
Understanding the Landscape: What Makes EM Program Research Different for DO Graduates
Researching emergency medicine residency programs as a DO graduate requires a tailored strategy. Emergency medicine (EM) is competitive and historically has had variability in how programs view osteopathic applicants. While the single accreditation system has unified ACGME and former AOA programs, not all residencies are equally DO-friendly.
Before diving into how to research residency programs, it’s crucial to understand the unique factors that shape a DO graduate’s EM match prospects:
- USMLE vs COMLEX: Some programs still “prefer” or require USMLE scores, even though COMLEX is accepted by ACGME. This can significantly affect your list.
- Former AOA vs historically ACGME programs: Programs with osteopathic roots often have more DO faculty, leadership, and alumni—frequently translating to a stronger DO culture.
- Program competitiveness: EM overall has become tighter in certain cycles, so choosing an appropriate mix of reach, target, and safety programs is essential.
- Your profile as a DO applicant:
- COMLEX (and possibly USMLE) scores
- EM clerkship grades and SLOEs (Standardized Letters of Evaluation)
- Research, leadership, volunteer work
- Geographic preferences and constraints
Your program research strategy should be intentional, data-driven, and realistic. The goal is not just to “get a list,” but to build a customized, evidence-based list that maximizes your chances in the EM match while aligning with your career goals and personal needs.
In the sections below, we’ll walk step-by-step through a comprehensive approach to researching and evaluating emergency medicine residency programs as a DO graduate.
Step 1: Clarify Your Priorities as a DO Applicant in Emergency Medicine
Before pulling up any databases, you need clarity on what matters most to you. This will guide how to research residency programs efficiently instead of getting overwhelmed by hundreds of EM options.
1. Clinical and Career Priorities
Ask yourself:
- Do you want academic EM with research, fellowships, and teaching responsibilities?
- Or are you more drawn to a community EM environment with high-volume, hands-on clinical work?
- Are you strongly interested in a future fellowship (toxicology, ultrasound, EMS, critical care, pediatric EM, global health, administration)?
If you’re fellowship-minded, you may prioritize:
- Programs with multiple EM fellowships
- Strong research infrastructure and scholarly output
- A track record of graduates matching into fellowships
If you’re clinically focused, you may look for:
- High ED volume and trauma exposure
- Diverse pathology (rural vs urban considerations)
- Breadth of procedures and autonomy
2. DO-Specific Considerations
As a DO graduate, integrate these into your self-assessment:
- Board exams taken:
- COMLEX only
- COMLEX + USMLE
- Strength of scores:
- Are your scores above, at, or below the average for matched EM applicants?
- Osteopathic identity:
- Do you value osteopathic recognition (OR) programs that formally incorporate OMT and osteopathic principles?
- Do you prefer a program with many DO residents/faculty?
Programs differ widely in their familiarity with COMLEX and their historical patterns with DO graduates. Your program research strategy must incorporate this from the start.
3. Personal and Lifestyle Priorities
These are not secondary; they dramatically influence your day-to-day life during residency:
- Geography (family needs, cost of living, climate, desired city size)
- Support systems (partner’s job, children’s schools, proximity to relatives)
- Wellness culture and schedule (shift patterns, night coverage, vacation structure)
- Diversity, inclusion, and program culture
Create a “Priority Map” with 3–5 non-negotiables and 5–10 “nice-to-haves.” This will help you rapidly filter programs later.
Step 2: Build a Master List Using Reliable Databases and DO-Friendly Resources
Once you know your priorities, you can systematically generate a long list of potential programs to investigate.
1. Start with Official Databases
Use multiple sources to avoid missing programs:
FREIDA (AMA Residency & Fellowship Database)
Filter by:- Specialty: Emergency Medicine
- Program type (university-based, community-based, etc.)
