Navigating Shift Patterns in Residency: Practical Strategies for Managing Hours and Protecting Your Well-being
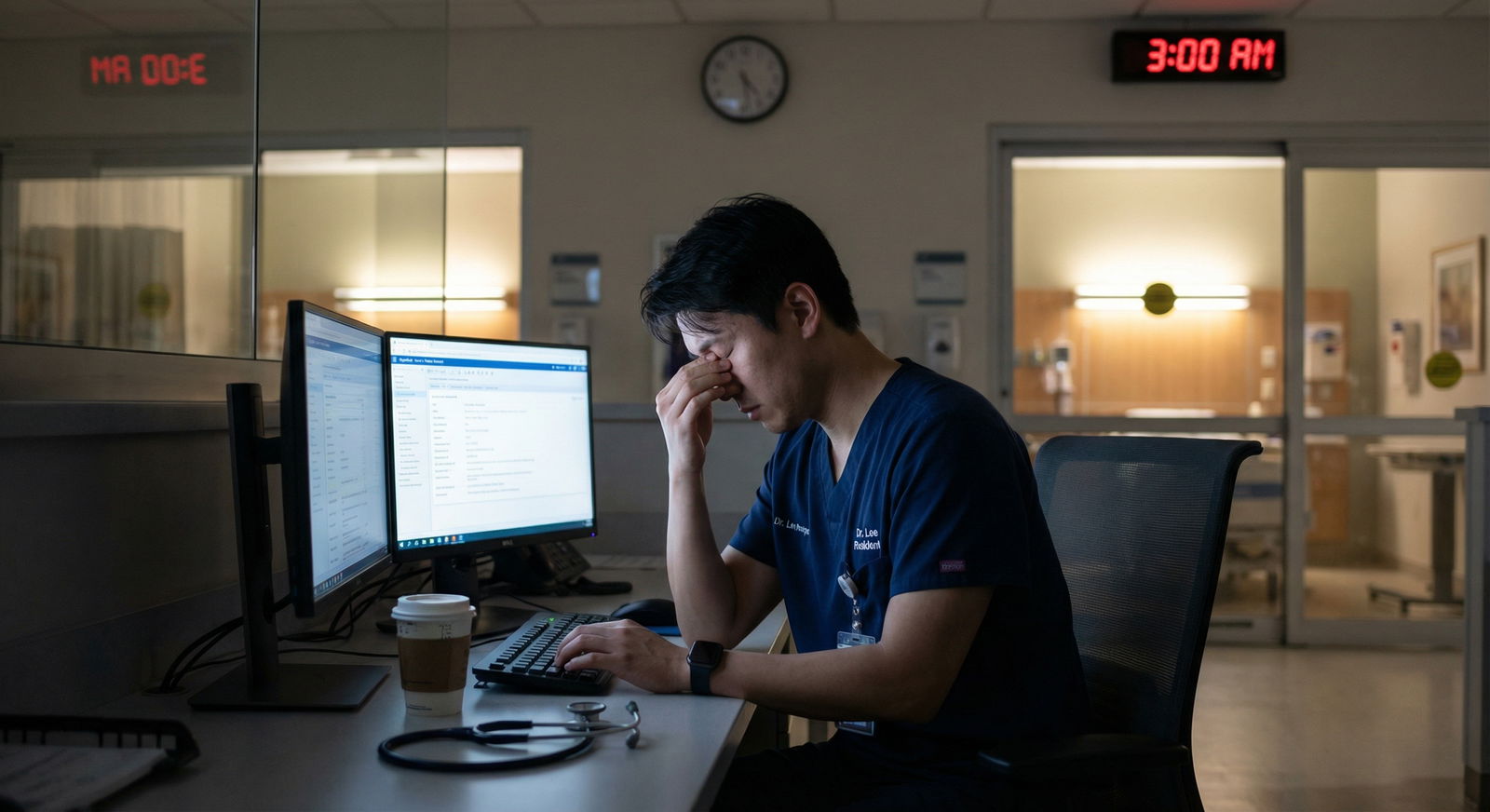
Residency is both a professional marathon and a personal stress test. It’s where clinical knowledge, responsibility, and real-world pressure converge—and where your schedule can feel like it’s running your life. Effective Residency Management isn’t just about surviving 60–80 hour work weeks; it’s about developing sustainable Shift Strategies that support your learning, performance, and long-term Physician Well-being.
This guide will help you understand common shift patterns, anticipate their impact, and apply practical, evidence-informed strategies to protect your health, optimize your performance, and maintain some semblance of Work-Life Balance during training.
