
Is Your Residency Program Really Compliant with Work Hour Laws?
Residency training sits at the intersection of intense clinical responsibility, high-stakes learning, and personal well-being. While long hours have historically been seen as a “rite of passage,” modern Residency Training recognizes that excessive fatigue harms both Resident Well-being and Patient Safety. That’s why Work Hour Regulations and ACGME Compliance are not just bureaucratic checkboxes—they are core components of a safe and sustainable training environment.
This guide will help you understand the current ACGME work hour standards, why they matter, how to evaluate your own program’s compliance, and what to do if you suspect violations. Whether you’re a new intern or a senior resident, knowing this information can empower you to protect your education, your health, and your patients.
Understanding ACGME Work Hour Regulations
Residency Work Hour Regulations are set by the Accreditation Council for Graduate Medical Education (ACGME), the body that accredits most U.S. residency and fellowship programs. These rules are designed to limit fatigue, preserve Resident Well-being, and support Patient Safety while maintaining high-quality clinical education.
The Role of the ACGME in Residency Training
The ACGME, founded in 1981, oversees Graduate Medical Education (GME) to ensure programs meet defined standards in:
- Educational quality
- Supervision and patient care
- Professionalism and safety
- Resident support and well-being
One crucial component is duty hour standards (often called “work hours”). These standards apply across most specialties and must be followed for ACGME Compliance and continued accreditation status.
Core ACGME Work Hour Regulations
While specific language may vary by specialty and year, the following principles represent the core of current ACGME Work Hour Regulations:
80-Hour Weekly Limit (Averaged Over 4 Weeks)
- Residents may not work more than 80 hours per week, including all in-house call, moonlighting, and clinical work, averaged over a rolling four-week period.
- Occasional weeks may exceed 80 hours, but the average across four weeks must remain at or below 80.
Maximum Shift Length and In-House Call
- Traditional in-house call every third night (q3 call) is no longer the norm in most programs. Instead, many programs use night float or shift-based systems.
- ACGME rules typically limit the maximum continuous duty period (for most residents) to 24 hours of continuous scheduled clinical duties, with up to 4 additional hours for transitions of care and educational activities, not for new patient admissions or routine clinical work.
Time Off Between Shifts (Minimum Rest Periods)
- Residents should have a minimum of 8 hours off between scheduled clinical duties.
- Ideally, residents receive 10 hours off between shifts when possible.
- In some rare educational circumstances, the rest interval may be reduced, but programs are expected to prevent this from becoming routine.
Required Time Off Each Week
- Residents must receive at least one day (24 continuous hours) off in seven, free of all clinical duties and required educational activities, averaged over four weeks.
- Some programs also emphasize scheduled “golden weekends” (full weekends off) or protected days to promote wellness.
Maximum Frequency of Overnight Responsibilities
- Traditional rules limiting overnight call to no more frequently than every third night (q3) still inform scheduling philosophy, even as many programs shift toward night float systems to reduce prolonged continuous duty.
Moonlighting Rules
- Any internal or external moonlighting must count toward the 80-hour weekly limit.
- Programs may prohibit moonlighting altogether if they feel it compromises Resident Well-being or education.
Fatigue Mitigation and Education
- Programs must educate residents and faculty about fatigue recognition, sleep hygiene, and fatigue mitigation strategies.
- Institutions should provide safe transportation options or backup systems when residents are too fatigued to drive safely.
Balance of Service and Education
- The ACGME emphasizes that residents must have an appropriate balance between patient care responsibilities, education, and rest. Residents should not be used as purely service labor.
Understanding these standards provides the foundation for assessing your program and advocating effectively when you notice concerns.
Why ACGME Compliance and Work Hour Limits Matter
Work hour limits are not about “making residency easy.” They are about making residency effective, sustainable, and safe—for both residents and patients.
