Staying Alert During the Graveyard Shift: A Comprehensive Guide for Healthcare Professionals
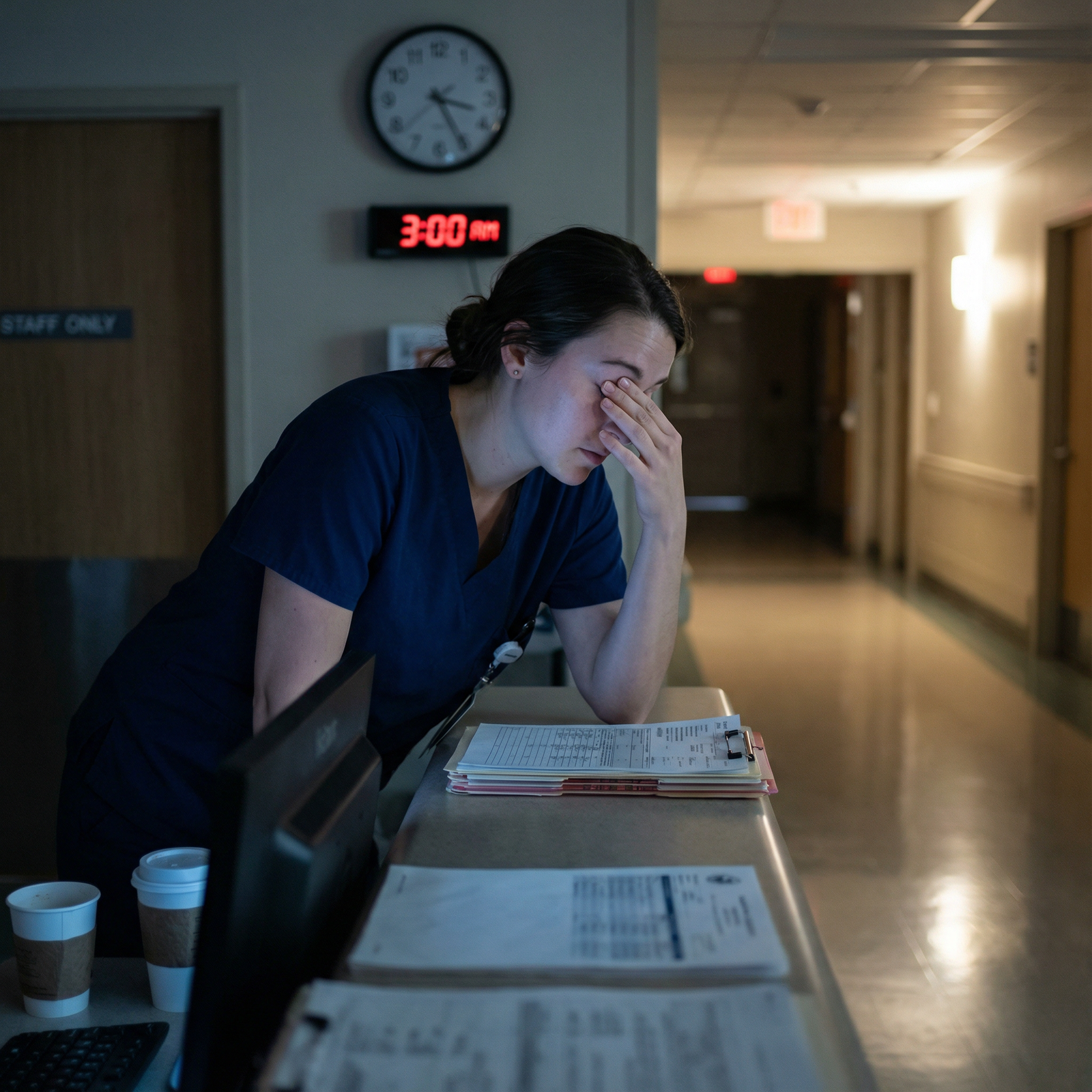
Working the Night Shift in healthcare—whether in the ED, ICU, wards, or on-call—means staying sharp while most of the world sleeps. For residents, nurses, and other frontline staff, those 11 p.m. to 7 a.m. hours can be some of the most demanding and high-stakes of your career.