- Geographic region
- Program size
NRMP and ACGME Program Information
While NRMP gives you match statistics and participating programs, ACGME offers details like:- Accreditation status
- Osteopathic Recognition status
- Program size and duration
ERAS Program Directory
Pay attention to:- Program “Requirements” tab (USMLE vs COMLEX expectations)
- Notes on EM letters/SLOEs, visa policies, and additional requirements
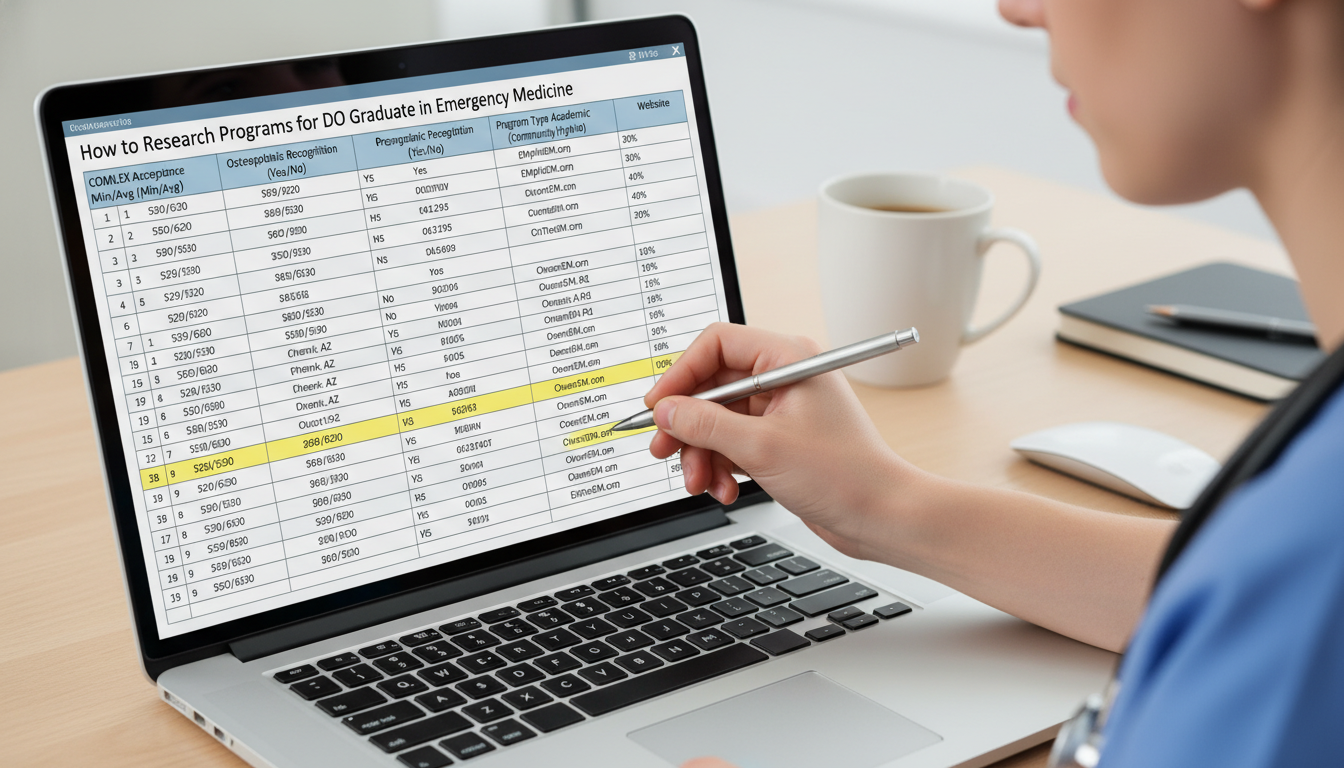
Create an initial spreadsheet with columns for:
- Program name
- City/state
- University vs community
- Number of residents per year
- Osteopathic Recognition (Y/N)
- COMLEX accepted (Y/N) and USMLE requirement
- Website link
2. Identify Historically DO-Friendly EM Programs
To refine your DO graduate residency list:
- Look for Osteopathic Recognition in ACGME data.
