
Understanding Your Position as a DO Graduate with a Low Step Score
Cardiothoracic surgery is among the most competitive specialties in medicine. For a DO graduate with a low Step 1 score, low COMLEX Level 1, or below average board scores, the path can feel almost impossible. It isn’t. It’s harder, narrower, and requires more strategy and persistence—but it is not closed.
A key reality:
Most applicants who successfully match into cardiothoracic surgery residency (either integrated CT surgery or general surgery with later CT fellowship) have very strong academic metrics. But programs also care deeply about:
- Operative potential and technical aptitude
- Work ethic and grit
- Commitment to heart surgery and long-term career goals
- Research productivity and letters of recommendation
- Performance in audition rotations and sub-internships
Your scores are one part of the file—not the entire story. For a DO graduate residency applicant, you must build an application that is so compelling in other domains that programs are willing to look past weaker metrics.
This article focuses on practical, concrete strategies for matching with low scores specifically tailored to:
- DO graduates or DO seniors
- Interested in cardiothoracic surgery or a pathway leading to heart surgery training
- Facing a low Step 1 score / low Level 1 or overall below average board scores
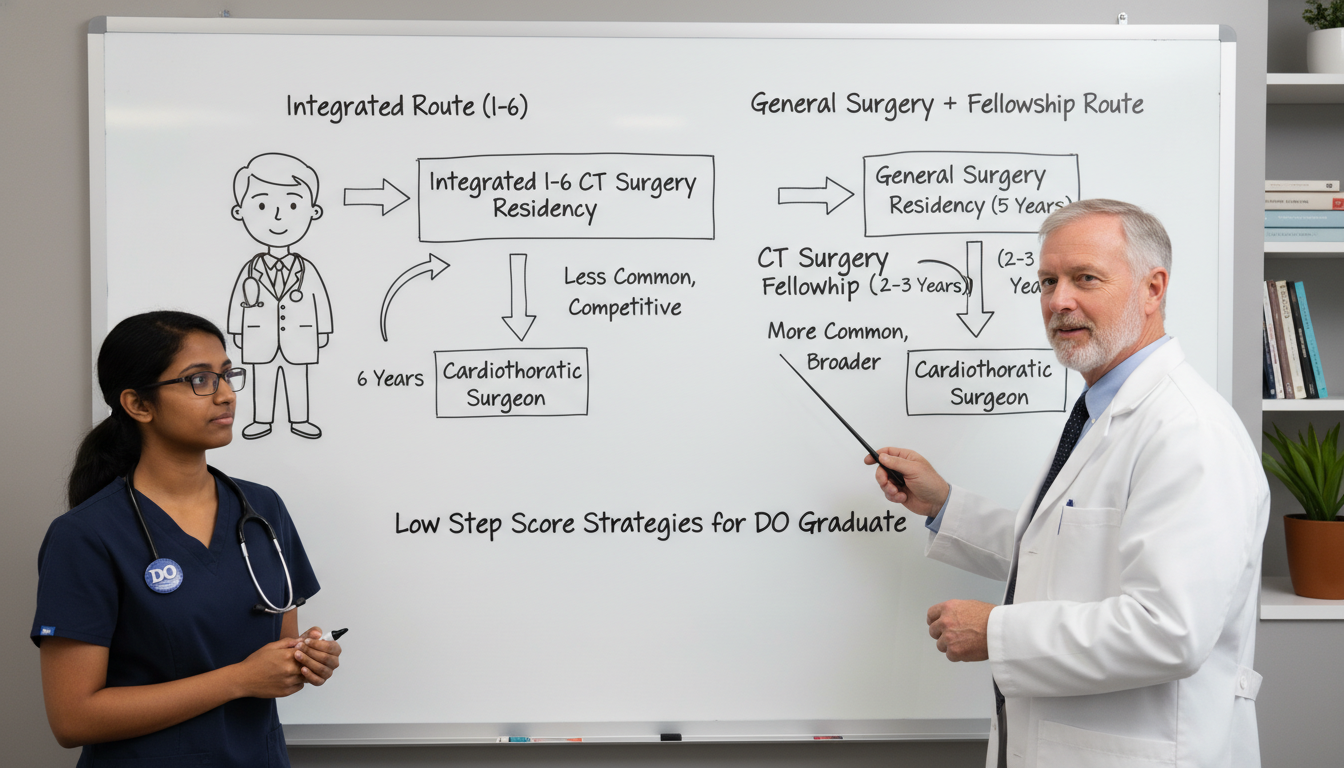
We will address both the integrated CT pathway (I-6) and the more common general surgery → CT fellowship route, with special attention to what is realistically attainable for a DO with weaker exam metrics.
