Introduction: Are You Overworking in Residency?
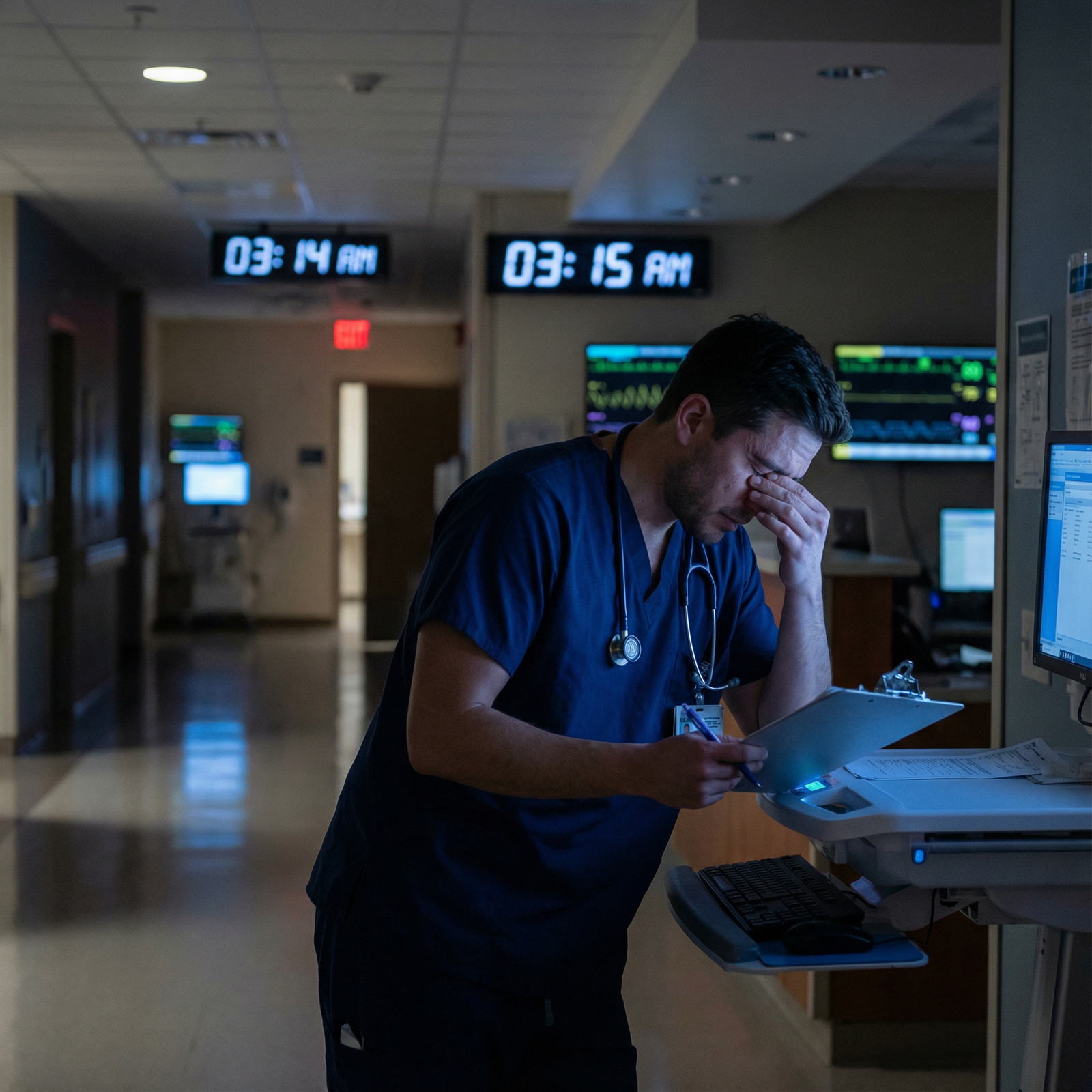
Residency is often described as the most demanding phase of medical training. You’re finally practicing as a physician-in-training, carrying real responsibility for patient care, studying for boards, and trying—often unsuccessfully—to maintain a life outside the hospital. In this high-pressure environment, it can be hard to know where the line is between “working hard” and “overworking.”
That’s where residency duty hour limits come in.
Residency duty hour regulations were created to protect both residents and patients. Yet many residents only have a vague understanding of the rules, or feel guilty about following them. Some quietly exceed limits because “everyone does it,” or because they worry it will make them look less committed.
