
Introduction: Why Smart Systems for Patient Records Matter in Residency
Residency is a high-pressure environment: rapidly changing clinical situations, rotating services, new EHR Systems to learn, and constant demands on your time and attention. In the middle of all this, managing Patient Records can feel like just one more task on an overflowing list.
But how you organize your documentation isn’t just an administrative concern—it directly affects:
- The safety and quality of patient care
- Your efficiency and burnout risk
- How attendings and program leadership perceive your reliability
- Your ability to meet legal and regulatory standards in any Healthcare Organization
Developing smart, sustainable documentation strategies early in your medical residency can save you hours each week, reduce errors, and give you more cognitive bandwidth for actual clinical reasoning. This guide expands on core organizational hacks and turns them into a coherent system you can adapt to any rotation or EHR platform.
The High Stakes of Organized Patient Records in Residency
Clinical, Legal, and Professional Implications
Before jumping into hacks, it’s worth grounding yourself in what’s at stake when managing patient records.
Improved Patient Care and Safety
- Organized, up-to-date records mean fewer missed abnormal labs or imaging results.
- Clear documentation helps the on-call team quickly understand what’s going on at 3:00 a.m.
- A well-structured note allows future providers to see what you were thinking and why specific decisions were made.
Regulatory and Legal Compliance
- Legally, if it isn’t documented, it didn’t happen.
- Accurate documentation protects you and your Healthcare Organization in audits, quality reviews, or medicolegal cases.
- Many institutions track documentation completeness and timeliness as part of your performance metrics.
Streamlined Workflow and Time Savings
- Poorly organized records lead to “chart spelunking” — digging through disorganized notes, scanned PDFs, or misfiled documents.
- A small investment in upfront organization can save 10–30 minutes per day, which adds up over weeks of call and nights.
Enhanced Team Communication
- Clear, concise, and consistent documentation supports handoffs, day–night transitions, cross-cover, and interdisciplinary care.
- Nurses, consultants, and therapists rely on your notes to coordinate care and avoid conflicting instructions.
Organized patient records aren’t optional “extra credit”—they are a core competency of being a safe, efficient resident.
Building a Digital Foundation: Tools and EHR Strategies
Choosing and Mastering Core Digital Management Tools
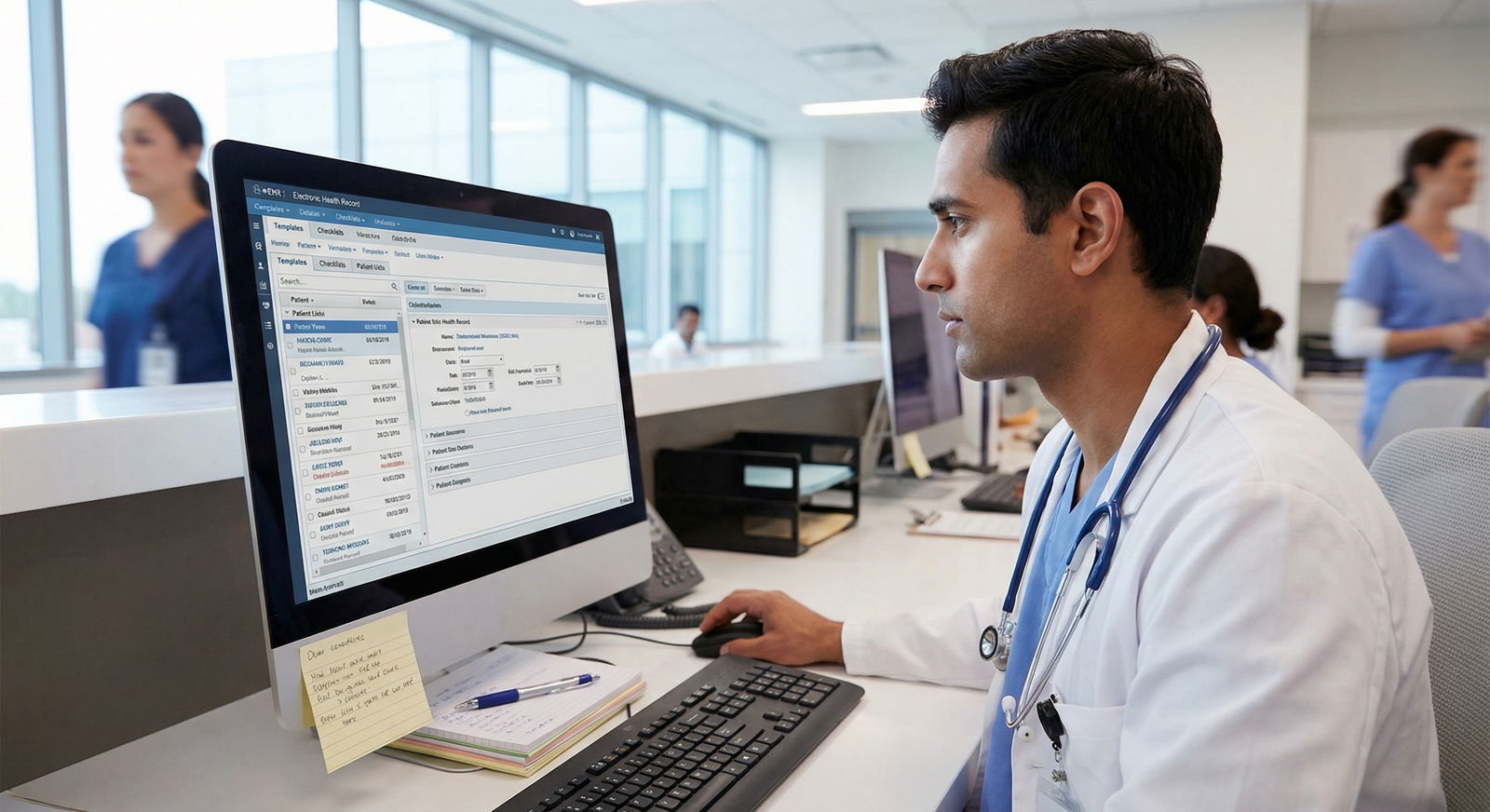
In modern training environments, EHR Systems are the backbone of patient record management. You usually don’t get to choose the main EHR, but you can choose how effectively you use it—and what supplemental tools you keep for yourself.
Common institutional EHR platforms include:
Epic
- Powerful search, smart phrases, and customization options
- Supports specialty-specific templates and flowsheets