The disruption to your circadian rhythm (your internal 24-hour body clock) can impair alertness, decision-making, and mood, all while you’re responsible for critically ill patients and rapid clinical judgments. Night shifts are not just tiring—they can impact patient safety, your performance, and your long-term health.
This guide expands on the fundamentals and provides evidence-informed, practical strategies tailored to medical trainees and healthcare workers. You’ll learn how to optimize sleep hygiene, fatigue management, nutrition, light exposure, and workplace wellness so you can survive—and even perform well—on the Night Shift.
Understanding Night Shift Challenges in Healthcare
How Circadian Rhythm Affects Night Shift Performance
Your circadian rhythm regulates core body temperature, hormone secretion (like melatonin and cortisol), appetite, and sleep-wake cycles. It’s strongly influenced by light exposure and usually promotes:
- Wakefulness and peak alertness during daytime (especially late morning)
- Sleepiness and performance dips at night, particularly between 2–6 a.m.
When you work nights, you’re asking your brain to function at a high level during its biologic low point. This mismatch can lead to:
- Microsleeps (brief, uncontrollable episodes of sleep)
- Slower reaction time and impaired psychomotor performance
- Reduced vigilance—critical in monitoring patients, meds, and alarms
- Greater susceptibility to errors, especially in repetitive or monotonous tasks
Night shift work has also been associated with increased risks of:
- Metabolic issues (weight gain, insulin resistance)
- Gastrointestinal problems (reflux, irregular appetite)
- Mood disorders (anxiety, depression)
- Longer-term cardiovascular risk in chronic shift workers
Recognizing that these effects are physiologic— not personal weakness—is the first step to building a sustainable strategy.
Common Experiences Among Night Shift Healthcare Workers
Across specialties and roles, night shift staff often describe:
Sleep Deprivation and Fragmented Sleep
- Daytime sleep tends to be shorter and lighter.
- Noise, light, family obligations, and early scheduled activities (e.g., conferences) reduce sleep opportunity.
- “I slept, but I don’t feel rested” is a frequent complaint.
Persistent Fatigue
- Accumulation of sleep debt across consecutive nights.
- Feeling heavy-eyed or mentally sluggish, especially between 2–5 a.m.
- Needing more time to think through orders, plans, or calculations.
Cognitive and Performance Effects
- Slower recall of clinical information and guidelines
- More difficulty multitasking or handling interruptions
- Higher risk of medication errors, missed subtle signs of deterioration, and documentation mistakes
Mood and Emotional Changes
- Irritability with colleagues, patients, or family
- Feeling disconnected from social life due to opposite schedules
- Reduced empathy when exhausted, sometimes termed “compassion fatigue”
Work–Life and Wellness Strain
- Difficulty maintaining relationships, exercising, and eating well
- Feeling “jet-lagged” even when not traveling
- Reduced time for study, research, or exam prep due to fatigue
Understanding these patterns helps you anticipate rough spots and apply targeted fatigue management strategies instead of just “pushing through.”
Strategy 1: Build a Night-Shift-Friendly Sleep Schedule and Environment
Design a Consistent Sleep Plan
Consistent Sleep Hygiene is the foundation of Night Shift survival. Rather than treating every shift as a one-off, create a structured plan.
For a single or occasional night shift:
- Pre-shift nap: Take a 90-minute nap in the late afternoon or early evening (e.g., 5–6:30 p.m.) before reporting for duty.
- Use caffeine strategically at the start of your shift (details below).
- After the shift, avoid long naps that can disrupt the following night’s sleep if you are returning to a daytime schedule.
For multiple consecutive night shifts:
- Aim for a fixed daytime sleep window, e.g., 9 a.m. to 3 p.m.
- Keep your wake and sleep times as consistent as possible across the stretch of nights.
- On your “turnaround day” (switching back to days), use shorter naps (1–2 hours) and earlier wake times to gradually reset.
Protect Your Daytime Sleep: Make It Non-Negotiable
Think of your post-shift sleep as a protected clinical responsibility—for your own safety and your patients’.
- Set expectations with family/roommates about quiet hours.
- Silence or focus-mode your phone; use auto-replies if needed.
- Schedule deliveries or errands outside your sleep block.