Understanding these limits—and using them strategically—is essential for:
- Preventing burnout
- Protecting your mental and physical health
- Preserving patient safety
- Maximizing your learning during medical training
This guide breaks down what residency duty hour limits actually are, why they exist, how overworking harms you and your patients, and practical strategies to stay within limits while still being a strong, reliable team member.
What Are Residency Duty Hour Limits?
Duty hour limits are rules that govern how much residents can work, how long they can be continuously on duty, and how much time off they must receive. In the United States, these are set by the Accreditation Council for Graduate Medical Education (ACGME), which accredits residency programs.
Before these rules, residents sometimes worked 100+ hours per week with minimal days off. Research, tragic patient outcomes, and high-profile cases of medical errors prompted a shift toward regulating work hours as a central part of patient safety and burnout prevention.
Core ACGME Duty Hour Regulations
While details can vary slightly by specialty (particularly in surgical programs), the core rules in most ACGME-accredited programs include:
Maximum Weekly Hours
- Residents must not work more than 80 hours per week, averaged over a 4-week period.
- This includes all in-house clinical duties, conferences, and moonlighting that occurs within the sponsoring institution.
Daily Duty Period Limits
- Most residents cannot be scheduled for more than 24 consecutive hours of in-house clinical duties.
- An additional 4 hours may be used for transitions of care, education, or documentation, but not for new patient admissions or procedures.
- Some specialties have more specific nuances (e.g., surgical programs), so always confirm with your program’s written policy.
Time Off Between Shifts
- Residents should have at least 8 hours off between scheduled duty periods.
- Programs are strongly encouraged to allow 10 hours off whenever possible, to promote adequate rest and recovery.
Mandatory Time Off Each Week
- Residents must receive one day (24 consecutive hours) free of all clinical duties every 7 days, averaged over 4 weeks.
- “Off” means truly off: no in-house call, telemedicine coverage, or mandatory academic activities unless explicitly voluntary.
In-House Call and Night Float
- In-house call should occur no more frequently than every third night, when averaged over 4 weeks.
- Night float systems must still comply with overall weekly hours and rest requirements.
Moonlighting Restrictions
- Moonlighting counts toward the 80-hour weekly limit.
- Programs must ensure moonlighting does not interfere with residents’ well-being, performance, or patient safety.
Your program is required to give you a written policy outlining how these rules are applied locally and how to report concerns confidentially.
Why Understanding the Details Matters
Knowing the rules does more than help you avoid trouble with accreditation:
- It allows you to advocate for your own well-being without guessing what is “allowed.”
- It equips you to speak up if your schedule consistently violates regulations.
- It helps you recognize when your fatigue is not a personal failure but a system-level problem that needs to be addressed.

Why Duty Hour Limits Matter for Patient Safety and Resident Well-Being
Duty hour regulations are not about making residency “easy.” They are about making it sustainable and safe—for residents and for the patients who rely on them.
1. Patient Safety: Fatigue as a Risk Factor
Numerous studies in medical training and high-risk industries (aviation, transportation) show that fatigue impairs performance in ways similar to alcohol:
- Slower reaction times
- Reduced attention and vigilance
- Poorer situational awareness
- Impaired decision-making and problem-solving
In the clinical setting, this fatigue translates directly into:
- Diagnostic errors (missing subtle findings, anchoring on an initial impression)
- Medication errors (wrong dose, drug, route, or patient)
- Incomplete handoffs and communication failures
- Delayed recognition of patient deterioration
When residents work beyond safe limits, the risk of preventable harm increases. Duty hour limits are therefore as much a patient safety intervention as a resident wellness initiative.
2. Burnout Prevention and Mental Health Protection
Burnout is characterized by three core dimensions:
- Emotional exhaustion
- Depersonalization (becoming cynical, detached, or numb)
- Reduced sense of personal accomplishment
Surveys have consistently shown 40–60% of residents experience significant burnout symptoms at some point during training. Contributing factors include:
- Chronic sleep deprivation
- Long work hours with limited control over schedule
- Moral distress and emotional burden of patient care
- High administrative load on top of clinical responsibilities
Chronic overwork also increases risk of:
- Depression and anxiety
- Substance misuse
- Relationship difficulties
- Thoughts of self-harm or suicide
Duty hour regulations alone do not “fix” burnout, but they are a necessary baseline. They set a minimum safeguard so that other wellness efforts—mentorship, peer support, access to counseling, and culture change—have a chance to work.