- In-basket tools to triage messages, lab results, and consults
Oracle Cerner
- Strong interoperability and cross-system data sharing
- Customizable views for labs, medications, and problem lists
- Order sets and pathways to standardize care
Meditech
- Frequently used in smaller hospitals and community settings
- Simpler, streamlined interface
- Good for building core habits that translate to other systems
Your goal is to become intentionally proficient rather than just “getting by.” Schedule time early in a rotation to:
- Ask a super-user (senior resident, fellow, or nurse) to walk you through their shortcuts
- Shadow how they handle pre-rounding, orders, and notes in the EHR
- Bookmark or save key patient lists, default note templates, and order sets
Supplemental Personal Tools (Used Carefully and Securely)
While the EHR is the official source of truth, supplemental tools can help you organize your workflows—not patient identifiers. Always follow HIPAA and institutional policies.
Some privacy-safe, high-yield tools:
Notion
- Great for creating personal reference pages (e.g., “ICU vent settings,” “ACS pathway,” “Stroke call algorithm”)
- Use for checklists and workflow guides, not for identifiable patient data
Evernote or OneNote
- Useful for quick general notes, study plans, and templates of phrases you commonly use in notes
- Maintain a library of non-identifiable documentation tips and teaching pearls
Task Managers (e.g., Todoist, TickTick, Apple Reminders)
- Ideal for non-patient specific tasks: call schedules, deadlines, conference prep, board study
Key principle: Anything with Patient Records or identifiable data belongs in the EHR or your institution’s secure systems, never on personal apps or devices unless officially sanctioned and encrypted.
Structuring Information: Naming, Color Coding, and Visual Cues
Even within standardized EHR platforms, your personal organization choices can dramatically affect speed and error rates.
Consistent Digital “Naming” and Structuring Strategies
Most residents don’t “name files” in the traditional sense within EHRs, but they do structure information in predictable ways that mimic a naming convention. Think about:
Problem List Discipline
- Keep problem lists clean, current, and prioritized.
- Consolidate duplicate entries (e.g., “Hypertension” vs. “Uncontrolled HTN”).
- Use specific, actionable language: “Acute hypoxic respiratory failure – improving” rather than just “Respiratory distress.”
Standardized Note Titles
Where you can influence naming, use consistent patterns like:- “H&P – [Service] – [Attending Last Name]”
- “Daily Progress Note – ICU – POD#X”
- “Discharge Summary – [Diagnosis Short Label]”
This improves searchability and makes it easier for consultants and auditors.
Local File Naming (for Non-Clinical Files)
For lecture slides, protocols, or reference materials (never PHI), adopt a consistent scheme such as:Cardiology_HeartFailure_ManagementProtocol_2025-02ICU_SedationDelirium_BundleChecklist_v3
This makes it much easier to search your own knowledge base over time.