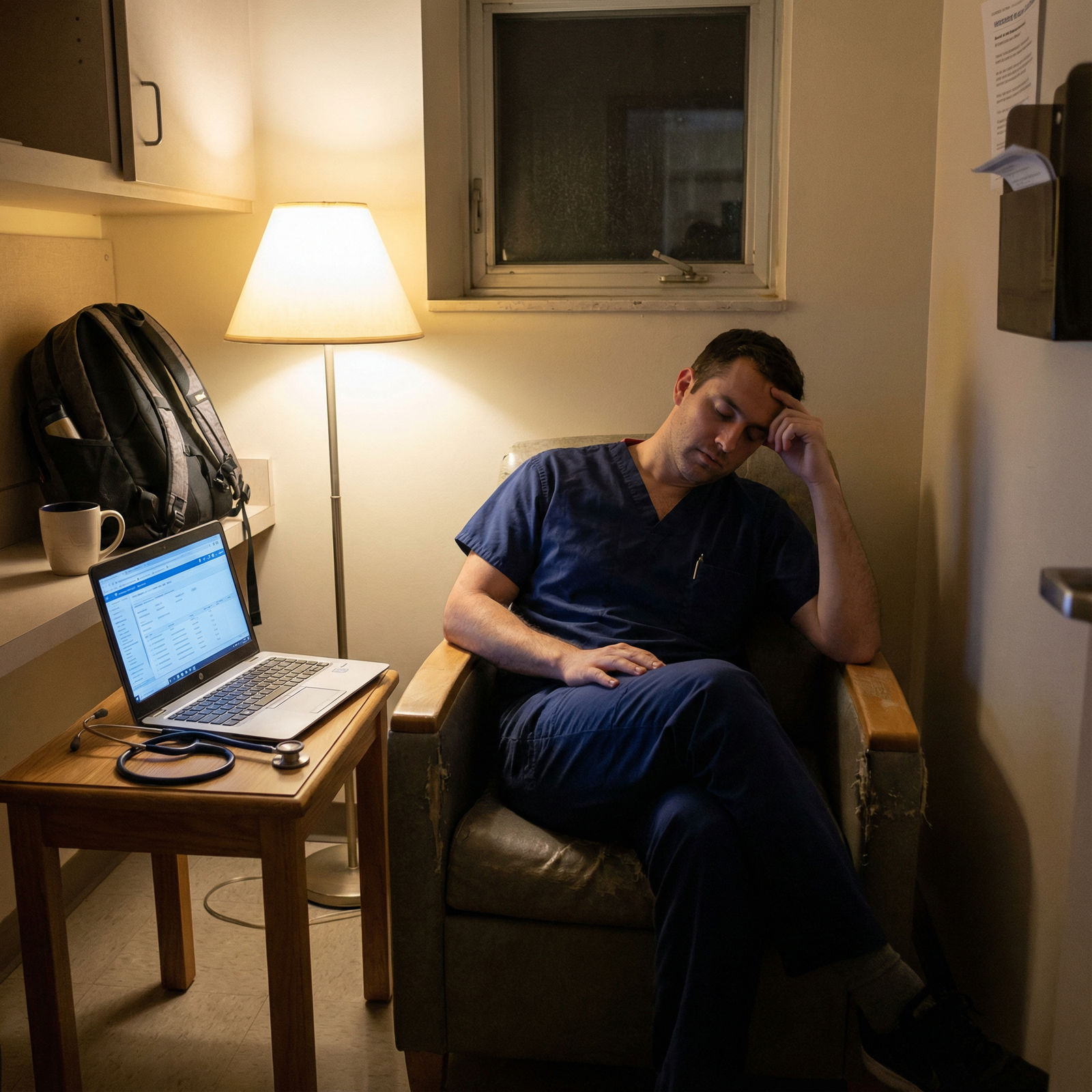
1. Resident Well-being and Mental Health
Chronic sleep deprivation and unrelenting hours are strongly linked with:
- Burnout
- Depressive symptoms and anxiety
- Impaired concentration and memory
- Increased risk of substance misuse and suicidal ideation
Residents facing extended periods of >80-hour weeks, insufficient post-call rest, or no true days off are at high risk for both physical and psychological harm. In contrast, programs that respect Work Hour Regulations and actively monitor wellness:
- Improve resident satisfaction and morale
- Decrease burnout and turnover
- Foster a culture where help-seeking and vulnerability are acceptable
Resident Well-being is not just a moral imperative; it is a prerequisite for high-quality clinical performance.