3. Protecting Your Learning and Long-Term Career
Residency is not just a job; it is a structured period of intensive medical training. You are expected to:
- Build clinical decision-making skills
- Develop procedural competence
- Learn to manage complex teams and systems of care
- Absorb large amounts of didactic and self-directed learning
When you are profoundly sleep-deprived:
- Memory consolidation and retention are impaired
- It is harder to integrate new information from conferences and reading
- You may avoid complex tasks, procedures, or conversations simply because you’re too tired to fully engage
Staying within duty hour limits allows you to be alert enough to learn from your cases, reflect on mistakes, and steadily grow into an independent physician.
The Real Risks of Overworking in Residency
Despite clear policies, many residents feel internal or external pressure to exceed duty hour limits—staying late to “help out,” finishing “just one more note,” or taking on extra calls. Over time, this pattern becomes normalized, and residents may not recognize how harmful it is.
1. Burnout, Moral Injury, and Mental Health Consequences
Consistently working beyond duty hour limits accelerates burnout and can also contribute to moral injury—the distress caused when you feel unable to provide the care you know patients deserve because of systemic or situational constraints.
Common signs that overworking is taking a toll:
- You dread going to work, even on rotations you used to enjoy
- You feel emotionally numb or detached in patient interactions
- Small frustrations trigger outsized anger or tears
- You’re relying increasingly on caffeine, alcohol, or other substances to cope
- Your non-medical relationships are deteriorating because you’re always exhausted or unavailable
Ignoring these signs in the name of “pushing through” can have serious long-term consequences for your mental health and your career.
2. Increased Risk of Medical Errors and Near Misses
No one enters residency planning to cut corners, but excessive fatigue makes it far more likely:
- Skipping full chart reviews due to time pressure
- Misreading lab results or imaging reports
- Forgetting to follow up on critical pending tests
- Overlooking drug interactions or contraindications
Clinically, this may look like:
- A septic patient whose deterioration is noticed too late
- An insulin order written incorrectly in a rush
- A key piece of the history never obtained because the resident is thinking about the 15 other tasks waiting
When these incidents occur under conditions of overwork, the system—not just the individual—has failed. Duty hour limits are designed to reduce the frequency of such risky conditions.
3. Legal, Accreditation, and Professional Consequences
Continual violation of duty hour policies can have institutional and personal repercussions:
- ACGME citations for the program, which can affect accreditation status
- Institutional investigations and mandated remediation of scheduling patterns
- Potential disciplinary actions if residents or faculty intentionally falsify reported hours
- Increased liability risk if adverse events are linked to known overwork or misreported duty hours
Residents sometimes fear that honest reporting will harm their program. In fact, accurate reporting is required and is the primary way programs and accrediting bodies can identify and fix unsafe systems.
Practical Strategies to Manage Duty Hours and Workload
Adhering to duty hour limits does not mean being less dedicated. It means working smarter, not just longer, and engaging your team and system in a more sustainable way.
1. Time Management Tactics for Residents
Prioritize Clinically and Logically
- Identify “must-do” tasks at the start of each shift: urgent lab reviews, critical follow-ups, unstable patients.
- Use a simple system (e.g., “A/B/C” or “stat/soon/can wait”) for your task list.
- Reassess priorities after major events (new admission, rapid response, code).
Batch and Streamline Tasks
- Group similar tasks: write all discharge summaries together; place multiple orders in a single charting session.
- Use templates and macros for common notes to save documentation time.
- Delegate appropriately to nurses, case managers, or ancillary staff when within their scope.
Protect Transitions and Sign-Out
- Start preparing sign-outs well before the end of your shift.
- Use structured handoff tools (e.g., I-PASS) to reduce missed information.
- Avoid starting non-urgent new tasks in the final 30–45 minutes of your scheduled time.
2. Communicating Early and Honestly
Open communication is essential for staying within duty hour limits without compromising patient care.
With Attendings and Fellows
- Inform them early in the day if you anticipate hitting hour limits: “I’m at 72 hours this week before today’s shift; I want to make sure we plan appropriately.”
- Ask for help in redistributing work or safely transitioning care if your shift end is approaching.
- Frame it as a patient safety and compliance issue, which it is—not as a personal failing.
With Co-Residents and the Team
- Normalize checking in with each other: “How are your hours this week?”
- Support colleagues in signing out on time when they are near their limits.
- Create a team culture where leaving on time when able is celebrated, not shamed.
3. Self-Care That Actually Fits Residency Reality
Self-care in residency must be practical and realistic. You may not have an hour for the gym every day, but small, consistent practices matter.
Physical Health
- Protect at least some consistent sleep window even on tough weeks (e.g., 4–5 hours anchored at a similar time).