The Reality of Residency Work Hours and Why They Matter
Residency schedules vary widely by specialty, institution, and rotation, but most residents in ACGME-accredited programs can expect:
- 60–80 hours per week on average
- Irregular shifts, including nights, weekends, and holidays
- Variable call structures, from night float to 24-hour calls (with post-call days depending on program rules)
ACGME Duty Hour Framework (U.S. Context)
While specifics can vary, typical ACGME guidelines include:
- Maximum 80 hours per week, averaged over 4 weeks
- One day in seven free from clinical duties, averaged over 4 weeks
- In-house call no more than every third night, averaged over 4 weeks (where 24-hour call is still used)
- Requirements for strategic transitions, supervision, and patient safety
Even within these limits, residents frequently report fatigue, stress, and difficulty maintaining Work-Life Balance. Schedules might be “technically compliant” but still functionally exhausting.
How Irregular Shift Patterns Affect Residents
Understanding the consequences of shifting schedules is key to planning your coping strategies.
1. Fatigue and Cognitive Performance
- Sleep debt and circadian disruption can:
- Impair concentration and memory
- Slow reaction times
- Increase risk of clinical errors
- Even moderate sleep loss (e.g., 5–6 hours instead of 7–8) over several nights can have cumulative effects comparable to acute total sleep deprivation.
2. Burnout and Emotional Exhaustion
Chronic overwork and emotional strain can lead to:
- Feelings of detachment or cynicism
- Reduced sense of accomplishment
- Emotional blunting or irritability
Unchecked, burnout affects clinical performance, learning, and career satisfaction, and it increases the risk of depression and suicidal ideation.
3. Strain on Relationships and Personal Life
Irregular schedules can:
- Make it hard to maintain routines with partners, children, or friends
- Interfere with hobbies, exercise, and personal time
- Complicate major life events (weddings, family emergencies, parenting)
Recognizing these challenges is not a sign of weakness—it’s the foundation for intentional, proactive Residency Management.
Mapping and Understanding Your Shift Patterns
Before you can manage your hours, you need a clear picture of what you’re dealing with. Think of this as your “shift anatomy.”
Common Types of Residency Shifts
1. Day Shifts
Typically from early morning to late afternoon/early evening (e.g., 6/7 AM–5/6 PM).
Characteristics:
- More predictable routines
- Higher density of rounds, teaching, and multidisciplinary interactions
- Often followed by charting and sign-out
Implication: Ideal time to build habits around efficiency, pre-rounding, and stable sleep/wake cycles.
2. Night Shifts and Night Float
Night coverage may be:
- Individual nights interspersed with days
- Night float blocks (e.g., 5–6 consecutive nights on, followed by several days off)
Challenges:
- Circadian rhythm disruption
- Reduced support staff at night
- Fewer attendings physically present; more independent decision-making
Implication: Requires a dedicated strategy for flipped sleep schedules, nutrition, and safety (especially on the drive home).
3. Long Shifts and 24-Hour Calls
Still common in some programs (e.g., surgical subspecialties, OB/GYN):
- Continuous in-hospital duty (often 24 hours)
- Sometimes capped at 24 + 4 hours for transitions and educational activities
Challenges:
- Profound fatigue toward the end of the shift
- Decision-making under conditions of prolonged wakefulness
Implication: Requires aggressive planning around sleep before and after call, and smart micro-breaks.
4. Back-to-Back or Compressed Rotations
Examples:
- Series of long days followed by weekend call
- Compressed block of nights followed by rapid flip back to days
Challenges:
- Minimal recovery time
- Frequent schedule transitions that make it hard to establish routine
Implication: You need a rotation-specific plan that includes when to sleep, how to transition, and what you must say “no” to during especially intense weeks.

Core Strategies for Managing Residency Hours and Shift Demands
The goal is not perfection; it’s a sustainable system that supports safe patient care and your own longevity in medicine. These strategies combine time management, sleep science, and Physician Well-being principles.
1. Protecting Sleep: Non-Negotiable for Performance and Safety
Sleep is your primary performance-enhancing “drug.” Treat it like a clinical priority.
Build Strong Sleep Hygiene (Even on Rotating Shifts)
- Dark, cool, quiet bedroom:
Use blackout curtains, a sleep mask, white noise, and keep the room slightly cool. - Screen discipline:
Limit bright screens 30–60 minutes before sleep; consider blue-light filters if using your phone. - Consistent pre-sleep routine:
A short, repeated ritual (shower, light reading, stretching) signals your brain it’s time to sleep—even at odd hours.
Strategies for Night Shifts
- Anchor sleep:
Aim for a “core” sleep block during the day that is consistent across your night block (e.g., 9 AM–1 PM), plus supplemental naps. - Strategic caffeine use:
Use caffeine early in the shift, avoid it 4–6 hours before planned sleep to reduce insomnia. - Post-shift safety:
If very tired, nap briefly before driving, or use public transportation/ride-share if available.