Step 1: Reframe the Goal – Direct CT vs. General Surgery Pathway
Before you commit to a strategy, you need clarity on what “success” actually looks like for you.
1. The Integrated Cardiothoracic Surgery (I-6) Route
I-6 programs accept applicants directly into cardiothoracic surgery residency out of medical school. These spots are extremely limited and highly competitive. Many successful applicants have:
- Top-tier Step and COMLEX scores
- Multiple high-impact CT surgery publications
- Extensive CT research years or dedicated research fellowships
- Strong institutional connections and mentors in heart surgery
For a DO graduate with a low Step 1 score or below average board scores, the I-6 path is not impossible, but it is realistically an uphill battle. You would likely need:
- Substantial CT-focused research productivity (often > 1–2 years)
- Multiple strong letters from well-known cardiothoracic surgeons
- Demonstrated technical interest/skill and clear long-term CT commitment
- Strong Step 2/Level 2 scores to offset earlier performance
If you are early enough in your training and willing to commit to 1–2+ years of research and targeted positioning, you can keep I-6 programs in consideration. But you should also have a parallel, more attainable primary plan.
2. General Surgery → Cardiothoracic Fellowship: A More Realistic Primary Path
For most DO graduates with low Step scores, the safer and more realistic path is:
- Match into a strong general surgery residency (ideally one with robust cardiothoracic exposure)
- Excel as a resident—evaluations, operative skills, research
- Apply to cardiothoracic surgery fellowship during residency
Advantages of this route for DOs with weaker metrics:
- Many more positions nationally in general surgery than in I-6 CT
- Some programs are more holistic and DO-friendly
- Performance as a resident and research trajectory can matter more than your old boards
- You can still build competitive CT credentials over 5 years
The mindset shift:
You are not necessarily “failing” if you do not enter an I-6 program. You are pursuing a more measured, stepwise route to the same end: heart surgery training.
Step 2: Neutralize the Impact of Low Scores Strategically
You can’t change a low Step 1 or Level 1, but you can:
- Limit the damage it does
- Provide counter-evidence of your capability
- Frame the narrative on your terms
A. Strengthen Subsequent Scores (Step 2 CK / Level 2 CE)
If your Step 1 score is low, Step 2 CK and COMLEX Level 2 are your most powerful tools to shift program perceptions.
Goals:
- Aim for a clear upward trend (e.g., Step 1 = borderline, Step 2 CK = solidly above national mean)
- Demonstrate that early struggles were not a fixed limitation but a temporary obstacle
Strategies for a DO with low scores:
- Start Step 2/Level 2 preparation early—at least 4–6 months before the exam
- Use high-yield resources (UWorld, COMBANK/COMQUEST, NBME practice tests)
- Address specific weaknesses from Step 1 (e.g., basic science integration)
- Consider postponing the exam if practice scores are not yet in a safe range
If you already have a low Step 2 CK as well, your application will rely even more heavily on:
- Clinical grades
- Sub-internship performance
- Research and letters
- Strong personal narrative
Programs must see measurable competence somewhere—be sure you maximize what you can still influence.
B. Use COMLEX and USMLE Wisely
As a DO graduate, you may have:
- COMLEX only
- COMLEX + USMLE
- Or low scores on both exams
In highly competitive fields like CT surgery and general surgery, having USMLE scores is generally advantageous, especially at historically MD-dominated institutions. But if your USMLE scores are distinctly lower than your COMLEX, you must be cautious.
If you haven’t taken USMLE yet and your COMLEX is low:
- Honestly assess: can you do substantially better on USMLE with targeted prep?
- Get input from a trusted faculty mentor or advisor
- If you can’t realistically improve, it might be better to rely on COMLEX plus strong clinical evidence rather than adding another weak exam
C. Explain (Briefly) Without Making Excuses
If there is a clear, compelling reason for your low Step performance (e.g., serious illness, family crisis, inadequate accommodations for a disability), you can address this in:
- Your personal statement (briefly, 2–3 sentences)
- Or a dean’s letter / MSPE narrative section
Principles:
- Take responsibility where appropriate
- Emphasize what you changed afterward (study methods, time management, resources, wellness)
- Highlight subsequent improvement in clinical rotations or other exams
Example phrasing:
“I underperformed on Step 1 during a period marked by a family health crisis and poor time management. Since then, I have significantly restructured my study approach and prioritized well-being, resulting in improved performance on subsequent clinical rotations and Step 2 CK.”