- Check program websites for:
- Proportion of DOs in current classes
- Presence of DOs on faculty or in leadership (APD/PD)
- Use:
- EMRA (Emergency Medicine Residents’ Association) resources
- Social media (program Instagram/Twitter/X) showcasing residents—count how many DOs you see
- DO forums (Student Doctor Network, Reddit r/medicalschoolDO, or r/EMresidency) cautiously, focusing on consistent patterns over isolated anecdotes
In your spreadsheet, add columns:
- % DO residents (rough estimate from class photos)
- Former AOA program (Y/N)
- DO-friendly (your rating: High/Moderate/Low)
3. Cross-Check with EM Match Data
To keep your EM match strategy realistic:
- Review NRMP’s “Charting Outcomes in the Match” and specialty-specific data for EM:
- Average Step/COMLEX scores for matched EM applicants
- Match rates by degree type (MD vs DO)
- Number of contiguous EM ranks of matched vs unmatched applicants
- If you have access, use EMRA Match (if maintained) or specialty society tools that list:
- Program features (fellowships, ultrasound, toxicology, etc.)
- Program contact information and unique characteristics
Use this data to mark programs as:
- Reach (stronger-than-your-stats)
- Target (aligned with your stats and profile)
- Safety (slightly below your stats but still solid)
Step 3: Deep-Dive into Each Program: What to Look For and Where to Find It
Now that you’ve built a master list, you need a structured way of evaluating residency programs in more depth. This is where many DO applicants make the mistake of “skimming” instead of truly analyzing fit.
1. Program Website: Your Primary Source
Every emergency medicine residency’s website should be your first stop for detailed evaluation.
Look for:
a. DO and COMLEX Policies
- Explicit statements like:
- “We accept COMLEX and/or USMLE”
- “USMLE strongly recommended for DO applicants”
- “We strongly prefer USMLE scores”
- Current resident bios with degree type (MD/DO)
If the website is vague:
- Assume no clear DO preference, but verify by emailing the program coordinator (politely) if you’re strongly interested.
b. Curriculum and Training Environment Evaluate:
- ED volume and patient mix:
- Annual ED visits
- Trauma level (I/II/III)
- Pediatric exposure (separate children’s hospital or integrated)
- Clinical rotations:
- ICU time, anesthesiology, ultrasound, EMS/flight, trauma surgery
- Ultrasound:
- Formal ultrasound curriculum? Dedicated ultrasound faculty? Fellowship?
- Simulation:
- Regular simulation sessions and procedure labs?
Ask:
“Does this environment support the kind of EM physician I want to become?”
c. Resident Life and Culture Look closely at:
- Resident wellness and mentorship descriptions
- Shift schedules:
- Number of shifts per month
- Length (8, 9, 10, or 12 hours)
- Call responsibilities (if any, for off-service rotations)
- Moonlighting policies for senior residents
Many programs share resident testimonials or “Day in the Life” examples—use these to infer culture and lifestyle.
2. Social Media and Resident-Led Content
Programs often reveal their true personality on social channels:
- Instagram, X/Twitter, TikTok, YouTube
- Look for:
- Team camaraderie
- Diversity
- Wellness activities
- Educational conferences and simulation
- Count how many DOs appear in class introductions and graduation posts.
- Look for:
Pay attention to:
- How they talk about osteopathic residents (if at all)
- Signals of inclusivity and support for different backgrounds
3. Objective Data Sources Beyond Marketing
For deeper evaluating of residency programs:
- ACGME Resident Survey results (if available in summary form or occasionally discussed publicly):
- Satisfaction with education
- Duty hour compliance
- Supervision and feedback
- Program accreditation status:
- Any recent citations or probation issues? (These may sometimes be referenced on ACGME or discussed in rumor mills—confirm with official sources or by asking residents.)
While red flags don’t necessarily disqualify a program, multiple serious concerns should prompt careful consideration.
Step 4: Tailor Your Research Strategy to Your Profile and Goals
A strong program research strategy is customized. Two DO applicants with the same COMLEX score might pursue very different lists depending on geography, family, and career goals.