Create a Sleep-Inducing Environment
Your brain expects light = day, dark = night. Help it adjust:
Block out light
- Use blackout curtains or a sleep mask.
- Consider dim, warm lighting if you must be up briefly.
Control noise
- Use white noise machines, fans, or earplugs.
- Close doors and windows where feasible.
Optimize temperature
- Aim for a cool room: around 18–20°C (65–68°F) supports better sleep.
Pre-sleep routine
- Take a warm shower, stretch briefly, or practice 5–10 minutes of mindfulness to drop post-shift adrenaline.

Strategy 2: Use Nutrition and Hydration to Support Alertness
What—and when—you eat on Night Shift directly impacts alertness, gut comfort, and energy stability.
Plan Night-Shift-Friendly Meals
Before your shift (1–3 hours prior):
- Eat a balanced meal with:
- Lean protein (chicken, fish, tofu, eggs)
- Complex carbohydrates (brown rice, quinoa, whole grains)
- Vegetables or salad
- Avoid very heavy, greasy, or overly large meals that can cause sleepiness and reflux once you start working.
During your shift:
- Aim for smaller, frequent meals or snacks rather than one huge “night dinner.”
- Good options:
- Greek yogurt with nuts or seeds
- Hummus and whole-grain crackers or veggie sticks
- Hard-boiled eggs, cheese sticks
- Fresh fruit (banana, berries, apple) instead of vending-machine candy
- Mixed nuts or trail mix (in moderation, due to calorie density)
Avoid:
- Highly processed foods, fast food, and heavy fried options
- Large sugary snacks or energy drinks that cause rapid spikes and crashes
Near the end of shift / pre-sleep:
- Keep it light: a small snack if you’re hungry (e.g., toast with nut butter, small bowl of oatmeal, or fruit).
- Avoid big meals right before daytime sleep; digestion can interfere with sleep quality.
Stay Hydrated Without Ruining Your Sleep
- Hydration supports alertness and reduces headaches and dizziness.
- Sip water consistently across the shift.
- In the last 1–2 hours before bed, reduce heavy fluid intake to avoid multiple bathroom trips once you’re finally sleeping.
Strategy 3: Caffeine as a Tool, Not a Crutch
Caffeine can be a powerful part of fatigue management on the Night Shift—if you use it deliberately.
Time Your Caffeine Intake
- Best window: The first half of your shift.
- Example for an 11 p.m. – 7 a.m. shift:
- 1st coffee/tea: around 10:30–11:30 p.m.
- Optional second smaller dose: around 1–2 a.m.
- Example for an 11 p.m. – 7 a.m. shift:
- Avoid caffeine within 5–6 hours of your planned sleep time.
- If you sleep at 9 a.m., stop caffeine by ~3–4 a.m.
Dose and Form Matter
- Aim for moderate doses: usually 100–200 mg at a time (roughly 1–2 cups of coffee).
- Excessive caffeine can cause:
- Jitters, palpitations
- Anxiety or panic sensations
- GI upset
- Worse rebound fatigue when it wears off
- Consider green tea or lower-dose options if you’re sensitive but still want mild stimulation.
Combine Caffeine with Strategic Naps
Some studies support a “caffeine nap”:
- Drink a small coffee or caffeinated beverage.
- Immediately take a 15–20 minute nap.
- When you wake up, the caffeine is starting to take effect, enhancing alertness.
Only do this if your workplace and role allow it, and you have a safe, appropriate place to rest.
Strategy 4: Breaks, Movement, and Light Exposure for Sustained Alertness
Use Regular Breaks to Reset Your Brain
While Night Shift may feel non-stop, micro-breaks make a real difference in cognitive performance and error reduction.
- Try to take a 5–10 minute break every 1–2 hours, if patient care allows.
- During breaks:
- Stand up, stretch your neck, shoulders, and back.
- Step away from high-stimulation areas if you feel overwhelmed.
- Drink water; have a light snack if hungry.
Physical Activity as Fatigue Countermeasure
Even brief movement can fight drowsiness:
- Walk a loop around the unit or up/down a flight of stairs.
- Do quick stretches:
- Neck rolls
- Shoulder shrugs
- Gentle back bends and hamstring stretches
- A short walk outdoors (if safe and feasible) can combine movement + cool air + natural light.