Step 3: Build a CT-Relevant “Value Stack” That Outweighs Low Scores
With weaker boards, you must present such a strong overall value proposition that programs are willing to overlook your metrics. Think in terms of a “value stack”—multiple strengths layered together:
- CT-related research and scholarly output
- Strong clinical performance, especially in surgery
- Exceptional letters of recommendation, ideally from CT or surgical leaders
- Demonstrated technical aptitude and commitment to heart surgery training
- Professionalism, reliability, and teamwork
A. Research: Your Most Powerful Lever in a Competitive Field
In cardiothoracic surgery, research matters. For a DO with below average board scores, research can be a primary way to prove:
- Commitment to the field
- Academic capability despite earlier low scores
- Ability to contribute to a department’s scholarly mission
Target types of research:
- Cardiothoracic or cardiovascular surgery projects
- Thoracic oncology, aortic disease, valve disease, heart failure, transplant, mechanical circulatory support
- Quality improvement or outcomes research in cardiac or thoracic surgery
- Even general surgery research can help if CT-specific opportunities are limited
Option 1: Research During Medical School / Gap Year
If you still have time before applying:
- Seek a dedicated research year at an institution with a strong CT surgery department
- Aim for abstracts, presentations, and manuscripts, not just “shadowing research”
- Work with a well-known CT surgeon if possible
For DO graduates, a formal research fellowship at a major academic center can be a game changer, especially if:
- Your PI is respected nationally
- You produce tangible output (first- or co-author papers, podium presentations)
- You build relationships that lead to strong letters of recommendation
Option 2: Research During General Surgery Residency
If you pursue the general surgery → CT fellowship path:
- Join research projects early in residency (PGY-1/PGY-2)
- Target CT attendings who are engaged in clinical or outcomes research
- Present at regional/national meetings (STS, AATS, ACS, etc.)
Even if your board scores are weak, a strong research portfolio can help you later when you apply to cardiothoracic fellowships.
B. Excel Clinically: Rotations, Sub-Internships, and Audition Rotations
Program directors care deeply about how you function on the wards and in the OR. For a DO with low scores, clinical performance must be a highlight.
Priorities:
- Honor grades in surgery clerkships and sub-internships
- Glowing narrative comments on evaluations
- Evidence that you are reliable, teachable, and technically promising
Look for opportunities to do:
- Sub-internships (sub-Is) in general surgery at programs with strong CT presence
- Away rotations in CT surgery (if aiming for I-6 or to build early CT exposure)
- Rotations at DO-friendly institutions known to support osteopathic graduates in surgery
During these rotations:
- Be the hardest-working student, not the loudest
- Learn OR etiquette: anticipation, instrument names, suture handling
- Stay late, follow up on patients, read about your cases
- Ask for mid-rotation feedback and adjust immediately
C. Letters of Recommendation: Your “Voice” in the Selection Room
Strong, detailed letters can significantly offset low scores, especially if they come from respected surgeons.
Aim to secure letters from:
- At least one cardiothoracic surgeon (if possible)
- One or two general surgeons who directly supervised you clinically
- A research mentor familiar with your academic capabilities
You want letters that say more than “hardworking and pleasant.” They should include:
- Specific cases where you showed initiative or growth
- Comments on your technical promise and learning curve
- Comparison with other students or residents (“top 10% I’ve worked with”)
Ask for letters only after you have given the writer enough time to truly observe you. And explicitly ask if they can write a “strong, supportive letter” for competitive surgical training.

Step 4: Smart Application Strategy for DOs with Below Average Board Scores
A strong profile can still fall short if you apply without a plan. You must align your goals with the competitive landscape.
A. Choosing the Right Programs (and the Right Path)
Be honest about competitiveness.
- If your Step 1 and Step 2 scores are substantially below national averages and you lack substantial research or CT connections, applying broadly to I-6 CT programs as your main plan may not be the best use of resources.
- Instead, focus primarily on general surgery programs, with I-6 as a selective long-shot.
Prioritize DO-friendly programs.
- Look for general surgery residencies where DO graduates have historically matched.
- Check program websites, resident rosters, and match lists to see DO representation.
- Use NRMP/ERAS data and talk to upperclassmen or recent alumni.
Identify programs with strong CT exposure.
- Integrated CT programs at the same institution
- High CT case volume and established CT faculty
- Opportunities for residents to rotate on CT services or pursue CT-related research
Cast a wide net.
- With low scores, being geographically flexible increases your chances significantly.
- Apply to a broad range of programs including community programs with academic affiliations.
B. Tailoring Your Application Materials
Every part of your application must support the narrative:
“Despite early challenges on board exams, I have demonstrated consistent improvement, deep commitment to cardiothoracic surgery, and strong clinical performance that make me an excellent candidate for surgical training.”