- Keep easy snacks (nuts, granola bars, fruit) in your bag to avoid going 8+ hours without food.
- Use stairs or short walks between tasks as micro-exercise.
Mental and Emotional Health
- Schedule brief check-ins with people who ground you (family, partners, friends)—even 5–10 minutes by text or phone.
- Use institutional counseling or wellness resources proactively, not only in crisis.
- Consider brief grounding strategies you can do at the workstation (e.g., box breathing, 2-minute mindfulness) between stressful encounters.
4. Know Your Rights and Your Reporting Options
Understanding your program’s process is part of professional responsibility.
- Review your institution’s GME handbook and duty hour policy annually.
- Learn how to report duty hour violations—usually through a confidential online system or scheduled GME surveys.
- Use anonymous ACGME surveys honestly; they carry weight in program review.
You are not “weak” for needing rest. You are fulfilling a core professional obligation to protect patients by protecting the clinicians who care for them—including yourself.

Frequently Asked Questions About Residency Duty Hour Limits
1. What should I do if my residency program routinely exceeds duty hour limits?
Start by documenting your experiences:
- Keep a personal log of start and end times, calls, and actual workload.
- Compare your hours to the ACGME rules and your program’s written policy.
Then:
- Discuss with a trusted chief resident or faculty mentor to get perspective and guidance.
- Use official channels (your program coordinator, program director, or GME office) to raise concerns professionally.
- If issues are persistent and unresolved, use confidential ACGME reporting mechanisms (e.g., ACGME Resident/Fellow Complaint system or ACGME surveys).
ACGME and institutional GME offices take these concerns seriously because they directly affect patient safety, burnout prevention, and accreditation.
2. Can I be punished for honestly reporting my duty hours?
Programs are required to encourage accurate duty hour reporting. Honest reporting:
- Should not result in punitive action against you when you are following guidance.
- Helps programs identify systemic problems and fix them before accreditation issues arise.
If you ever feel threatened or retaliated against for accurate reporting, that itself is a serious violation and should be reported to your GME office or the ACGME.
3. Are there specific consequences for my program if duty hour rules are violated?
Yes. When patterns of violation are identified, possible consequences include:
- Citations from the ACGME requiring formal corrective action plans
- Focused or site-visit reviews of the program
- Potential impact on accreditation status if problems are severe or persistent
For residents, there may be:
- Adjustments in scheduling systems (e.g., more night float, additional residents)
- Required educational interventions around time management or wellness
The goal is not punishment, but systemic correction to ensure safe medical training and patient care.
4. How can I accurately track my hours without adding more work to my plate?
Simplify your tracking process:
- Use your institution’s duty hour logging system (e.g., MedHub, New Innovations) regularly—log in small chunks rather than all at once at month’s end.
- Set a daily or post-shift reminder on your phone to quickly record start/end times.
- If the system allows, add brief notes for context (e.g., “Stayed late for code; hours >80 this week”).
The few minutes spent tracking accurately can prevent larger problems later—for you and for your program.
5. How do I balance learning opportunities with staying within duty hour limits?
This is a common tension. Some tips:
- Be selective but strategic: prioritize high-yield learning (unique procedures, rare cases, critical conversations) over staying just to “hang out” when exhausted.
- Ask attendings to schedule teaching and feedback earlier in the day whenever possible.
- If you are near your duty hour limits, discuss alternatives: observing a similar case later in the rotation, simulation lab sessions, or reviewing de-identified case materials.
Your learning is best when you are alert, engaged, and emotionally present. Sometimes the most professional choice is to rest now so you can learn better tomorrow.
Closing Thoughts: Protecting Yourself and Your Patients
Residency will likely be one of the most challenging periods of your life, but it should not be a test of how much chronic sleep deprivation and overwork you can endure. Duty hour limits exist because:
- Fatigued residents make more errors, putting patients at risk.
- Overwork accelerates burnout, depression, and moral injury.
- Sustainable medical training requires balancing service with education and self-preservation.
Understanding residency duty hour limits—and using them—does not make you less dedicated. It makes you a more responsible physician in training, capable of:
- Showing up for your patients with attention and compassion
- Preserving your own mental and physical health
- Building a long, meaningful career in medicine rather than burning out early
Advocate for yourself and your colleagues. Speak up when systems are unsafe. Support a culture where signing out on time when appropriate, taking days off, and accurately logging hours are seen as professional, not problematic.
In doing so, you protect not just your own well-being, but also the safety and dignity of the patients you serve.



