Color-Coding Strategies in Clinical Practice
Many EHR Systems and productivity tools allow you to use colors as fast visual cues. Used consistently, they function like a second language in your workflow.
In the EHR:
Patient Lists
- Red or high-alert icon: critical patients, unstable vitals, or recent rapid response
- Yellow: undergoing active workup with pending critical results
- Green: stable, likely discharge candidates
Orders and Results
- Use built-in flags or color codes for abnormal labs that need follow-up
- Highlight stat or time-sensitive imaging studies
In-Basket / Message Queues
- Color-tag messages requiring action today vs. this week vs. just FYI
In Personal Systems (Non-PHI):
- Rotation-Based Color Coding
- Blue: inpatient wards
- Green: clinic
- Red: ICU / ED
- Purple: night float / cross-cover
Consistent visual cues reduce cognitive load and help you rapidly triage what needs attention first.
Checklists, Templates, and Macros: The Core of Efficient Documentation
Designing High-Impact Checklists for Patient Records
Checklists are one of the most powerful documentation strategies you can build into your residency life. They reduce errors, standardize processes, and offload memory.
1. Admission Checklist
A robust admission checklist might include:
History and Examination
- Chief complaint clearly stated
- Onset, duration, and key associated symptoms
- Relevant PMH, PSH, meds, allergies, social and family history documented
Orders and Initial Management
- Admission orders set (level of care, code status, isolation if needed)
- Labs, imaging, and consultations placed
- Home meds reconciled and critical meds continued or held
Risk and Safety Items
- VTE prophylaxis ordered or contraindication documented
- Pressure ulcer risk, falls risk, delirium risk noted
- Advance directives / surrogate decision-maker identified if applicable
Create this as a mental or written checklist you run through on every admission, or build it into a pre-populated note template.
2. Daily Chart Review / Progress Note Checklist
For each patient you see daily:
- Review overnight events, vitals, I/Os, relevant labs, imaging
- Update problem list and impression/plan problem by problem
- Confirm active medications, including antibiotics, anticoagulants, and high-risk drugs
- Reassess need for lines, drains, catheters, restraints, and telemetry
- Identify discharge barriers and potential date
This checklist can be integrated into your note template—each problem heading becomes a prompt.
3. Discharge Summary Checklist
High-quality discharge documents are critical for transitions of care:
- Final working diagnosis and significant comorbidities
- Brief but clear hospital course organized chronologically or by problem
- Clear medication list with indications and changes explained
- Follow-up appointments: when, where, and with whom
- Pending labs or results and who will follow them
- Explicit return precautions and patient/family instructions
Many programs track readmissions and adverse events linked to poor discharge documentation, so this is a high-yield area for meticulousness.
Templates and Macros: Work Smarter, Not Sloppier
Templates and macros (smart phrases, dot phrases, or text expanders) can be your best friends or your worst enemies depending on how you use them.
Best practices:
- Start with your institution’s standard templates, then refine them to match your thinking pattern.
- Keep templates lean: they should guide your note, not produce pages of boilerplate that obscure key information.
- Build macros for:
- Common phrases (e.g., “Discussed risks, benefits, and alternatives of the procedure including bleeding, infection, and anesthesia risks; patient voiced understanding and agreed to proceed.”)
- Standard counseling statements (e.g., smoking cessation, anticoagulation teaching)
- Physical exam blocks you frequently document (but always edit to reflect actual findings).
Never paste in content that doesn’t apply to the specific patient. Inconsistent or incorrect macros are a frequent source of attendings’ frustration and can be dangerous medicolegally.
Maintenance Mode: Review, Cleanup, and Continuous Improvement
Scheduling Regular Record Review and Cleanup
Just like your living space, your digital workspace and documentation habits get messy over time. Plan routine maintenance instead of waiting for chaos.
Weekly or biweekly documentation reset:
- Clean up active patient lists (remove discharged patients, archive old lists)
- Review unresolved tasks in the EHR (unsigned notes, incomplete orders, unacknowledged results)
- Identify and correct charting errors or outdated problem list items
End-of-rotation cleanup:
- Archive or rename personal reference documents for that service
- Update your personal templates based on what actually worked
- Note any EHR tricks or pitfalls to share with incoming interns/residents
This repeated reflection builds a feedback loop that continuously refines your organizational system.
Continuous Training and Peer Feedback
EHR Systems and institutional policies evolve. Staying updated is part of your professional development.
Formal Workshops and Training Sessions
- Attend refresher sessions offered by IT or clinical informatics teams.
- Ask questions specific to your service (ICU flowsheets, ED triage, oncology order sets).
Peer Learning
- Observe how efficient seniors manage notes and patient lists.