Napping Wisely
- Short “power naps” (15–30 minutes):
Improve alertness without deep sleep inertia. - Pre-call nap:
Even 60–90 minutes before a long call can provide a buffer against fatigue.
2. Time Management as a Clinical Skill
Think of time management as a core competency—just like interpreting EKGs.
Plan Your Week with Intention
- Preview your schedule:
At the start of each rotation or week, identify:- Longest days
- Call nights
- Ideal windows for meals, workouts, and errands
- Block time for essentials:
Put non-negotiables in your calendar—sleep, commute, 2–3 workouts per week, and one block for personal life (family/friends/hobby).
Use Tools and Systems, Not Just Willpower
- Task management apps:
Tools like Notion, Todoist, or even simple notes apps can track:- Follow-up labs/imaging
- Call-backs
- Study goals and board prep
- Batch similar tasks:
Check messages/inbox/EHR in batches instead of constantly switching tasks. - Prioritize with “must-do” vs. “nice-to-do”:
Each day, identify 1–3 critical tasks outside of direct patient care and accomplish those first when you have protected time.
Collaborate and Delegate Where Appropriate
- Leverage your team:
Nurses, pharmacists, social workers, and other residents are partners. Don’t shoulder everything solo when tasks can be shared. - Ask for help early:
If you’re drowning, let your senior resident know before things become unsafe.
3. Managing Stress and Protecting Physician Well-being
Residency stress is expected; suffering in silence is not.
Everyday Micro-Strategies
- Mindful minutes:
Take 1–3 minutes between patients to do simple grounding:- 4–6 deep breaths
- Quick body scan (relax jaw, drop shoulders)
- Name 3 things you can see/hear/feel
- Movement snacks:
Even 5–10 minutes of walking stairs, stretching, or a short body-weight routine during a lull can boost energy and mood. - Micro-boundaries:
Protect small acts of autonomy:- Sit down to eat when possible
- Step outside for fresh air once per shift
- Use your scheduled break rather than skipping it “to be a hero”
Structured Coping Practices
- Exercise “minimum effective dose”:
Aim for:- 2–3 short workouts per week (20–30 minutes)
- Mix of strength training and cardio
Even brief sessions count and have measurable mental health benefits.
- Reflection and debriefing:
Journaling for 5 minutes after a tough day or joining resident debrief groups can normalize stress and help process difficult cases.
4. Building a Supportive Network and Culture
Training is a team sport. Strong relationships buffer against burnout.
Peer Support
- Find your “residency people”:
A small group you can text after a rough call night or celebrate wins with. - Normalize real talk:
Share challenges, not just achievements—this reduces stigma and isolation.
Mentorship and Sponsorship
- Identify multiple mentors:
Consider:- A clinical mentor in your specialty
- A wellness-focused mentor who models sustainable practice
- A research or career mentor
- Ask specific questions:
Instead of “How do you balance it all?” try:- “How did you manage night shifts when you were a PGY-1?”
- “What do you wish you had done differently to protect your well-being?”
5. Fueling Your Body: Nutrition and Hydration on a Tight Schedule
Food is more than calories—it’s cognitive fuel.
Plan Ahead for Challenging Rotations
- Batch meal prep on off days:
Simple, portable options:- Grain + protein bowls (e.g., quinoa, chicken, roasted veggies)
- Wraps or sandwiches
- Overnight oats or yogurt parfaits
- Smart snacks:
Pack:- Nuts, trail mix
- Fruit (apples, bananas, oranges)
- Greek yogurt, cheese sticks
- Protein bars with moderate sugar
Hydration Habits
- Carry a water bottle:
Keep it at your workstation or in your white coat pocket. - Use cues:
Pair water breaks with existing habits (after sign-out, each time you log into the EHR, etc.).
6. Communication and Advocacy Around Work Hours
Effective communication is central to safe care and healthy Shift Strategies.
Upfront Communication About Schedules
- Share constraints early (when appropriate):
If you have critical personal commitments (e.g., childcare, medical appointments), discuss them with your chief residents or program coordinator as early as possible. - Be solution-oriented:
When requesting schedule adjustments, propose alternatives:- Offer swap options
- Volunteer for less popular shifts in exchange when feasible
Speak Up When You’re Overwhelmed
- Know the escalation path:
Senior resident → Chief resident → Program director → GME office. - Frame concerns around safety and learning:
For example:“I’m consistently staying past duty hours and I’m worried about my ability to safely care for patients and maintain required rest.”
Documenting patterns can make it easier to communicate concretely.
7. Using Institutional and Professional Resources
Residency Management isn’t just on your shoulders; your program has responsibilities too.
