
Introduction: Why Duty Hours Matter in Medical Residency
Medical residency is one of the most formative—and demanding—phases in a physician’s career. Residents navigate steep learning curves, high-stakes decision-making, and emotionally charged clinical encounters, often while working irregular and extended hours. In this context, the structure and regulation of duty hours play a critical role in shaping not only resident education, but also work-life balance, resident well-being, and ultimately patient safety.
Over the past two decades, the conversation has shifted from “How much can residents work?” to “How can we design healthier work environments that support sustainable, high-quality healthcare training?” This article explores:
- How duty hour regulations evolved and what they currently require
- The impact of long work hours on resident health, performance, and patient care
- Practical strategies programs and residents can use to create healthier work environments
- How to balance service needs, educational value, and human limits in modern medical residency
By understanding the role of duty hours and intentionally designing training systems around them, programs can better protect their residents, enhance learning, and improve the care delivered to patients.
The Role and Rationale of Duty Hour Regulations
Understanding Modern Duty Hour Standards
Duty hour regulations emerged in response to growing evidence that excessive work hours impair performance and increase the risk of medical errors. In the United States, the Accreditation Council for Graduate Medical Education (ACGME) has taken the lead in establishing national standards across specialties.
While some details vary by specialty and program, key ACGME duty hour principles include:
Maximum Weekly Work Hours
- Residents must not exceed an average of 80 hours per week, calculated over a four-week period, including in-house call and moonlighting.
- This cap aims to limit chronic sleep deprivation while acknowledging the realities of clinical workloads in teaching hospitals.
Shift Length Limits
- Residents generally may not work more than 24 consecutive hours of in-house clinical duties.
- Up to 4 additional hours may be used for transitions of care, charting, and education, but not for accepting new patients.
- Interns (PGY-1) in some specialties may have even shorter maximum shift lengths, depending on contemporary program and specialty guidelines.
Rest Periods Between Shifts
- Residents should typically have at least 10 hours of rest between duty periods.
- In rare, well-justified circumstances (e.g., selected educational activities), shorter intervals may be allowed, but these should be the exception, not the rule.
Days Off and Time Away from Hospital
- Residents must receive a minimum of one day free of clinical and educational responsibilities every week, averaged over four weeks.
- They should not be scheduled for more than six consecutive days of duty without a day off.
At-Home Call and Night Float
- At-home call should still allow sufficient rest. Time spent in the hospital due to at-home call counts toward weekly hour limits.
- Night float systems are encouraged as a way to distribute night work more evenly and reduce extended shifts.
These guidelines are not simply bureaucratic constraints; they are designed to protect both patients and residents by recognizing the well-documented effects of fatigue.
Why Excessive Working Hours Are So Dangerous
Chronic overwork takes a toll that extends far beyond feeling “tired.” In the context of healthcare training, the stakes are particularly high, as fatigue may compromise critical clinical decisions.
Key risks of excessive duty hours include:
Cognitive Impairment and Decision Fatigue
- Sleep deprivation impairs attention, memory, and executive function at levels comparable to alcohol intoxication.
- Residents may struggle with diagnostic reasoning, medication dosing, interpretation of imaging, or detecting subtle clinical changes.
Physical and Mental Health Consequences
- Increased risk of hypertension, weight gain, impaired immunity, and musculoskeletal pain.
- Elevated rates of depression, anxiety, and burnout, with some studies showing more than half of residents experiencing at least one symptom of burnout.
Emotional Exhaustion and Cynicism
- Persistent fatigue and stress can erode empathy, increase irritability, and foster a sense of detachment from patients and colleagues.
- Over time, residents may lose the passion and curiosity that initially drew them to medicine.
Work-Life Imbalance and Relationship Strain
- Irregular and prolonged work hours often interfere with family life, friendships, exercise, sleep hygiene, and hobbies.
- Without intentional strategies, many residents experience social isolation and difficulty maintaining meaningful relationships.
In short, duty hours are not just statistics on a schedule; they define the framework in which residents live, learn, and care for patients.
