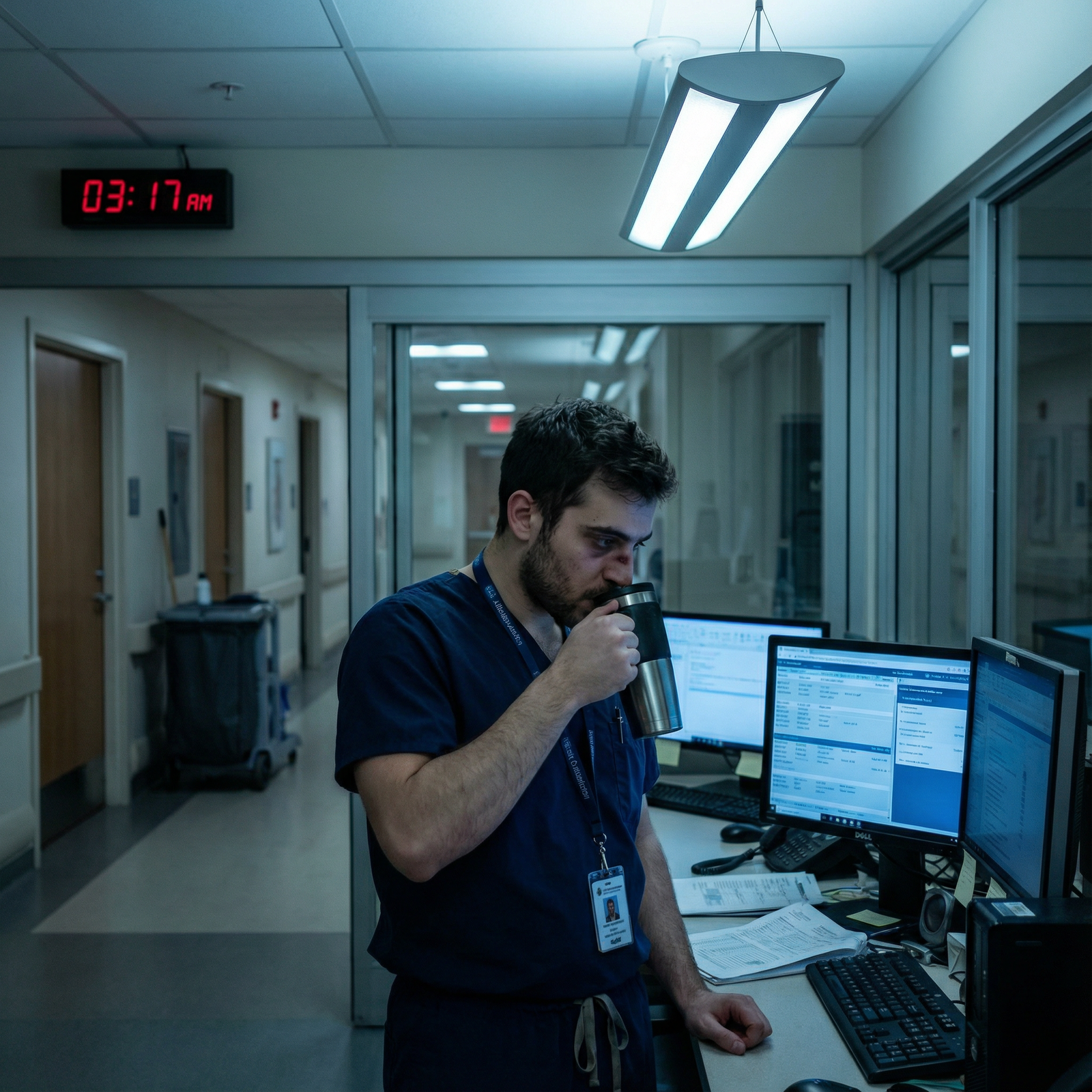
Conquering Fatigue: Innovative Strategies for Night Shift Resilience
When the sun sets and most of the world powers down, hospitals, emergency services, and critical infrastructure come fully alive. For residents and other night shift workers, this reality is part of the job—but it comes with a cost. Night work collides head-on with human biology, increasing fatigue, impairing performance, and elevating long-term health risks.
For trainees in medicine and other demanding fields, fatigue management, sleep optimization, and mental resilience are not optional “extras”—they are core professional skills that protect both patient safety and personal health and wellness. This expanded guide explores evidence-informed, practical strategies to help you not only survive nights, but build sustainable night shift resilience.