Light Exposure: Managing Melatonin and Alertness
Light is one of the strongest signals to your circadian rhythm.
During the shift:
- Increase exposure to bright, cool (blue-enriched) light in the early part of the night:
- Work in well-lit areas when possible.
- Some hospitals use bright-light boxes in break rooms; consider them early in the shift.
After the shift:
- On your way home, reduce blue light exposure:
- Wear sunglasses when driving home after sunrise.
- Avoid checking a bright phone screen in bed.
Before sleep:
- Keep your environment dim and calm, promoting melatonin release and better sleep onset.
Strategy 5: Exercise, Social Support, and Mental Techniques
Exercise to Support Overall Workplace Wellness
Regular exercise helps stabilize mood, metabolism, and sleep quality.
- Aim for at least 150 minutes/week of moderate-intensity exercise (e.g., brisk walking, cycling) plus strength training twice weekly.
- For Night Shift workers:
- Short, moderate workouts before your shift can boost pre-shift alertness.
- Gentle stretching or yoga after your shift can help transition to sleep.
Avoid intense workouts in the hour immediately before planned sleep, as they may delay sleep onset for some people.
Maintain Social Connection and Support
Night shifts can feel isolating and can strain relationships with friends and family who keep daytime schedules.
- Connect with colleagues:
- Use calm periods to talk (appropriately) with co-workers about coping strategies.
- Share healthy snacks or create a supportive “night team” culture.
- Stay in touch with loved ones:
- Schedule brief but meaningful check-ins (calls, texts, or shared meals on off-days).
- Explain your schedule and fatigue pattern so others understand your limitations and can support your well-being.
Mental Techniques to Stay Sharp and Centered
Engage your mind during lulls
- Review guidelines, checklists, or pocket cards.
- Do short learning tasks: one article, one topic, one case review.
- Use active recall (e.g., “How would I manage X?”) rather than passive scrolling.
Mindfulness and Micro-Relaxation
- Try 1–2 minutes of focused breathing:
- Inhale for 4 seconds, hold for 4, exhale for 6–8.
- Use brief grounding exercises (“What are 5 things I see, 4 I feel,” etc.) to reset during stressful moments.
- Try 1–2 minutes of focused breathing:
Recognize Warning Signs of Dangerous Fatigue
- Re-reading orders multiple times to understand them
- Forgetting tasks you just heard
- Difficulty keeping eyes open, nodding off while charting
- Irritability out of proportion to the situation
If you notice these signs, prioritize a brief break, ask a teammate to double-check critical tasks, and be transparent with your team about your fatigue level when patient safety is at stake.
Strategy 6: Monitoring and Protecting Your Long-Term Health
Regular Health Check-Ins
Night shift work isn’t just about surviving a single call—it’s about long-term workplace wellness.
Discuss your schedule and symptoms with your primary care clinician:
- Persistent insomnia
- Snoring or gasping (possible sleep apnea)
- Chronic fatigue that doesn’t improve with rest
- New or worsening mood symptoms
Consider referral to a sleep specialist if:
- You suspect a circadian rhythm disorder (e.g., Shift Work Sleep Disorder).
- You have unrefreshing sleep despite good Sleep Hygiene.
- You experience excessive daytime sleepiness when off duty.
Protecting Mental Health
Residency and healthcare work are already psychologically demanding; Night Shift can amplify stress.
- Know your institution’s mental health and counseling resources.
- Watch for:
- Loss of interest in usual activities
- Persistent low mood
- Thoughts of self-harm or feeling that others are better off without you
- Reach out early—to a mentor, program director, trusted colleague, or mental health professional.
Set Realistic Expectations and Boundaries
- On post-call or post-night days, lower your expectations for productivity outside work.
- Protect time for:
- Sleep
- One meaningful social interaction or self-care activity
- Simple, nourishing meals
- Over time, experiment to see what balance of nights, exercise, social time, and rest keeps you functioning at your best.

Putting It All Together: A Sample Night Shift Survival Plan
To make these concepts actionable, here’s an example schedule for a resident working 7 p.m.–7 a.m. for several nights in a row.
On a Workday (During Consecutive Night Shifts)
- 1:00 p.m. – Wake up, hydrate, light snack.