When Duty Hours Go Wrong: A Closer Look at Impact
Case Study: The Human Cost of Long Shifts
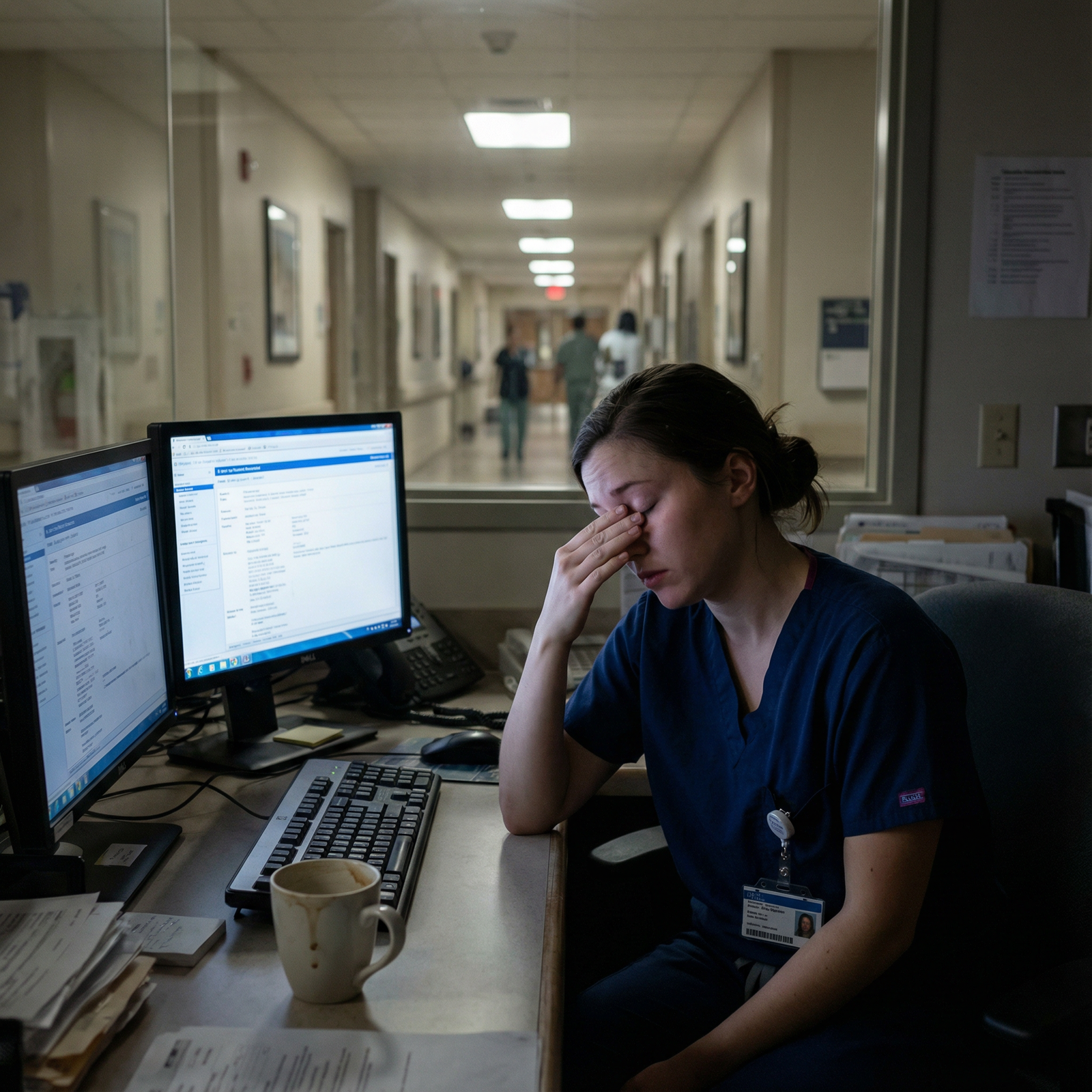
Consider Dr. Sarah, a first-year resident in a busy emergency department of a large academic center. She started residency motivated and optimistic, eager to take on responsibility and learn from complex cases.
Over her first few months, however, she routinely worked back-to-back 28-hour shifts, with minimal protected time for sleep between them. On more than one occasion, a high census and multiple overnight traumas meant that she went nearly the entire shift without meaningful rest.