Understanding the Night Shift Challenge in Residency
Night shifts challenge nearly every aspect of human physiology and psychology. Recognizing what you are up against is the first step to designing effective countermeasures.
Circadian Rhythm Disruption
Humans are wired to be awake in daylight and asleep in darkness, governed by the circadian rhythm—a roughly 24-hour internal clock driven by the brain’s suprachiasmatic nucleus.
Night work disrupts this system by:
- Forcing alertness during the biological “low point” (typically 2–5 a.m.)
- Suppressing melatonin with artificial light
- Fragmenting or shifting sleep into daytime hours when the body expects to be awake
Consequences for night shift workers include:
- Increased sleepiness and microsleeps
- Slower reaction times and impaired decision-making
- Higher rates of errors, near-misses, and accidents—critical issues in clinical environments
Sleep Quantity and Quality Challenges
Even if you “protect” 7–9 hours for sleep during the day, sleep quality is often poor:
- Environmental noise: traffic, deliveries, children, roommates, neighbors
- Light exposure: sunlight creeping around blinds or through thin curtains
- Social and family demands: school runs, appointments, relationship time
Daytime sleep tends to be:
- Shorter in duration (commonly 4–6 hours)
- More fragmented
- Less restorative, with reduced REM and deep sleep
Over time, this chronic sleep restriction adds up to accumulated sleep debt, worsening fatigue and decreasing resilience.
Health and Wellness Implications of Night Work
Night shift work is associated in the literature with increased risk of:
- Cardiovascular disease (hypertension, coronary artery disease)
- Metabolic issues (weight gain, insulin resistance, type 2 diabetes)
- Gastrointestinal problems (reflux, dyspepsia, irregular bowel habits)
- Mood disorders (depression, anxiety, burnout)
- Reproductive and hormonal changes (especially with long-term rotating shifts)
For residents, these risks combine with high baseline stress, long work hours, and emotional load—making health and wellness strategies even more critical.
Social Isolation and Lifestyle Disruption
Working while loved ones sleep (and vice versa) creates:
- Missed social events and family time
- Difficulty maintaining hobbies and exercise routines
- Strain on relationships and support systems
This social disconnection can erode mental resilience, increase perceived stress, and worsen burnout—especially when layered onto the emotional intensity of clinical work.
Understanding these interconnected challenges allows you to address them proactively instead of simply “pushing through.”
Core Principle #1: Sleep Optimization for Night Shift Workers
High-quality sleep is the foundation of fatigue management. You cannot “hack” your way out of chronic sleep deprivation with caffeine alone. Instead, think strategically about both your sleep environment and your sleep schedule.
Build a Night-Shift-Friendly Sleep Environment
You want your bedroom to signal “nighttime” to your brain, even at noon.
1. Control Light
- Use blackout curtains or a combination of blackout curtains + blinds.
- Consider an eye mask if you can’t fully control room lighting (e.g., call room, shared space).
- Avoid bright light exposure (especially blue light) during the 60–90 minutes before bed:
- Use warm-tone, low-brightness lamps.
- Enable night shift/blue light filters on screens or wear blue light–blocking glasses if you must use devices.
2. Control Noise
- Use foam or silicone earplugs to block background sounds.
- Consider a white noise machine or fan to mask intermittent disruptions (voices, traffic, neighbor noise).
- If living with others, negotiate “quiet hours” and post a simple sign on your door when sleeping after nights.
3. Optimize Comfort and Temperature
- Target a room temperature of 60–67°F (15–19°C).
- Choose a comfortable mattress and pillows that support your preferred sleep posture, especially important if you have back or neck issues from long clinical days.
- Keep bedding breathable (cotton, bamboo, or moisture-wicking fabrics) to prevent overheating.
4. Pre-Sleep Wind-Down Routine
Create a brief, repeatable sequence your brain comes to associate with “sleep time,” for example:
- Light snack (if hungry) → shower → 5–10 minutes of quiet reading or relaxation → bed
- Avoid heavy meals and intense exercise immediately before sleep, as they can delay sleep onset.
Structuring Your Sleep Around Night Shifts
For recurring nights (e.g., a 3–7 night block), use a consistent pattern when possible.