1. Scenario-Based Examples
Example 1: DO with COMLEX Only, Solid Scores, Fellowship Interest
- Priority: Academic EM, ultrasound and critical care exposure, strong DO support
- Research approach:
- Target former AOA/osteopathic recognition programs at large academic centers.
- Focus on programs explicitly stating they accept COMLEX only.
- Prioritize programs with ultrasound and critical care fellowships.
- EM match strategy:
- Heavy emphasis on DO-friendly academic centers across multiple regions.
- Apply broadly (30–40+ EM programs, depending on competitiveness of your profile and year).
Example 2: DO with COMLEX + USMLE, Average Scores, Strong Geographic Preference
- Priority: Staying near a specific region (e.g., Midwest) for partner/family
- Research approach:
- List all EM programs within a defined radius.
- Stratify: highly DO-friendly vs moderate vs unclear.
- Avoid overloading list with only ultra-competitive “flagship” programs.
- EM match strategy:
- Mix of university-affiliated and community-based EM programs.
- Consider a few out-of-region programs as backup in case primary geographic region is saturated.
Example 3: DO with Below-Average Scores, Strong Clinical Evaluations, and Great SLOEs
- Priority: Maximizing match probability while preserving EM as target specialty
- Research approach:
- Focus heavily on historically DO-friendly programs and smaller community-based residencies.
- Emphasize programs with a track record of holistic review and supportive culture.
- EM match strategy:
- Apply very broadly, including some dual-apply strategies if advised (e.g., prelim year or categorical in another specialty if strongly concerned).
- Communicate with program leadership at EM audition rotation sites; strong SLOEs are especially crucial.
Step 5: Comparing and Ranking Programs: Turning Data into Decisions
Once you’ve gathered information, you must synthesize it. Otherwise, everything blurs and decisions become emotional or random.
1. Create a Structured Scoring System
Design a scoring rubric aligned with your priorities. For each program, you might score (1–5) on:
- DO-friendliness (resident mix, leadership, COMLEX policy)
- Academic opportunities (research, fellowships, scholarly output)
- Clinical exposure (volume, trauma level, pathologic diversity)
- Education quality (conference structure, simulation, ultrasound training)
- Culture and wellness (resident happiness, mentorship, schedule)
- Geographic fit (family, lifestyle, cost of living)
- “Gut fit” (how you feel after deep research or a conversation with residents)
Example:
| Factor | Weight | Score (1–5) | Weighted Score |
|---|---|---|---|
| DO-friendliness | 1.5 | 4 | 6.0 |
| Academic opportunities | 1.2 | 3 | 3.6 |
| Clinical exposure | 1.3 | 5 | 6.5 |
| Culture & wellness | 1.0 | 4 | 4.0 |
| Geographic fit | 1.0 | 2 | 2.0 |
| Gut fit | 1.0 | 4 | 4.0 |
| Total | 26.1 |
You don’t need perfect precision; the goal is to differentiate and make patterns visible.
2. Trimming Your List Before Applying
After scoring:
- Define your target number of applications based on your competitiveness and current EM match climate (your advisor or EM faculty can help tailor this).
- Cut programs that:
- Are obvious poor fits (wrong geography, no DOs, require USMLE when you don’t have it).
- Score clearly lower than others in the same region or category.
You might aim for:
- 10–15 reach programs
- 15–20 target programs
- 5–10 safety programs
Adjust these ranges based on your specific risk tolerance and advisor input.
3. Preparing for Interviews with Your Research
Your research doesn’t end when you submit ERAS. Use your notes to:
- Craft program-specific responses:
- “I’m particularly excited about your ultrasound curriculum and the osteopathic recognition track…”
- Develop intelligent questions:
- “Can you tell me more about how DO residents are integrated here and whether there’s any structured OMT involvement?”
- “What support do residents receive if they want to pursue EMS or critical care fellowship after graduation?”
- Tailor your thank you emails to reflect genuine understanding of the program.