- 1:30–2:30 p.m. – Light exercise (walk, gym, or yoga).
- 3:00 p.m. – Main pre-shift meal: balanced protein + complex carbs + vegetables.
- 4:00–5:30 p.m. – Study, personal tasks, or family time.
- 6:00 p.m. – Commute; mentally prepare for shift.
- 7:00 p.m. – Start shift. Light, bright work area if possible.
- 7:00–11:00 p.m. – One serving of caffeine early on; water regularly.
- 11:00 p.m.–1:00 a.m. – Small snack (yogurt & fruit, nuts).
- 1:00–3:00 a.m. – Optional small second caffeinated drink if needed; short walk or stretch each hour.
- 3:00–5:00 a.m. – No more caffeine. Use bright light exposure and short breaks to fight sleepiness.
- 5:00–7:00 a.m. – Light snack if hungry; begin mentally winding down.
- 7:30 a.m. – Commute home with sunglasses if it’s bright.
- 8:00–9:00 a.m. – Brief wind-down routine: shower, light snack, relaxation.
- 9:00 a.m.–3:00 p.m. – Protected sleep block in dark, cool, quiet room.
Adjust timing based on your specific shift hours and personal response, but keep the same principles: consistent sleep window, early caffeine, healthy meals, and strategic light exposure.
FAQs: Night Shift, Sleep Hygiene, and Fatigue Management
1. How long should a power nap be during a Night Shift, and when should I take it?
A 10–20 minute power nap is ideal—it’s long enough to improve alertness and performance but short enough to avoid deep sleep and sleep inertia. If your workplace allows, aim to nap in the first half of the shift (e.g., between midnight and 3 a.m.). Avoid napping close to the end of your shift if it will interfere with your ability to sleep once you get home.
2. Can I really adjust my circadian rhythm to night work, or will it always feel like jet lag?
Your circadian rhythm can partially adapt, especially if you work multiple consecutive nights and keep a consistent daytime sleep schedule. However, full adaptation is difficult for many healthcare workers who rotate frequently between days and nights. You can still significantly reduce symptoms by:
- Keeping sleep/wake times consistent across a block of nights
- Using bright light during shifts and darkness before sleep
- Avoiding abrupt, large schedule swings when possible
3. What foods or drinks should I avoid during Night Shift to prevent crashes and GI upset?
Avoid:
- Large, heavy, greasy meals—they increase sluggishness and reflux
- High-sugar snacks and sugary energy drinks—they cause rapid spikes and crashes in blood sugar and alertness
- Very spicy or acidic foods if you’re prone to heartburn
- Caffeine in the final 5–6 hours before planned sleep
Focus on moderate portions of lean protein, complex carbs, and fiber-rich foods, plus water or unsweetened beverages.
4. How does caffeine affect sleep, and what’s a safe strategy for Night Shift?
Caffeine can remain active in your body for 5–7 hours or longer. Taken too late in the shift, it:
- Delays sleep onset
- Reduces total sleep time
- Fragments sleep and decreases its restorative quality
For Night Shift:
- Use caffeine early in the shift only (first half).
- Keep doses moderate (about 100–200 mg at a time).
- Stop caffeine 5–6 hours before your intended sleep time.
5. When should I seek professional help about Night Shift-related sleep or fatigue problems?
You should talk to a healthcare professional if you experience:
- Persistent insomnia, despite good Sleep Hygiene
- Excessive sleepiness or dozing off in unsafe situations (e.g., driving home, during patient care)
- Loud snoring, gasping during sleep, or unrefreshing sleep—possible sleep apnea
- Mood changes, burnout, or signs of depression or anxiety
A primary care clinician or sleep specialist can assess for conditions like Shift Work Sleep Disorder and recommend therapies (light therapy, melatonin timing, behavioral strategies, or other interventions).
By combining consistent sleep strategies, smart caffeine use, intentional nutrition, movement, light management, and social/mental support, you can navigate the Night Shift more safely and sustainably. Protecting your own health and alertness is not a luxury—it’s a critical part of providing safe, high-quality care to your patients while preserving your long-term well-being as a healthcare professional.



















