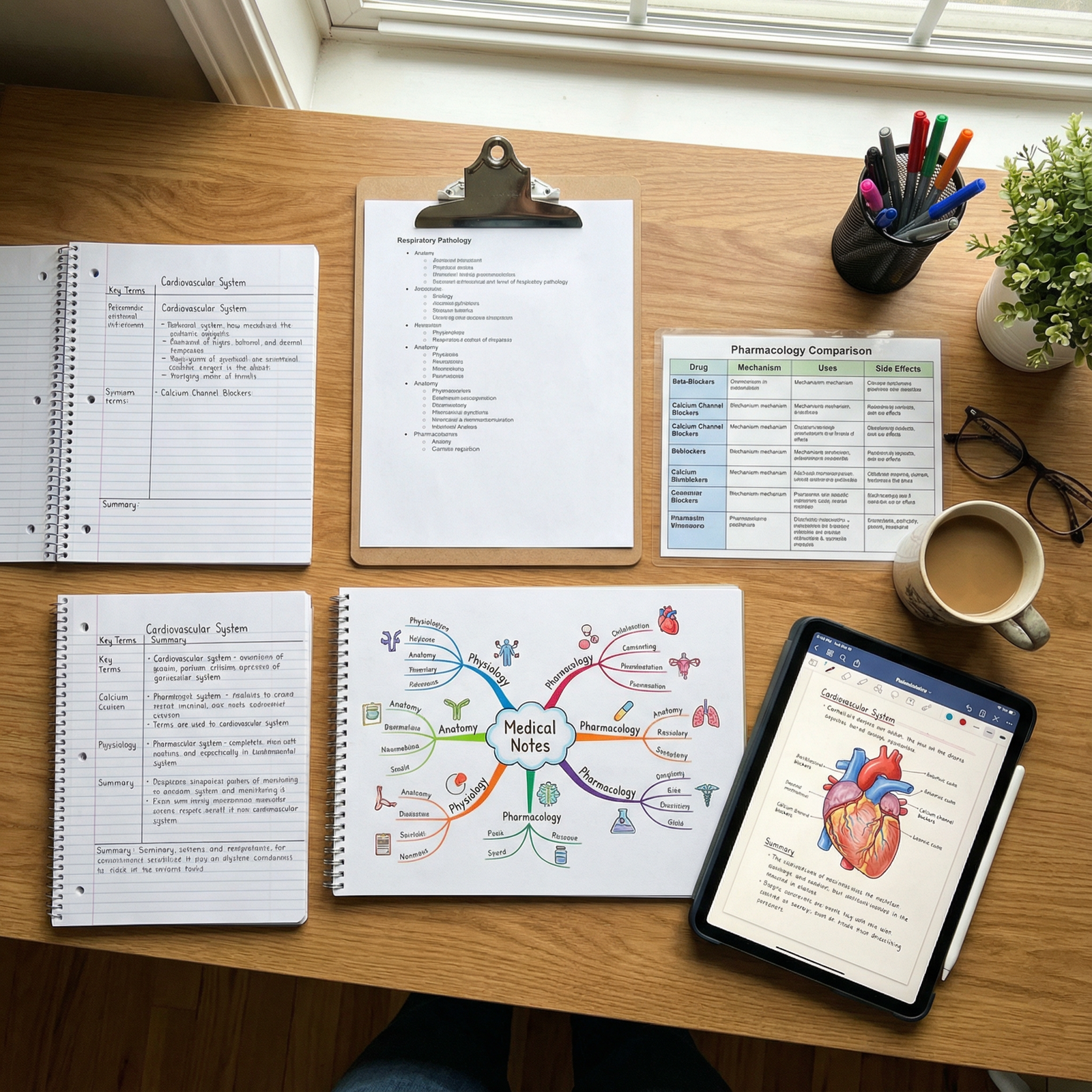
1. The Cornell Method: Structured Notes for Conceptual Clarity
The Cornell Method is a classic system that works especially well for lectures, case discussions, and readings where you need to capture explanations and relationships.
How the Cornell System Works
Divide your page (digital or paper) into three sections:
Cue Column (left, narrow):
- Key terms, questions, or prompts
- Example: “Pathophysiology of heart failure?” “Contraindications to beta-blockers?”