Step 6: Red Flags, Green Flags, and How to Interpret Mixed Signals
While researching, you’ll encounter conflicting information. Learning how to interpret it is a key part of evaluating residency programs.
1. Common Green Flags for DO Graduates in EM
- Clear website language:
“We welcome applications from DO graduates and accept COMLEX and/or USMLE.” - Current residents:
- Multiple DOs in each class
- DOs in chief roles or leadership positions
- Program leadership:
- DO faculty in core faculty or APD/PD roles
- Strong EM education features:
- Weekly protected didactics
- Robust ultrasound and simulation curriculum
- Regular feedback and mentoring structure
- Cultural signals:
- Emphasis on wellness, diversity, and inclusion
- Transparent communication about scheduling and workload
2. Potential Red Flags (Especially for DOs)
- Website states:
- “USMLE required for DO applicants” when you only have COMLEX.
- “No DOs currently in our program” in a region where many DOs are available.
- Vague or evasive responses when you ask about:
- COMLEX score interpretation
- DO match history
- Stories from multiple, unrelated sources about:
- Hostile culture or chronic resident dissatisfaction
- Unresolved ACGME citations or persistent accreditation concerns
A single red flag doesn’t automatically disqualify a program, but consistent patterns across multiple sources should make you cautious.
3. What to Do When Information Conflicts
When you see conflicting information (e.g., website vs rumor vs social media):
- Prioritize official and first-hand sources:
- Program website
- Direct emails with coordinators or residents
- Conversations with alumni from your med school who matched there
- Ask clarifying questions:
- “I noticed your website mentions USMLE scores. How do you consider COMLEX for DO applicants?”
- Document and compare:
- Note discrepancies in your spreadsheet
- Consider whether the inconsistency itself is a concern (e.g., poor communication/organization)
Frequently Asked Questions (FAQ)
1. As a DO, do I need to take USMLE for emergency medicine?
It depends on your EM match goals and the specific programs you’re targeting. Many EM programs do accept COMLEX only, and some are explicitly DO-friendly. However, some historically ACGME academic programs either strongly prefer or require USMLE. If your goal is to keep the broadest possible range of EM programs open—especially highly competitive academic centers—USMLE can be helpful. If you’ve already decided against taking USMLE, focus your program research on those that openly accept COMLEX and have a track record of matching DOs.
2. How many EM programs should I apply to as a DO graduate?
The ideal number varies by cycle and by your competitiveness (scores, SLOEs, grades, geography). Many DO applicants apply to 25–40+ EM programs, with some going higher if they have significant risk factors (lower scores, fewer SLOEs, limited geographic flexibility). Work with your EM clerkship director or advisor to calibrate your numbers using recent EM match data and your individualized risk profile.
3. How can I tell if a program is truly DO-friendly?
Look for multiple converging signs:
- DOs in current and recent residency classes
- DO faculty or leadership (PD/APD)
- Clear acceptance of COMLEX, ideally with explicit mention on the website
- Positive feedback from DO alumni or your school’s graduates
- Absence of “USMLE required” language if you only have COMLEX
You can also ask directly during away rotations or interviews:
“How have DO residents historically done here, and are there any differences in how DO and MD applicants are evaluated?”
4. Should I prioritize former AOA/osteopathic programs for my EM applications?
Former AOA programs and those with Osteopathic Recognition often have a strong osteopathic culture and may be particularly supportive of DO graduates. They can be excellent options, especially if you value OMT, osteopathic philosophy, and a community that understands COMLEX. However, they shouldn’t be your only focus—many historically ACGME EM programs are also supportive and have robust training. A balanced list that includes both former AOA and historically ACGME programs—filtered by DO-friendliness, location, and training quality—is usually the best approach.
By using a structured, data-driven program research strategy tailored specifically to your goals as a DO graduate in emergency medicine, you can move beyond guesswork. Thoughtful program research not only strengthens your osteopathic residency match chances, it also increases the likelihood that you’ll spend your EM training years in a program where you can truly thrive—clinically, academically, and personally.






