Wellness and Mental Health Services
- Employee Assistance Programs (EAP):
Often provide confidential counseling, financial or legal advice, and stress management resources. - On-site or affiliated mental health providers:
Accessible for therapy or psychiatric care, often with resident-specific pathways. - Burnout and resilience workshops:
Look for training in mindfulness, emotional intelligence, or cognitive-behavioral strategies tailored to clinicians.
Educational and Academic Support
- Study groups and board review resources:
Help you use limited study time more efficiently. - Time management or efficiency workshops:
Offered by some GME offices to enhance clinical workflow and reduce unnecessary after-hours work.

Integrating Work-Life Balance into a Realistic Residency Life
Work-Life Balance in residency won’t look like a 9–5 job—but it also doesn’t mean abandoning your personal life entirely. The key is intentional, flexible balance.
Redefine Balance for the Residency Phase
Instead of aiming for daily balance, think in weeks or months:
- Some rotations are survival mode; others allow more recovery and personal time.
- During lighter months, invest in:
- Relationships
- Health (appointments, regular exercise)
- Hobbies and intellectual interests outside medicine
Protect at Least One Domain of Your Non-Clinical Life
You might not be able to do everything, but you can prioritize something:
- Weekly dinner with a partner or friend (even if virtual)
- One hobby session per week (music, running, art, gaming)
- Dedicated family time on your golden weekend
Being intentional about even a small slice of your life outside the hospital can significantly improve resilience.
Long-Term Perspective: You’re Building a Career, Not Passing an Endurance Test
Residency is finite. The habits you form now—around sleep, boundaries, communication, and self-care—will shape your life as an attending. Prioritizing Physician Well-being and sustainable Shift Strategies is an investment in decades of practice, not a sign you’re “less dedicated.”
FAQ: Residency Hours, Shift Strategies, and Well-being
1. What is the maximum number of hours residents can work per week?
In ACGME-accredited programs in the U.S., residents are generally limited to 80 hours per week, averaged over 4 weeks, inclusive of all in-house call and moonlighting. Individual programs and specialties may have additional restrictions or local policies. Always review your program’s specific duty hour policy and know how to report violations confidentially if needed.
2. How can I realistically manage sleep deprivation as a resident?
You likely can’t eliminate sleep loss, but you can mitigate its effects:
- Prioritize a consistent core sleep window whenever possible.
- Use short power naps (15–30 minutes) before or during long shifts.
- Protect your sleep environment (dark, cool, quiet).
- Limit caffeine to the first half of your shift and avoid it close to planned sleep.
- If you feel unsafe driving post-call, nap briefly or arrange alternative transport.
If you experience persistent insomnia or excessive daytime sleepiness, consult a healthcare professional—sleep disorders can coexist with shift work.
3. What should I do if I feel overwhelmed or burned out during residency?
Take feeling overwhelmed seriously and respond early:
- Talk to someone you trust: A co-resident, chief, mentor, or faculty advisor.
- Access institutional resources: Employee Assistance Programs, in-house counseling, or wellness offices.
- Consider adjustments: Discuss rotation changes, schedule accommodations, or temporary reduction of non-essential commitments if possible.
- Seek professional help: If you’re noticing signs of depression, hopelessness, or thoughts of self-harm, reach out urgently—this is a medical issue, not a personal failure.
4. Are wellness and support programs really useful, or are they just “checkbox” initiatives?
The quality of wellness initiatives varies by institution, but many programs offer genuinely helpful resources:
- Confidential counseling or therapy
- Mindfulness or resilience training with practical techniques
- Peer support groups and formal debriefing sessions
- Access to gym facilities or fitness classes
- Protected time for wellness or reflection during some rotations
Experiment and see what fits you. If something isn’t helpful, that’s feedback—not a sign that wellness doesn’t matter.
5. How can I communicate my needs around scheduling without being seen as “difficult”?
Approach these conversations with clarity, professionalism, and collaboration:
- Prepare specifics: Explain the issue clearly (e.g., chronic duty hour overages, major personal constraint).
- Propose solutions: Offer shift swaps or alternatives where possible.
- Frame around safety and sustainability: Emphasize that managing your schedule effectively helps you provide safer, more consistent patient care.
- Use the right channels: Start with your senior or chief resident, and escalate respectfully if needed.
Most program leaders prefer early, clear communication to silent struggle that leads to errors or attrition.
By understanding your shift patterns, applying practical Shift Strategies, and leveraging institutional support, you can transform residency from a purely exhausting rite of passage into a challenging but sustainable phase of growth. Residency Management done well is not just about surviving these years—it’s about setting yourself up for a long, meaningful career in medicine while preserving your health, relationships, and sense of purpose.



