2. Patient Safety and Clinical Performance
Fatigued clinicians are more likely to:
- Make diagnostic and medication errors
- Miss subtle clinical changes
- Communicate poorly during handoffs
- Show slower reaction times and impaired judgment
Multiple studies have associated prolonged duty hours and inadequate rest with increased medical errors and adverse patient events. ACGME Compliance with duty hour standards is therefore directly linked to Patient Safety:
- Well-rested residents think more clearly.
- Handoffs can be structured and deliberate rather than rushed at the end of a 30+ hour stretch.
- Supervisors can more reliably trust residents’ decision-making.
3. Educational Quality and Long-Term Career Sustainability
Residency Training is not just service work; it is meant to be guided, high-quality education. When duty hours are excessive:
- Residents are more likely to focus only on “tasks” instead of learning.
- Teaching moments get missed because everyone is exhausted.
- Time for reading, reflection, and deliberate practice shrinks.
Conversely, when programs honor Work Hour Regulations:
- Residents can engage more deeply with teaching rounds and conferences.
- There is time for self-study, board prep, and scholarly projects.
- Residents are more likely to sustain enthusiasm for their specialty long-term.
4. Program Accreditation and Institutional Reputation
Non-compliance with ACGME Work Hour Regulations can have serious consequences for programs:
- Warnings or citations from the ACGME
- Required corrective action plans or focused site visits
- Probation or, in extreme cases, loss of accreditation
For residents, training in a program with accreditation problems can:
- Create anxiety about the value of their training experience
- Affect future fellowship or job prospects if program reputation suffers
- Lead to disrupted rotations or major schedule changes during remediation periods
In short, Work Hour Regulations aren’t optional guidelines; they are critical to maintaining a stable, reputable training environment.
How to Assess Whether Your Residency Program Is Compliant
You probably have a “gut feeling” about your schedule—but it’s helpful to assess compliance systematically. Here are practical steps to evaluate whether your program adheres to Work Hour Regulations and supports Resident Well-being.
Step 1: Review Your Program’s Official Policies and Schedules
Start with written documentation. Ask for or review:
- The residency program handbook
- GME office policies on duty hours and fatigue
- Sample rotation schedules and call schedules
Look for:
- Explicit reference to ACGME duty hour standards
- Clear policies on post-call days, days off, and night float
- Defined processes for duty hour logging and correction
If you do not see clear, written policies, that is your first red flag; transparency is a cornerstone of ACGME Compliance.
Step 2: Log Your Actual Work Hours Accurately
Most programs use an electronic duty hour logging system. However, it’s wise to keep your own parallel record for comparison, especially if you suspect under-reporting or pressure to misrepresent hours.
In your personal log (simple spreadsheet or app):
- Document start and end times of each shift.
- Include late stays for emergencies, procedures, or family meetings.
- Note call nights, cross-cover responsibilities, and telehealth or home-call duties that generate significant work.
- Track your days off and post-call days.
After 4–6 weeks, compare:
- Are you staying under the 80-hour averaged limit?
- Are you getting one day off in seven, averaged over four weeks?
- Do you have at least 8 hours (ideally 10) between clinical shifts most of the time?
- Are post-call days truly free from clinical duties?
Patterns matter more than isolated exceptions. One exceptionally busy week may be explainable; chronic overwork is not.
Step 3: Talk Openly with Co-Residents
Informal conversations are powerful reality checks. Ask colleagues at your level and above:
- “How often do you feel like we’re actually under 80 hours?”
- “Do you log your true hours, or do you feel pressured to adjust them?”
- “Do you routinely get your full day off?”
- “Are there rotations everyone dreads because the hours are out of control?”
If many residents share similar concerns—especially across multiple classes—this strongly suggests a systemic issue rather than isolated overwork.
Step 4: Compare Culture Versus Policy
Sometimes policies look perfect on paper, but the culture undermines them. Warning signs include:
- Faculty or seniors discouraging accurate duty hour reporting (“Just log out—everyone does it”).
- Program leadership informally rewarding residents who routinely stay late and punishing those who respect their hours.
- A culture where missing conferences or teaching due to fatigue is stigmatized rather than addressed.