Note-Taking Area (right, wide):
- Main content from lecture/readings
- Bullet points, short phrases, diagrams, simple tables
Summary (bottom):
- 3–5 sentence summary of the page
- “Big picture” takeaways and most testable points
How to Apply Cornell in Medical School
During lecture:
- Use the right side for concise notes linked to each slide or topic.
- In real time, jot down only minimal cues in the left column.
Immediately after lecture (within 24 hours):
- Fill in the left column with questions that test the material.
- Example: “List the main causes of secondary hypertension.”
- Write a 3–5 line summary at the bottom focusing on mechanisms, patterns, and key rules.
For review:
- Cover the right side and quiz yourself using just the cue questions.
- Try to recall, then check your responses against your notes.
Why Cornell Works in Medical Education
- Promotes active recall and self-testing.
- Naturally prepares material for oral exams and clinical reasoning.
- Helps you quickly identify what is high-yield vs. extra detail.
2. Mind Mapping: Visualizing Complex Relationships
Medical knowledge is highly interconnected—systems, pathways, and feedback loops. Mind Mapping is an excellent Note-Taking Strategy for integrating and visualizing these relationships.
When Mind Maps Are Especially Useful
- Physiology and pathophysiology (e.g., RAAS system, coagulation cascade)
- Microbiology (organisms, virulence factors, treatments)
- Differential diagnoses (e.g., causes of jaundice, chest pain, anemia)
- Approaches or algorithms (e.g., workup of hyponatremia)
How to Create Effective Mind Maps
Central concept in the center
- Example: “Acute Kidney Injury (AKI)”
Main branches for major categories
- Prerenal, Intrinsic, Postrenal
- Under each: causes, pathophys, labs, treatment
Sub-branches for details
- Under “Intrinsic”: ATN, AIN, GN
- Under “ATN”: ischemic vs nephrotoxic, key drugs, urine findings
Use color, icons, and diagrams
- Color code: blue = pathophys, red = red flags, green = treatment
- Simple visual cues (e.g., a blocked pipe for obstruction)
Digital Mind Mapping Tools
- XMind, MindMeister, Coggle, or Notability/GoodNotes (drawing tools)
- Integrate screenshots from lecture slides or textbooks.
Benefits for Retention and Exams
Mind maps transform memorization into conceptual understanding, making it easier to:
- Tackle unfamiliar vignettes on exams
- Explain pathophysiology during rounds
- Build differential diagnoses logically
3. The Outline Method: Linear, High-Yield Capture
The Outline Method is ideal for structured, sequential content—like a lecture that follows textbook headings or guideline outlines.
How to Structure Outline Notes
Use hierarchical levels:
- I. Major topic
- A. Subtopic
- Detail
- a. Example or clinical pearl
- A. Subtopic
Example for “Asthma”:
- I. Definition and Epidemiology
- II. Pathophysiology
- A. Airway inflammation
- B. Bronchial hyperresponsiveness
- III. Clinical Features
- A. Symptoms
- B. Physical exam signs
- IV. Diagnosis
- A. Spirometry criteria
- B. Differential diagnoses
- V. Management
- A. Stepwise therapy
- B. Acute exacerbations protocol
Best Uses in Medical School
- Lectures with clear headings or learning objectives
- Reading from major review books (e.g., First Aid, BRS)
- Summarizing guidelines or protocols
- e.g., “Sepsis management,” “Stroke protocol,” “ACLS algorithm”
Why Outlining Works
- Creates a logical, test-like structure (mirrors how exam questions are built).
- Makes it easy to condense later into flashcards or summary sheets.
- Helpful for “big picture” plus fine details in one place.
4. Charting Method: Mastering Comparisons and Patterns
Some of the hardest content in medical education is comparative—distinguishing similar diseases, drug classes, or organisms. The Charting Method uses side-by-side tables to highlight these differences clearly.