Initially, Sarah pushed through, telling herself this was “part of paying dues.” Over time, she began to notice:
- Constant fatigue, even on her days off
- Frequent headaches and difficulty concentrating
- Growing irritability with colleagues and patients
- A sense of emotional numbness during serious emergencies
One week, after several nights of fragmented sleep, she miscalculated a medication dose on rounds. The error was caught by a pharmacist before reaching the patient, but the near-miss shook her confidence. Sarah found herself questioning her competence and suitability for the field.
This scenario is not rare. It illustrates how unsafe duty hour patterns can:
- Increase medical error risk
- Undermine resident self-confidence and learning
- Erode the sense of calling and purpose in medicine
Duty hour regulations and thoughtful scheduling practices exist to prevent situations like Sarah’s from becoming routine.
The Education Debate: Do Shorter Hours Hurt Training?
Some faculty and residents worry that stricter duty hour limits may compromise education by:
- Reducing continuity of care and follow-up on patients
- Limiting exposure to rare or complex cases
- Increasing handoffs and fragmentation of learning experiences
The evidence is nuanced:
- Many studies show no significant decline in board exam performance or clinical outcomes after duty hour reforms.
- Some data suggest that well-rested residents learn more efficiently, recall better, and engage more meaningfully in rounds and teaching sessions.
- Handoff quality and systems design, rather than the sheer number of hours, appear to be key drivers of safety and continuity.
The challenge, then, is not to abandon duty hour protections, but to intelligently design educational experiences within these limits. Thoughtful scheduling, structured teaching, and protected learning time can maintain or even improve education while prioritizing resident well-being.
Building Healthy Work Environments Within Duty Hour Limits
Duty hour regulations establish minimum standards, but a truly healthy work environment requires more: culture change, systems-level design, and individual skill building. Below are key strategies programs and residents can use to promote work-life balance and resident well-being in medical residency.
1. Promoting a Supportive and Transparent Culture
Culture often defines the real experience of training more than any formal policy.
Normalize Conversations About Fatigue and Burnout
Programs should actively encourage residents to:
- Speak up when they are unsafe to work or nearing duty hour violations
- Report near-misses or errors without fear of punishment
- Discuss emotional distress after critical incidents or patient deaths
Practical steps include:
- Regular check-ins (e.g., monthly or rotation-based) with program leadership
- Anonymous surveys to monitor workload, burnout, and psychological safety
- Clear communication that preserving resident well-being is a program priority, not a sign of weakness
Leadership Modeling and Accountability
Attending physicians, chiefs, and program directors shape expectations by example. Healthy leadership behaviors include:
- Leaving on time when appropriate, rather than glorifying staying late
- Taking vacation and mental health days themselves
- Intervening when residents consistently stay beyond scheduled hours
- Explicitly valuing efficiency and teamwork over martyrdom and heroics
When senior physicians respect duty hour rules, residents receive the message that well-being and patient safety are non-negotiable.
2. Improving Structural Support: Staff, Systems, and Workflows
Healthy work environments depend on adequate staffing and smart systems.
Manageable Patient Loads and Team-Based Care
Programs can:
- Adjust census caps to ensure resident patient loads are educationally appropriate, not just service-driven
- Expand the use of advanced practice providers (APPs), hospitalists, or additional residents during high-census periods
- Implement geographic rounding or team-based rounding to reduce fragmentation and wasted time
These changes not only protect duty hours, but also enhance teaching quality and patient care.
Efficient Documentation and Technology Use
Electronic health records (EHRs) can either support or undermine duty hours, depending on how they are used.
Actionable strategies:
- Standardize templates for common notes, orders, and discharge summaries
- Offer EHR efficiency training for new residents
- Use voice recognition or mobile tools where available
- Limit non-essential documentation requirements that do not add clinical value
Reducing “click burden” can meaningfully shorten workdays and decrease after-hours charting.
3. Rethinking Shift and Rotation Design
Scheduling is one of the most powerful tools for balancing clinical exposure with rest.