- Ask co-residents to share their best templates and smart phrases.
- Offer to show interns your systems; teaching often clarifies and improves your own methods.
Quality Improvement (QI) Mindset
- Track one or two metrics you care about (e.g., “all my discharge summaries completed within 24 hours,” “no unsigned notes at end of week”).
- Adjust your workflows if you consistently miss your targets.

Case Example: Transforming a Chaotic Service into an Organized System
Imagine a busy general surgery service in a large Healthcare Organization. The problems will sound familiar:
- Post-op notes written hours late or missing critical details
- Discharge instructions inconsistent or incomplete
- Cross-cover pages overnight about questions that could have been answered by better documentation
The residency leadership decides to systematize documentation and Patient Records management.
Step 1: Standardized EHR Templates
They create service-wide templates for:
- Pre-op H&P with a built-in risk checklist (cardiac, pulmonary, thromboembolism)
- Post-op progress notes aligned with ERAS or standard recovery protocols
- Discharge summaries with mandatory fields for follow-up and pending results
Residents are encouraged to personalize these—but not to reinvent the wheel completely.
Step 2: Checklist Integration
Each template incorporates mini-checklists:
- Post-op note: pain control, DVT prophylaxis, diet, mobilization, drains, lines, antibiotics stop date
- Discharge summary: specific wound care instructions, activity restrictions, warning signs
These checklists significantly reduce omissions and nursing phone calls for clarifications.
Step 3: Color-Coded Patient Lists
The team builds a shared EHR patient list with color coding:
- Red: patients POD#0–1 or unstable
- Yellow: POD#2–3 or with active issues
- Green: likely discharge candidates
Morning huddles use this list to prioritize rounds and identify discharge planning tasks early.
Step 4: Ongoing Training and Feedback
- Monthly 20-minute lunch sessions cover new EHR features and documentation pitfalls.
- Residents anonymously submit “documentation fails” (e.g., incorrect copied text, missing DNR documentation) for group learning.
- The chief resident reviews a small sample of discharge summaries each month and provides constructive feedback.
Within a few months, the program sees:
- Fewer readmissions related to unclear instructions
- Shorter time from “medically ready” to actual discharge
- Residents reporting less stress around notes at the end of the day
The transformation didn’t require new technology—just intentional design of systems and consistent habits.
FAQs: Patient Records, EHR Systems, and Documentation Strategies in Residency
1. How can I keep up with documentation during a hectic call shift without falling behind?
- Pre-build concise templates for H&Ps and progress notes before your shift.
- Prioritize real-time or near-real-time documentation for critical events (codes, procedures, high-risk conversations).
- Use quick note stubs during peak chaos (e.g., brief bullet points) and expand them as soon as you catch a lull.
- At minimum, aim to complete essential notes before leaving the hospital to avoid memory lapses and after-hours burnout.
2. What should I do if my attending prefers a very different documentation style than my templates?
- Ask explicitly what they value: shorter versus longer notes, problem-based versus system-based, particular phrases or structures.
- Create an “Attending-specific” variant of your template for that rotation.
- Maintain your core organization system but flex details to match expectations—it’s part of professional adaptability.
3. How do I avoid copy-paste errors and “note bloat” while still being efficient?
- Use templates and macros as prompts rather than as full pre-written notes.
- Always reread your note from top to bottom before signing, scanning for contradictions (e.g., “no chest pain” in HPI but “ongoing chest pain” in assessment).
- Limit copying forward to factual data that truly hasn’t changed (e.g., past medical history), and always update labs, exam findings, and assessment/plan.
4. Are personal apps like Notion or Evernote safe for anything related to patient care?
- Do not store identifiable patient information or screenshots from EHRs in personal apps unless explicitly allowed and encrypted by your Healthcare Organization.
- Use these tools instead for generic protocols, study materials, personal to-do lists, and non-PHI templates or phrases.
- When in doubt, check with your institution’s compliance or IT department.
5. What’s one high-yield change I can make this week to improve my documentation organization?
- Implement a simple daily “documentation shutdown” routine:
- Review your patient list for any missing notes or unsigned documents
- Check your in-basket/messages for unresolved items
- Clean your problem lists on 1–2 patients each day
- Reflect on what slowed you down and tweak one small part of your system
This 10–15 minute routine can rapidly improve both efficiency and safety.
By approaching Patient Records and EHR Systems with deliberate, well-designed documentation strategies, you can turn a major residency stressor into a professional strength. Smart systems don’t just keep charts neat—they protect patients, support your team, and free up your most valuable resource: your clinical judgment and time.



