Ideal Topics for Charting
- Pharmacology (drug classes, mechanisms, ADRs, indications)
- Hematology (types of anemias, leukemias, coagulopathies)
- Renal or liver diseases (e.g., nephritic vs nephrotic syndromes, hepatitis types)
- Microbiology (organism, reservoir, transmission, disease, treatment)
- Imaging choices and test characteristics (sensitivity, specificity)
Example Pharmacology Chart
| Drug Class | Drug Name | Mechanism of Action | Key Indications | Notable Side Effects | Contraindications |
|---|---|---|---|---|---|
| Beta Blockers | Metoprolol | Blocks beta-1 adrenergic receptors | HTN, angina, HF | Bradycardia, fatigue | Severe asthma, bradycardia |
| ACE Inhibitors | Lisinopril | Inhibits angiotensin-converting enzyme | HTN, HF, diabetic nephropathy | Cough, hyperkalemia, angioedema | Pregnancy, bilateral RAS |
Advantages of Chart-Based Note-Taking
- Supports pattern recognition, crucial for exams and clinical decisions.
- Easy to skim for last-minute review (“all the SLE drugs in one place”).
- Excellent source for generating targeted flashcards.
5. Digital Note-Taking Tools in Medical Education
Modern medical students often blend handwritten and digital notes. Used wisely, digital note-taking enhances organization, searchability, and integration with other Study Techniques.
Popular Digital Platforms
Microsoft OneNote
- Excellent for “notebooks” per system/course
- Flexible: text, images, freehand drawing, audio recording
Notion
- Combines notes, databases, and task tracking
- Great for integrating question logs, study schedules, and concept pages
Evernote
- Robust tagging, web clipping, and document organization
GoodNotes / Notability (iPad)
- Ideal for handwritten notes with stylus
- Mark up lecture PDFs, add diagrams and sketches
Best Practices for Digital Note-Taking
Use consistent structure
- e.g., Folders for “MSK,” “Cardio,” “Obs/Gyn,” or by blocks/semesters.
Tag for rapid retrieval
- Tags like “pharm,” “differential,” “imaging,” “OSCE,” “must-memorize.”
Embed images and diagrams
- Insert clinical images, radiology, or histology slides directly into notes with captions.
Sync across devices
- Ensure access on phone, tablet, and laptop for review during commutes or on the wards.
Handwritten vs Digital: Finding Your Balance
- Handwriting may improve encoding and understanding, especially for complex diagrams or pathways.
- Digital shines for organization, speed, templates, and search.
Many students:
- Handwrite during lecture or case discussions
- Then digitize, reorganize, or summarize into a digital “master note” later
Turning Notes into Learning: Active Recall & Spaced Repetition