Shorter, Smarter Shifts
Programs can:
- Favor 12–16 hour shifts over continuous 24–28 hour stretches when possible
- Use night float systems to distribute night coverage more evenly and avoid chronic flip-flopping between days and nights
- Carefully monitor the impact of any extended shifts on fatigue, error rates, and resident feedback
Shorter shifts often translate into more alert residents, better bedside teaching, and fewer safety incidents.
Flexible and Predictable Scheduling
Where feasible, programs should:
- Allow residents to indicate preferences for certain rotations, call patterns, or days off (e.g., important family events)
- Post schedules well in advance, reducing anxiety and enabling residents to plan personal obligations
- Provide mechanisms for shift swaps within program policy, promoting autonomy and control
Even modest flexibility can significantly improve residents’ sense of agency and overall work-life balance.
4. Developing Time Management and Efficiency Skills
Individual skills are also a crucial part of surviving—and thriving—in residency.
Teaching Prioritization and Task Management
Residents benefit from explicit coaching on:
- Differentiating urgent vs. non-urgent tasks
- Structuring pre-rounding and rounds to maximize efficiency
- Grouping tasks by location or patient to reduce unnecessary walking and interruptions
- Using “to-do” lists, checklists, and end-of-day wrap-up routines
Workshops, mentorship, and early role modeling by seniors can accelerate this learning curve.
Leveraging Technology for Organization
Residents can use:
- Calendar apps with alerts for conferences, deadlines, and follow-up tasks
- Secure messaging tools (within institutional policy) for efficient team communication
- Task managers or note apps for tracking patient issues and personal reminders
The goal is not to fill every minute with productivity, but to create enough order that true rest becomes possible when off duty.
5. Prioritizing Mental Health and Emotional Resilience
No duty hour policy can eliminate the emotional intensity of caring for sick and dying patients. Structured support is essential.
Accessible Mental Health Resources
Programs should ensure:
- Confidential, low-barrier access to mental health services (counseling, psychiatry, coaching)
- Clear communication that seeking help is encouraged and will not jeopardize evaluation or advancement
- Coverage options or protected time so that residents can attend appointments
Embedding mental health professionals within GME or employee assistance programs can normalize their use.
Wellness and Peer Support Initiatives
Actions that can make a meaningful difference:
- Regular wellness workshops on stress management, mindfulness, nutrition, and sleep hygiene
- Peer support groups or Balint groups for discussing challenging patient interactions
- Debriefings after critical incidents, codes, or unexpected patient deaths
- Social events and community-building efforts that foster camaraderie
These initiatives should be integrated into the curriculum, not relegated to optional “extras” that residents feel guilty for attending.
6. Centering Empathy, Purpose, and Professional Identity
Paradoxically, one of the best antidotes to burnout is reconnecting with the meaning of the work.
Patient-Centered Care as a Source of Fulfillment
Programs can:
- Encourage residents to spend a few extra, intentional minutes at the bedside with selected patients, even on busy days
- Incorporate narrative medicine, reflective writing, or patient stories into conferences and debriefings
- Highlight moments of healing, gratitude, and growth—not just morbidity and mortality
Meaningful patient relationships can counterbalance administrative burdens and remind residents why they chose medicine in the first place.
Professional Identity Formation
Faculty should explicitly discuss:
- How to integrate the physician role with other identities (parent, partner, friend, community member)
- Healthy boundaries between professional and personal life
- Realistic expectations about perfection, fallibility, and growth over a career
Supporting residents in forming a sustainable professional identity is just as important as teaching clinical guidelines.

Resident Strategies for Protecting Personal Well-Being
While institutions bear the primary responsibility for safe duty hour practices, residents can take proactive steps to care for themselves within the system.
Build a Sustainable Foundation
- Prioritize sleep on off days and between shifts; treat it as non-negotiable.
- Maintain basic pillars of health—nutrition, hydration, and regular light exercise (even 10–15 minutes can help).
- Protect at least one non-medical activity you enjoy each week (music, sports, reading, time with loved ones).
Learn to Set Boundaries
- When you are post-call or off duty, avoid lingering unnecessarily to take on new tasks that can be managed by the on-call team.