Personal Statement:
- Clearly state your interest in surgery and future goals in heart surgery training
- Briefly acknowledge any score-related context if relevant, but do not dwell on it
- Emphasize growth, resilience, and what you’ve done since (research, rotations, leadership)
CV/Experiences Section:
- Feature CT or surgical experiences prominently
- Highlight leadership roles, teaching, and QI projects that demonstrate work ethic and maturity
- Quantify impact where possible (e.g., “co-authored 3 manuscripts,” “presented at 2 national meetings”)
C. Interview Strategy: Turning a Weakness into a Strength
If you’re invited to interviews, you’ve already cleared the initial screen. Now you must reinforce that the low scores are not who you are now.
When asked directly about low scores:
- Be concise, honest, and accountable
- Avoid blaming others or making excuses
- Emphasize what you learned and how you’ve improved
Example response framework:
- Acknowledge: “I did underperform on Step 1.”
- Context (brief): “At the time, I struggled with test strategy and time management.”
- Growth: “Afterward, I restructured my study methods, sought mentorship, and focused on foundational understanding.”
- Evidence: “You can see that reflected in my improved clinical evaluations, my stronger Step 2 CK performance, and my success in surgical rotations.”
Also, use interviews to highlight:
- Your long-term commitment to CT surgery
- Your willingness to work hard and learn
- Your compatibility with the program’s culture and values
Step 5: Backup Planning Without Giving Up Your CT Ambition
Not everyone will match on the first attempt—especially in competitive fields with low scores. Planning for contingencies doesn’t mean you don’t believe in yourself; it means you are strategic.
A. Strengthening Before Reapplying (If Needed)
If you don’t match:
- Consider a dedicated research fellowship in cardiothoracic or general surgery at a reputable institution.
- Continue to build your publication record and network with CT surgeons.
- Obtain updated, powerful letters of recommendation reflecting your new work.
- In some cases, a preliminary surgical year can also provide more clinical experience and letters—but be cautious, as prelim spots do not guarantee re-entry.
B. Alternative but Related Paths
Some DO graduates with persistent score-related barriers still pursue careers strongly related to cardiothoracic care, such as:
- Cardiology (with eventual structural or interventional focus)
- Critical care / cardiac anesthesia (if open to additional training pathways)
- Pulmonary/critical care with emphasis on thoracic ICU medicine
These paths can still let you work closely with cardiothoracic teams and high-acuity cardiac patients, even if you ultimately cannot secure heart surgery training itself.
C. Emotional and Professional Resilience
Repeated exposure to your score deficit can be draining. To stay grounded:
- Maintain regular contact with mentors who believe in your potential.
- Keep perspective: low scores limit certain doors but do not define your entire career.
- Invest in skills you can always use—communication, teamwork, analytical thinking, and teaching.
In competitive surgical disciplines, grit is often as important as talent. Your response to adversity—like low scores—is part of how programs will perceive your readiness for the rigors of a surgical career.
FAQs: Low Step Score Strategies for DOs Pursuing Cardiothoracic Surgery
1. Is it realistic for a DO graduate with low Step scores to match into cardiothoracic surgery?
It is realistic, but not guaranteed, and generally harder. Direct entry into an integrated CT program is extremely challenging with low scores unless you have exceptional compensating strengths (major research, strong CT connections, outstanding letters). The more realistic path for most DOs with weaker scores is to:
- Match into a solid general surgery residency, preferably DO-friendly and CT-exposed
- Excel clinically and academically
- Apply to cardiothoracic fellowship with a strong portfolio
2. Should I still apply to integrated cardiothoracic surgery (I-6) programs?
You can consider I-6 applications if:
- You have strong CT research and mentor support
- You can afford the time and financial cost of a broad, competitive application
- You understand that it is likely a reach rather than your primary plan
For most DO applicants with below average board scores, I-6 should be a secondary or aspirational target, with general surgery as the primary and realistic focus.
3. How important is research for matching into CT surgery if my scores are low?
For you, it is very important. Research demonstrates academic capability and commitment to the field, both of which can partially offset low Step scores. A robust record of CT-related research—especially with publications and presentations—signals to programs that you are serious about contributing to the specialty. A structured research year or fellowship with a notable CT surgeon can be particularly valuable.
4. Should I mention my low scores directly in my personal statement?
You may briefly address them only if there is meaningful context and growth to describe (e.g., health issues, personal circumstances, initial adjustment to medical school). The focus should be on:
- What you learned
- What changed in your approach
- How subsequent performance (Step 2, clinical rotations, research productivity) shows improvement
Avoid centering your entire personal statement on the scores. The main emphasis should be your journey toward surgery, your commitment to cardiothoracic care, and the strengths you bring to a program.
By approaching your application with strategic clarity—acknowledging your low scores, yet systematically building compensating strengths—you can still carve a path toward cardiothoracic surgery residency or a later CT fellowship. As a DO graduate, your osteopathic background, resilience, and commitment to patients can be assets, not liabilities, when combined with focused planning and sustained effort.






