Capturing information is only half the job. To truly transform your medical studies, your notes must feed into Retention Strategies that exploit how memory works.
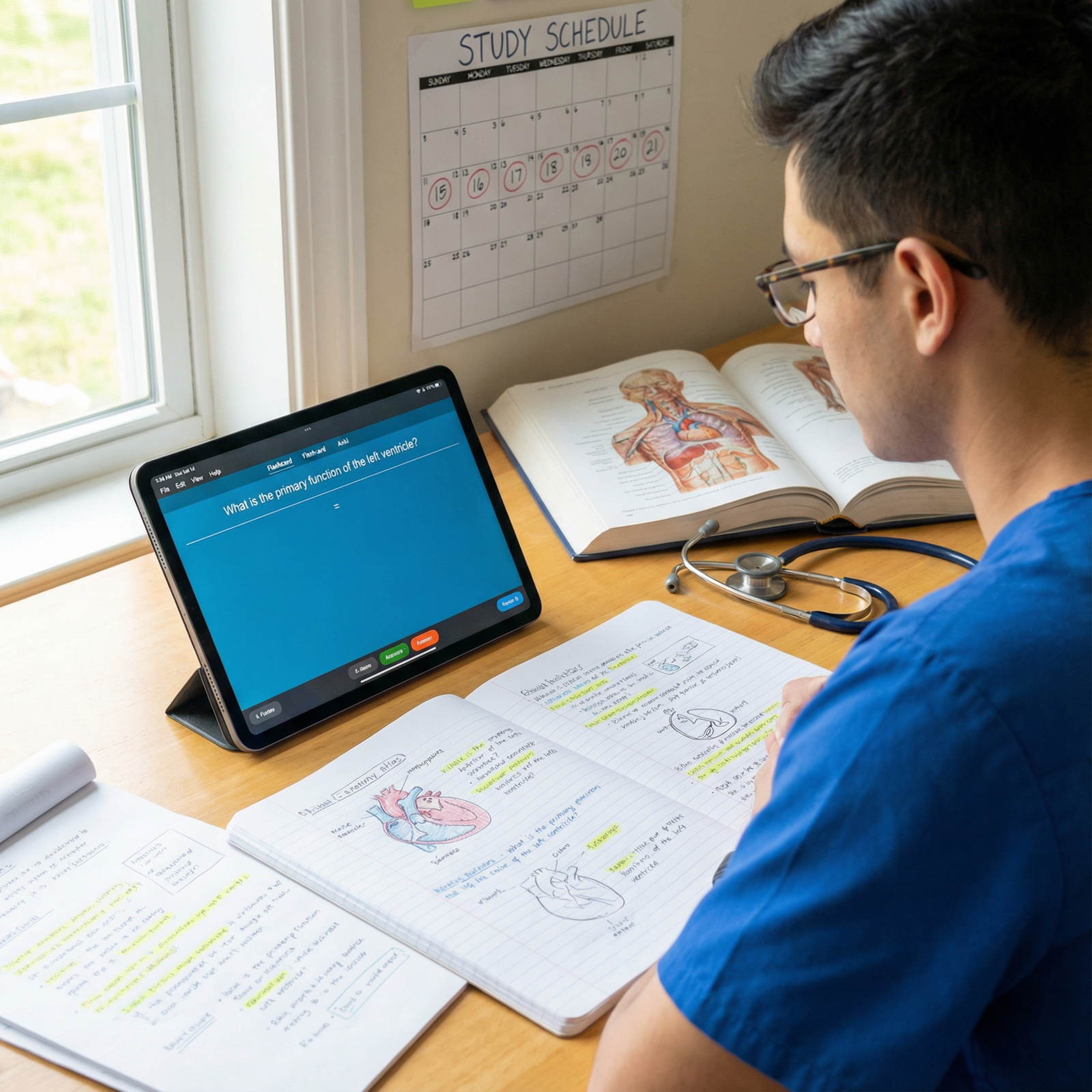
6. Active Recall: Test Yourself, Don’t Just Reread
Active recall means pulling information out of memory, not just looking at it. It is one of the most effective Learning Methods for long-term retention and exam success.
How to Build Active Recall into Your Notes
Convert headings into questions
- Instead of “Complications of MI” write “What are the major early and late complications of MI?”
Use the Cornell cue column
- Fill it with questions that force you to explain, list, and compare.
Cover-and-recall technique
- Hide the right side (or content area) of your notes and answer from memory.
Quick oral recall
- Explain the topic aloud as if summarizing to a patient, a peer, or a junior student.
7. Spaced Repetition: Review at the Right Time
Without review, even well-understood material fades. Spaced repetition schedules your reviews just before you’re likely to forget.
Implementing Spaced Repetition from Your Notes
Convert key facts into flashcards
- Tools like Anki, Quizlet, or Memrise
- Cards drawn directly from your notes: definitions, mechanisms, images, tables
Types of high-yield cards:
- One-fact cards: “First-line treatment for uncomplicated pyelonephritis?”
- Concept cards: “Explain the mechanism by which ACE inhibitors cause hyperkalemia.”
- Image cards: show an ECG or histology slide and ask for diagnosis or key findings.
Link back to notes
- Add a “source” tag or link to the note for deeper review when a card is hard.
Suggested review rhythm:
- Initial review within 24 hours
- Then at ~3 days, 7 days, 14+ days, guided by your app’s algorithm
This combination—note-taking → flashcards → spaced repetition—is one of the most powerful Retention Strategies in modern medical education.
Enhancing Your Notes: Color, Annotations, and Peer Teaching
8. Annotation and Color‑Coding for Clarity
Smart use of color and annotations helps you visually prioritize and connect information.
Practical Color-Coding System (Example)
- Red: Emergencies, red flags, life-threatening conditions
- Blue: Core concepts and mechanisms
- Green: Treatments, doses, and guidelines
- Purple: Clinical pearls or exam hints
- Orange: “Common pitfalls” or frequently confused concepts
Annotation Tips
Annotate lecture slides with:
- Clarifying comments from the lecturer
- Memory aids (“mnemonics” or analogies)
- Clinical examples (“Seen in 65-year-old smoker with weight loss”)
Mark recurring exam themes with symbols:
- ★ = high-yield
- ! = common mistake
- ? = unclear, to ask professor or look up later
These small tweaks improve scan-ability when you come back to your notes before exams or OSCEs.