- Communicate clearly but respectfully if you are at or beyond duty hour limits.
- Practice saying “I can do X, but I won’t be able to do Y safely today. How should we prioritize?”
Use Your Support Network
- Stay connected with family and friends, even if briefly, to avoid isolation.
- Lean on co-residents—many are facing similar challenges and can provide empathy and practical advice.
- Seek formal help (counseling, coaching, mentorship) early, not as a last resort.
These individual strategies work best in environments that already value resident well-being, but they can also help residents advocate for themselves more effectively.
Conclusion: Designing Residency for Longevity, Learning, and Compassion
Duty hour regulations are more than administrative rules; they are a reflection of medicine’s evolving understanding of human limits, safety, and sustainability. In medical residency, the way we structure work hours directly influences:
- Resident well-being and mental health
- The quality and depth of healthcare training
- The safety and outcomes of the patients we serve
- The long-term career satisfaction and retention of physicians
Creating healthy work environments requires aligning policies, culture, and daily practices. That means:
- Respecting evidence-based duty hour limits
- Designing schedules that protect rest while preserving educational value
- Supporting residents with mental health resources, wellness initiatives, and strong mentorship
- Fostering a culture where asking for help and acknowledging fatigue are signs of professionalism—not weakness
By prioritizing humane and thoughtful structures for resident work, the medical community not only safeguards its trainees but also invests in a more compassionate, competent, and resilient physician workforce for the future.
FAQs About Duty Hours, Residency Life, and Resident Well-Being
Q1: What are typical work hours for a resident, and do they really follow the 80-hour rule?
A: ACGME guidelines limit residents to an average of 80 hours per week, over four weeks, inclusive of all in-hospital activities and moonlighting. Actual hours vary by specialty, rotation, and institution. Some high-intensity services may approach the upper limit, while others are significantly lighter. Programs are required to monitor and correct violations; residents should report persistent overages through established channels so they can be addressed.
Q2: Do duty hour restrictions negatively affect resident education or patient care?
A: Evidence to date suggests that duty hour reforms have not systematically harmed educational outcomes such as board pass rates. Some studies show neutral or modestly improved patient outcomes, particularly when reforms are accompanied by robust handoff systems. The biggest determinants of education appear to be teaching quality, case mix, and feedback, rather than raw hours worked. Well-rested residents tend to learn more efficiently and engage more meaningfully in clinical care.
Q3: What support systems exist for residents experiencing burnout or mental health concerns?
A: Most training programs and hospitals offer multiple support resources, such as:
- Confidential counseling or psychotherapy through employee assistance or GME wellness programs
- Peer support groups and resident-led wellness committees
- Access to psychiatrists or primary care providers familiar with trainee needs
- Formal mentoring and coaching relationships
- Debriefings after adverse events or critical incidents
Residents should be informed about these options during orientation and encouraged to use them without stigma.
Q4: Can residency rotation and call schedules be changed to improve work-life balance?
A: Yes. Many programs have redesigned rotations to improve work-life balance while maintaining educational quality. Common changes include:
- Replacing traditional 24–28 hour call with night float systems
- Shortening shift length to 12–16 hours in high-acuity services
- Capping patient loads for interns and senior residents
- Introducing greater scheduling flexibility and early posting of call schedules
Residents can provide feedback through program evaluation, resident councils, and direct conversations with leadership to drive ongoing improvements.
Q5: How can residents manage time more effectively to stay within duty hours and reduce stress?
A: Effective strategies include:
- Prioritizing tasks at the start of each shift (who is sickest, what must be done now vs. later)
- Using standardized templates and checklists for notes, sign-out, and admissions
- Minimizing unnecessary interruptions by batching pages, calls, or EHR tasks when possible
- Leveraging scheduling and task management apps to track responsibilities and deadlines
- Seeking tips from senior residents and attendings known for their efficiency
Over time, these skills help residents complete work within scheduled hours more consistently, leaving more time for rest and life outside the hospital.
By aligning duty hours, culture, and personal strategies, residency can become not just survivable, but a period of profound growth, learning, and professional fulfillment.



