Healthy programs explicitly encourage:
- Honest duty hour reporting
- Use of backup systems when patient volume spikes
- Open discussion of fatigue and wellness without fear of retaliation
Step 5: Use Institutional and GME Resources
Your institution’s Graduate Medical Education (GME) office exists to oversee Resident Well-being and program ACGME Compliance. Key resources often include:
- Anonymized duty hour dashboards
- Wellness committees or Resident councils
- Ombudspersons or confidential liaisons
- Anonymous reporting mechanisms (email, hotlines, online portals)
If you suspect a pattern of non-compliance, these resources can guide you on institutional policies, protection from retaliation, and possible next steps.
Step 6: Know Your Rights and Protections
As a resident, you have the right to:
- A safe, non-retaliatory environment for raising concerns
- Protection from harassment or punishment for truthful reporting of duty hours
- Information about the program’s accreditation status and any ACGME citations
Many institutions also have whistleblower policies and non-retaliation statements embedded in their GME documents. Familiarize yourself with them. Knowing your rights makes it feasible to advocate for both yourself and your peers.
Navigating Suspected or Confirmed Work Hour Violations
If you determine that your residency program is not consistently honoring Work Hour Regulations, it can be uncomfortable to know what to do next. There are ways to approach the situation thoughtfully and strategically.

Step 1: Document Specific Violations and Patterns
General complaints like “we’re always overworked” are harder to act on than concrete data. Strengthen your case by:
- Keeping detailed, date-specific logs of duty hours.
- Noting specific shifts where you exceeded 24+4 hours or violated minimum time off.
- Identifying rotations where the 80-hour limit is repeatedly exceeded across multiple weeks.
- Gathering de-identified examples from peers (with their consent) showing similar patterns.
Specific, well-documented concerns are far more likely to receive serious attention and prompt corrective actions.
Step 2: Consider the Context and Pattern
Before escalating:
- Ask: Is this a temporary surge (e.g., COVID surge, multiple attendings out sick), or is it chronic?
- Check: Are adjustments being made (e.g., float coverage added, schedules revised), or is leadership ignoring the problem?
- Reflect: Are both interns and seniors affected, or is the burden falling disproportionately on certain groups?
ACGME recognizes that rare, extraordinary circumstances may temporarily strain duty hours, but chronic non-compliance is not acceptable.
Step 3: Engage Program Leadership First When Safe
When you feel safe doing so, start by raising concerns at the program level:
- Talk with your chief residents or class representative.
- Meet with your program director or associate program director.
- Bring your data and observations in a professional, solutions-focused manner.
You might say:
“Over the last eight weeks, my log shows an average of 86 hours per week during this rotation, and several of us have missed required days off. I want to share these patterns because I’m concerned about fatigue and patient safety. Are there ways we can adjust coverage or schedules to stay within ACGME standards?”
Programs that value resident input will appreciate early, honest, data-driven feedback.
Step 4: Use Anonymous or Formal Reporting Mechanisms if Needed
If:
- Local attempts don’t lead to meaningful changes
- You feel unsafe raising concerns directly
- There is a culture of retaliation or intimidation
…then consider:
- Anonymous institutional reporting hotlines
- Directly contacting the GME office or DIO (Designated Institutional Official)
- Using the ACGME Resident/Fellow Complaints Process (available on the ACGME website)
When reporting externally, be prepared with:
- Concrete descriptions of violations
- Approximate dates and services involved
- Evidence that local solutions were attempted (if applicable)
The ACGME takes duty hour and training environment concerns seriously and will protect anonymity to the greatest extent possible.
Step 5: Build and Lean on Support Networks
Navigating these issues can feel isolating. Sources of support include:
- Co-residents and chief residents
- Program or faculty mentors you trust
- Resident wellness committees or housestaff councils
- Specialty-specific resident associations
- Mental health services (often provided free and confidentially by your institution)
You are not alone in caring about Work Hour Regulations, Resident Well-being, and Patient Safety. Many residents across the country face similar challenges and have successfully advocated for change.
Practical Strategies for Residents to Cope Within the System
Even in programs that are generally compliant, certain rotations will still feel intense. While the responsibility to create safe schedules lies with the program, there are strategies you can use to protect yourself and your performance.