Before the First Night Shift:
- Aim for a 90-minute nap in the late afternoon or early evening (e.g., 5–6:30 p.m.) before your first night.
- If your schedule allows, gradually shift your bedtime later for 1–2 days prior.
During a Block of Night Shifts:
- After your shift, go to bed as soon as reasonably possible (e.g., 8–9 a.m.).
- Aim for at least 6–8 hours of sleep; treat it as non-negotiable.
- Keep your daily sleep/wake timing as consistent as possible across the entire block to help your internal clock partially adjust.
Transitioning Off Nights:
This is often the hardest part and varies by personal preference:
- Option A: Partial Sleep, Early Bedtime
- Sleep a shorter block after your last night (e.g., 3–4 hours).
- Wake by early afternoon, stay active, and go to bed early (8–9 p.m.) to realign with a daytime schedule.
- Option B: Full Sleep, Gradual Shift
- Sleep a near-full block after your last night.
- Accept that your first “day off” will be shorter and adjust gradually over 1–2 days.
Experiment during residency to discover which transition strategy leaves you feeling more restored and less “jetlagged.”

Core Principle #2: Strategic Nutrition and Hydration on Night Shifts
What and when you eat significantly affects your alertness, digestion, and overall health and wellness, especially when your circadian rhythms are misaligned.
Meal Timing Around Night Shifts
Think of your food as fuel strategically timed to support sustained performance:
Pre-shift meal (60–90 minutes before work)
- Make this your largest and most balanced meal, similar to a dinner:
- Complex carbohydrates (brown rice, quinoa, whole grain pasta)
- Lean protein (chicken, fish, tofu, beans)
- Healthy fats (olive oil, avocado, nuts)
- Vegetables for fiber and micronutrients
- Avoid very heavy, greasy food that can cause sluggishness or reflux.
- Make this your largest and most balanced meal, similar to a dinner:
During-shift snacks and light meals
- Aim for small, frequent portions every 3–4 hours to maintain steady energy.
- Combine protein + complex carbs for satiety and stable blood sugar:
- Greek yogurt with nuts
- Whole-grain crackers with hummus
- An apple or banana with peanut butter
- Trail mix (unsalted nuts + seeds + a bit of dried fruit)
End-of-shift nutrition
- Avoid large, high-fat, or high-sugar meals right before sleep.
- If hungry, choose a light snack (e.g., toast with nut butter, a small bowl of oatmeal, or a banana) to prevent waking from hunger without overloading digestion.
Smart Caffeine Use for Fatigue Management
Caffeine can be a helpful tool—but only if you use it strategically:
- Use caffeine early in your shift (first half), not continuously throughout.
- Typical safe total: up to 400 mg/day for most healthy adults, but many night shift workers need less.
- Avoid caffeine in the 4–6 hours before planned sleep to reduce insomnia and fragmented sleep.
- Space doses (e.g., a cup of coffee at 9 p.m. and another at 1 a.m.) rather than “front-loading” or constantly sipping.
Hydration and Gastrointestinal Comfort
Dehydration worsens fatigue and headaches:
- Keep a reusable water bottle with you and aim for steady intake throughout the shift.
- Limit very sugary drinks that can cause energy spikes and crashes.
- If prone to reflux on nights, avoid:
- Very spicy or acidic foods late in the shift
- Large volumes of food at once
- Lying down immediately after eating
Core Principle #3: Napping, Movement, and Physical Activity
Power Naps as a Performance Tool
Short, well-timed naps can significantly improve alertness and performance, especially in the biologic low hours of the night.
Key principles:
- Nap before the shift: A 60–90-minute nap in the evening before starting a night can offset some sleep debt.
- On-shift power naps:
- If your setting allows, take 10–25 minute naps during breaks.
- Ideal timing: pre-dawn hours (e.g., between 2–4 a.m.) when your circadian sleep drive peaks.
- Set an alarm; longer naps (30–60 minutes) increase the chance of waking from deep sleep and feeling groggy.
After a nap:
- Give yourself 5–10 minutes to fully wake up before doing complex tasks or making high-stakes decisions.
- Splash cold water on your face, do a brief brisk walk, or combine with a small dose of caffeine (“caffeine nap”: drink coffee, then nap for 15–20 minutes).