9. Peer Teaching: Turn Notes into Teaching Tools
One of the most powerful Learning Methods is teaching others. When you teach, you must organize your thoughts, fill knowledge gaps, and anticipate questions.
How to Use Peer Teaching Strategically
Study groups
- Assign each person a topic (e.g., “nephrotic syndromes,” “TB drugs”)
- Use your notes to teach the group in 5–10 minutes
- Group members ask questions and add clinical scenarios
One-on-one teaching
- Explain a concept to a classmate who missed a lecture or struggled with the topic
- Teaching from your notes reveals what is unclear or incomplete
Micro-teaching sessions
- On the wards, after a patient encounter, take 2 minutes to teach a key concept (e.g., “approach to hyponatremia”) using mental notes or a small summary you keep in your phone.
Peer teaching solidifies knowledge at a deeper level—exactly the type you’ll need in clinical reasoning and board-style questions.
Putting It All Together: Building a Personal Note-Taking System
Every student’s optimal system looks different, but here is a sample integrated approach:
Example Weekly Workflow
Before lecture:
- Skim objectives, pre-read a short summary (e.g., review book chapter).
- Prepare a Cornell or outline template for that lecture.
During lecture:
- Use Cornell or Outline method to capture key points.
- Mark high-yield or confusing areas with symbols.
Within 24 hours:
- Clean up notes; add missing information from slides or textbook.
- Fill Cornell cue column with questions.
- Create tables or mind maps where comparisons are needed.
- Make flashcards from the most important facts.
Weekly review:
- Use active recall with your Cornell questions.
- Review flashcards using spaced repetition.
- Update mind maps and charts for integration.
Pre-exam:
- Focus on your most condensed materials: charts, mind maps, summary sheets.
- Add rapid-fire oral recall using your notes as prompts.
This system transforms notes from static documents into a dynamic learning engine that supports continuous growth throughout medical school and into residency.
FAQ: Note-Taking Strategies in Medical School
Q1: What is the single best note-taking method for medical students?
There is no universal “best” method. Most high-performing students use a hybrid system: Cornell or Outline for lectures, Mind Maps for complex relationships, and Charts for comparisons (especially in pharmacology and pathology). The best method is the one you consistently use and that integrates well with your flashcards, practice questions, and review schedule.
Q2: Should I focus on handwritten notes or go fully digital?
Both have advantages:
- Handwritten notes may improve initial understanding and are great for drawing diagrams and pathways.
- Digital notes excel at organization, searchability, and integration of images and links.
Many students take rough handwritten notes in class and later convert them into organized digital notes for long-term review. Experiment and choose the balance that keeps you efficient and engaged.
Q3: How often should I review my notes to maximize retention?
Aim for:
- First review: within 24 hours of the lecture or study session
- Follow-up reviews: at spaced intervals (e.g., days 3, 7, 14, and beyond), guided by a spaced repetition tool like Anki.
Short, frequent reviews using active recall (questions, flashcards, self-quizzing) are far more effective than long, infrequent rereads.
Q4: How can I avoid just copying slides and writing too much?
Before and during lecture:
- Focus on understanding, not transcribing.
- Paraphrase in your own words.
- Note only what adds beyond the slide: clarifications, examples, clinical pearls.
After lecture: - Condense your notes—combine points, remove redundancies, and highlight only what is high-yield or clinically important.
Q5: Can I integrate images and diagrams into my notes effectively?
Yes, and you should—especially in anatomy, pathology, radiology, and dermatology.
- Insert or draw labeled diagrams, flowcharts, and diagnostic algorithms.
- Use image-based flashcards (e.g., histology slides, ECGs, imaging).
- Add short captions explaining “what this image shows” and why it matters clinically.
Visuals significantly improve recognition and recall on exams and in clinical practice.
By designing an intentional note-taking system, you’re not just collecting information—you’re training your brain to think like a clinician. Combine structured Note-Taking Strategies with proven Study Techniques, Active Recall, and Spaced Repetition, and your notes will become one of the most powerful tools in your medical education journey.





