Time Management and Efficiency on Busy Services
- Prioritize tasks using a daily to-do list (urgent vs. important).
- Use checklists for admissions, discharges, and cross-cover to reduce cognitive load.
- Batch similar tasks (e.g., all discharge summaries, all phone calls) when possible.
- Learn “smart charting” tricks from seniors to document efficiently without cutting corners.
Fatigue Management and Sleep Hygiene
- Protect your pre-call and post-call sleep as non-negotiable when possible.
- Use short power naps (15–20 minutes) during long nights if safe and feasible.
- Maintain a consistent sleep routine on your off days to stabilize circadian rhythms.
- Limit caffeine late in your shift to avoid sleep disruption post-call.
Boundaries and Saying “No” Appropriately
- If you are well beyond duty hour limits or dangerously fatigued, it is appropriate to say:
- “I’m concerned about my ability to provide safe care if I stay longer. Is there a backup plan we can activate?”
- Use your chain of command: senior resident → chief resident → attending → program leadership.
You are not failing by respecting your limits; you are upholding Patient Safety and ACGME standards.
FAQ: Residency Work Hours, ACGME Compliance, and Your Rights
1. What happens if residency programs repeatedly violate ACGME Work Hour Regulations?
If programs are found to be repeatedly non-compliant, the ACGME can:
- Issue citations or warnings
- Require formal corrective action plans and follow-up evaluations
- Conduct site visits focusing on Resident Well-being and duty hours
- Place the program on probation or, in severe cases, withdraw accreditation
Such actions can affect the program’s reputation, recruitment, and, in extreme situations, residents’ ability to complete accredited training. This is why most institutions take duty hour concerns very seriously once they are documented and raised.

2. Can my program force me to alter my duty hour logs or discourage accurate reporting?
No. Pressuring residents to falsify duty hour data is a serious violation of ACGME expectations and institutional integrity. You have the right to:
- Report your actual hours worked
- Raise concerns if you feel coerced to under-report
- Use anonymous reporting channels if needed
If you experience pressure to misrepresent hours, document the situation and consider discussing it with the GME office, a trusted mentor, or the ACGME through its resident complaint process.
3. Are there any exceptions to the 80-hour per week rule?
The 80-hour limit (averaged over four weeks) is a firm standard. However:
- A single very busy week above 80 hours can be acceptable if the 4-week average remains at or below 80 hours.
- Extraordinary, rare circumstances (major disasters, public health emergencies) may briefly strain schedules, but programs are still expected to adjust and correct as soon as feasible.
Repeated or predictable 80+ hour weeks across a rotation or year indicate non-compliance—not an exception.
4. What should I do if my program doesn’t accurately track or report work hours?
You can:
- Maintain your own detailed log of shifts and hours as evidence.
- Compare your records with what’s recorded in the official duty hour system.
- Discuss discrepancies with your chief residents or program director.
- If the system doesn’t allow accurate tracking—or if you’re discouraged from honest reporting—bring the issue to your GME office or use anonymous reporting channels.
Transparency and accuracy in duty hour reporting are essential to both Resident Well-being and Patient Safety.
5. How can I advocate for better schedules without being labeled “unprofessional” or “not a team player”?
Professional advocacy focuses on data, safety, and solutions, not complaints. To advocate effectively:
- Present specific examples and patterns, not vague dissatisfaction.
- Emphasize concern for patient safety, your ability to learn, and team well-being.
- Suggest possible solutions (e.g., redistribute cross-cover, add float coverage, improve triage).
- Use neutral, respectful language and be open to collaborative problem-solving.
Programs increasingly recognize that sustainable Work Hour Regulations and Resident Well-being are integral to professional behavior—not opposed to it.
Residency Training will always be demanding, but it does not need to be unsafe or unsustainable. Understanding ACGME Work Hour Regulations, monitoring your own schedule, and knowing how to raise concerns are essential skills for modern physicians. By ensuring your program maintains ACGME Compliance and prioritizes Resident Well-being, you are not only protecting yourself—you are actively contributing to a safer, higher-quality environment for your patients and colleagues.



