Movement to Combat Fatigue
Prolonged sitting in dim environments deepens fatigue. Light movement boosts circulation and alertness:
- Take quick 2–5 minute “movement breaks” every 1–2 hours:
- Walk the hallways
- Climb one or two flights of stairs
- Do simple stretches (neck rolls, shoulder shrugs, calf raises)
- Use downtime to:
- Stand at the workstation rather than sit
- Review charts while lightly pacing (if appropriate in your setting)
Regular Exercise for Long-Term Resilience
Outside of shifts, regular physical activity supports:
- Sleep regulation
- Mood stabilization
- Cardiovascular and metabolic health
- Overall mental resilience
Aim for:
- 150 minutes/week of moderate aerobic activity (fast walking, cycling, swimming), plus
- 2 strength-training sessions/week
Timing tips for night shift workers:
- Try to avoid vigorous exercise right before your post-shift sleep, as it may delay sleep onset.
- Many residents find:
- Light exercise before a night shift (late afternoon) boosts alertness.
- More intense workouts on days off or between blocks of nights are more sustainable.
Core Principle #4: Mental Resilience, Mindfulness, and Emotional Health
Sustained night work tests not just your body, but your mind. Building mental resilience is essential for error prevention, empathy, and long-term career satisfaction.
Mindfulness and Stress-Reduction Tools
Mindfulness doesn’t require hour-long sessions or perfect silence. You can integrate it into short windows:
- 3-minute breathing exercises between pages or tasks:
- Inhale for 4 seconds, hold for 4, exhale for 6–8 seconds.
- Brief grounding techniques during stressful situations:
- 5–4–3–2–1 method: name 5 things you see, 4 you feel, 3 you hear, 2 you smell, 1 you taste.
- Use mindfulness apps (Headspace, Calm, Insight Timer, Ten Percent Happier) for:
- Guided meditations designed for busy schedules
- Sleep stories or body scans after a shift to ease into sleep
Even 5–10 minutes per day can help dampen the physiological stress response, support emotional regulation, and improve sleep.
Connection and Peer Support
Social connection is a powerful buffer against burnout:
- Build camaraderie with co-residents and colleagues on nights:
- Check in with each other during slow moments.
- Normalize talking about fatigue and coping strategies.
- Create informal peer support:
- Debrief after difficult cases.
- Share “what’s working” for managing nights—sleep routines, meal ideas, small hacks.
- Maintain connection outside work:
- Schedule recurring brief check-ins with friends/partners that fit your night schedule (e.g., a 10-minute FaceTime before your pre-shift nap or right after shift).
Professional Mental Health Support
If you notice:
- Persistent low mood or hopelessness
- Anxiety, panic symptoms, or intrusive thoughts
- Increasing irritability or emotional numbness
- Recurrent thoughts that others would be “better off without you”
reach out promptly:
- Many residency programs offer confidential counseling, wellness resources, or Employee Assistance Programs.
- Consider seeing a psychologist, therapist, or psychiatrist familiar with healthcare workers and shift work.
- Seeking support is a professional strength, not a weakness—it protects both you and your patients.
Core Principle #5: Harnessing Light and Scheduling Strategies
Using Light as a Biological Tool
Light exposure is one of the most powerful regulators of circadian rhythm:
During your night shift:
- Maximize bright, cool-toned light in your workspace, especially early in the shift.
- If feasible, use a 10,000-lux light box for 20–30 minutes at the start of the shift to signal “daytime” to your brain (confirm safety considerations and institutional policies).
After your shift:
- As you leave work, minimize bright light exposure:
- Wear dark sunglasses, even on cloudy days.
- Avoid lingering outside in direct sunlight.
- At home, keep lighting dim and warm until you go to bed.
On days off:
- Get morning daylight exposure soon after waking to anchor your circadian rhythm when transitioning back to day schedule.
Strategic Scheduling (When You Have Any Control)
Residents often have limited control, but where possible:
- Advocate for forward-rotating schedules (day → evening → night), which align better with the body’s natural tendency to adjust to later times.
- Try to avoid:
- Multiple quick turnarounds (e.g., finishing a night shift, then starting days the next morning with minimal rest).
- Very long strings of nights without adequate recovery days afterward.
- If you moonlight or pick up extra shifts:
- Be honest about your current fatigue level.
- Avoid stacking extra nights on top of a heavy clinical week when you’re already depleted.
Proactive scheduling choices, even small ones, significantly impact long-term health and sustainability.
The Real Benefits of Building Night Shift Resilience
Effective fatigue management and sleep optimization are not about being “tough enough” to ignore exhaustion—they’re about practicing safely and living sustainably.
Enhanced Job and Clinical Performance
When you are rested and managing your energy wisely, you are more likely to:
- Make accurate clinical decisions
- Recognize subtle changes in patient status
- Communicate clearly with nurses, consultants, and families
- Learn more effectively from each case and teaching moment
These benefits compound over the course of training.
Improved Health and Wellness Outcomes
Over months and years, consistent night shift resilience strategies can:
- Reduce risk of weight gain, hypertension, and metabolic disease
- Protect mood and emotional stability
- Decrease GI issues related to poor timing of meals and stress
- Maintain better overall health and wellness, even in a demanding field
Greater Satisfaction and Career Longevity
Feeling less exhausted, more connected, and more in control of your schedule—and your energy—supports:
- Higher job satisfaction
- Lower burnout and emotional exhaustion
- More capacity to engage in relationships and activities outside of medicine
- A realistic path to long, meaningful practice rather than early exit due to burnout
Resilience is not about never feeling tired; it’s about having a toolkit that lets you recover, adapt, and continue to grow.

FAQ: Night Shift Fatigue, Health, and Mental Resilience
1. What are the best foods to eat during night shifts to maintain energy?
Focus on balanced, easily digestible options that provide steady energy:
- Before your shift: A full meal with complex carbs (brown rice, quinoa), lean protein (chicken, beans, tofu), healthy fats (olive oil, avocado), and vegetables.
- During your shift: Small snacks every 3–4 hours:
- Greek yogurt with nuts or seeds
- Whole-grain crackers with hummus or cheese
- Fresh fruit (apples, bananas, berries) with a protein source
- Trail mix with unsalted nuts and minimal added sugar
- Avoid large, heavy, or greasy meals and very sugary snacks, which can lead to crashes, GI discomfort, and sleep disruption after your shift.
2. How can I stay alert during a night shift without wrecking my daytime sleep?
Combine multiple strategies:
- Use caffeine strategically in the first half of the shift, avoiding it 4–6 hours before your planned sleep.
- Take short movement breaks every 1–2 hours (walk, stretch, climb a few stairs).
- Consider power naps (10–25 minutes) during breaks if allowed, especially between 2–4 a.m.
- Maximize bright light exposure early in the shift via overhead lights or a light box (if permitted).
- Stay mentally engaged where possible—review learning points, discuss cases with colleagues, or tidy up notes when the clinical load dips.
3. Is napping during night shifts actually safe and beneficial?
When allowed by institutional policy and done thoughtfully, yes:
- Short naps (10–25 minutes) have been shown to improve alertness, reaction time, and performance, especially during circadian low points.
- Keep naps short to avoid deep sleep and post-nap grogginess.
- If you take a longer nap (40–90 minutes), allow more waking time before performing high-stakes tasks.
- Always ensure patient coverage and follow your institution’s rules for rest breaks.
4. How does light exposure affect my sleep and night shift experience?
Light is a powerful signal to your brain about when to be awake or asleep:
- Bright light during your shift, especially early, helps you feel more alert and can partially shift your internal clock.
- Blue light from screens in the hour before sleep can suppress melatonin and delay sleep onset—use filters or dim screens.
- Minimizing light exposure after your shift (sunglasses outdoors, dim lights at home) supports faster sleep onset and more consolidated daytime sleep.
- On days off, morning sunlight helps reset you to a daytime schedule.
5. What mental health resources are available for night shift workers and residents?
Most hospitals and training programs now recognize the toll of night work and offer:
- Resident wellness programs with workshops, small groups, or coaching
- Employee Assistance Programs (EAPs) providing confidential counseling sessions
- Access to psychologists, therapists, or psychiatrists familiar with physician stress and shift work
- Peer support groups and mentoring systems
If you notice sustained mood changes, anxiety, or difficulty coping, reach out early—to your program’s wellness office, occupational health, your primary care clinician, or a mental health professional. Early support can prevent crises and improve both your training experience and long-term mental resilience.
Adapting to nights is a core part of residency and many healthcare careers. By taking intentional steps in sleep optimization, nutrition, movement, mental health, and scheduling, you can transform nights from a purely draining obligation into a manageable—and even growth-promoting—part of your professional life.



















