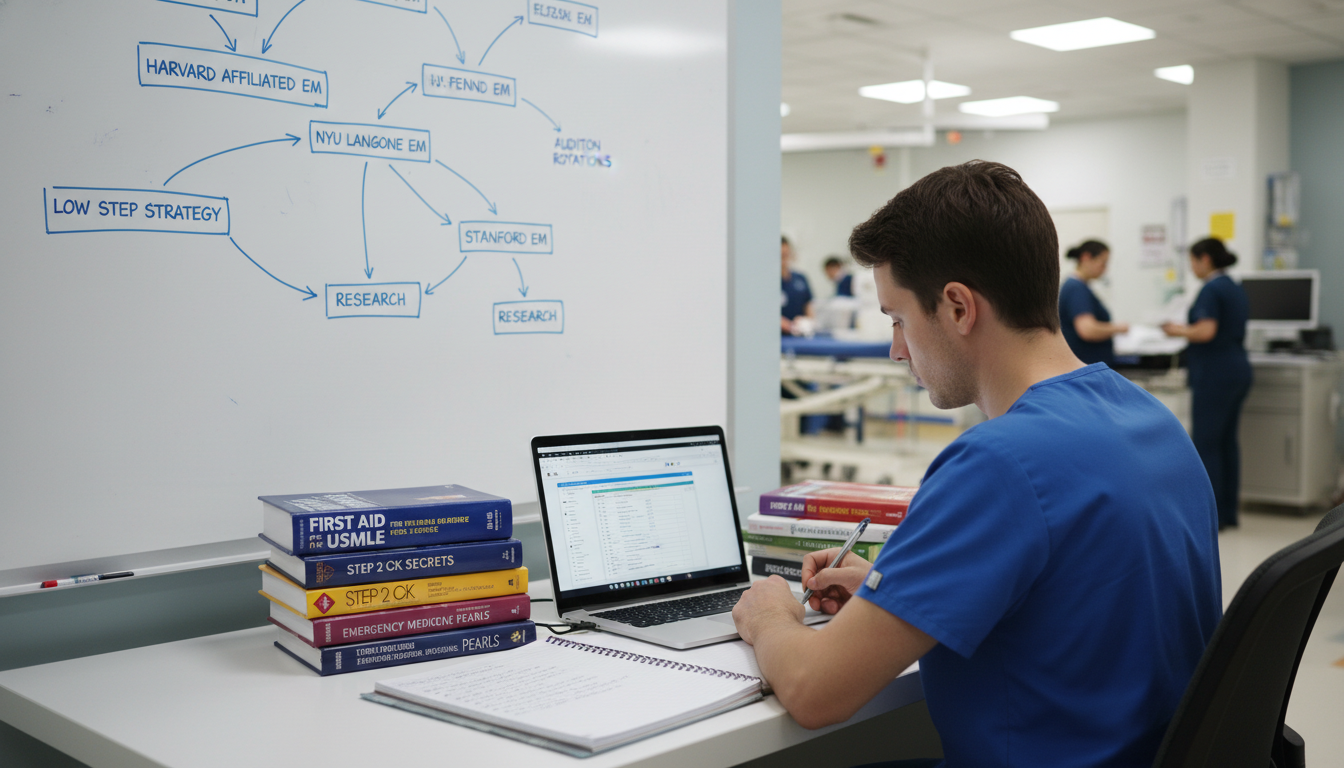
Understanding the Challenge: Low Step Scores and the EM Match
For an MD graduate targeting emergency medicine residency, a low Step 1 or Step 2 CK score can feel like a door closing. It isn’t. Emergency Medicine (EM) remains accessible to many applicants with below average board scores—if you are strategic, realistic, and disciplined.
In the current environment, Step 1 is pass/fail, but many EM programs still examine historical numeric Step 1 scores (for older graduates) and place heavy emphasis on Step 2 CK. If you are an MD graduate from an allopathic medical school with a low Step 1 score or a modest Step 2 CK, there are still viable paths into an emergency medicine residency.
This guide focuses on low Step score strategies specifically for EM, tailored to an MD graduate approaching or in the allopathic medical school match process. You’ll find practical, concrete steps to improve your EM match odds despite low scores.
Reality Check: How Much Do Scores Matter in EM?
Emergency medicine has traditionally emphasized standardized test performance, but it is also a specialty that strongly values clinical performance, work ethic, and fit. That combination gives you room to compensate for weaker numbers.
Where Scores Matter Most
Initial Application Screen
- Many programs use score thresholds (especially Step 2 CK) to sift applicants quickly.
- “Red flag” ranges vary, but many EM programs consider:
- Below ~215–220: potentially concerning, depending on the overall application.
- Below ~200: often treated as a significant red flag, but not always disqualifying if other factors are strong and explained.
Perceived Risk of Failing Boards
- EM PDs worry about in‑training exams and ABEM written boards.
- A low Step 1 score combined with low or barely passing Step 2 CK is interpreted as a possible pattern.
- A clear upward trend—even if still a bit “below average”—helps reduce that concern.
Comparison With Peer Applicants
- US MDs generally fare better than DO or international grads with similar scores because of perceived training standardization and clinical experiences.
- As a US MD with low scores, you begin with some advantages, but you still must prove you can handle the cognitive load.
Where You Can Outweigh Your Scores
Emergency medicine is uniquely inclined to reward:
- Strong Standardized Letters of Evaluation (SLOEs) from EM rotations.
- Demonstrated clinical performance under pressure.
- Evidence of teamwork, resilience, and communication.
- A history of reliable, hands-on work in clinical settings.
Your strategy should be to minimize the impact of your low Step 1 score and/or weak Step 2 CK by building a profile where PDs think, “Yes, the scores are a concern, but everything else about this candidate screams ‘safe, teachable, and hard-working resident.’”

Core Strategy 1: Optimize Your Step 2 CK and Knowledge Profile
For an MD graduate with a low Step 1 score, Step 2 CK becomes your primary tool to show growth. For those who already have a low Step 2 CK, your goal shifts to demonstrating knowledge progression and remediation.
Scenario A: Step 2 CK Still Pending
If you haven’t taken Step 2 CK yet, this is your highest-yield move.
Delay Match If Necessary
- If your Step 1 is low, rushing a mediocre or rushed Step 2 CK is risky.
- Taking an extra 3–6 months after graduation to prepare properly, do research or work clinically (e.g., scribe), and then crush Step 2 can radically improve your profile.
- An MD graduate with a low Step 1 but solid (or at least improved) Step 2 CK can be very competitive in an allopathic medical school match.
Study Like a Board-At-Risk Candidate
- Assume you are at higher risk and use intensive strategies:
- Core resources: UWorld (complete at least one full pass), NBME practice tests (all available forms).
- Structured schedule: 6–8 weeks of dedicated time, full-time study if possible.
- Track progress with practice tests; do not test until your practice NBME scores are consistently at or above your target (often at least low- to mid-220s for EM, higher is better).
- Assume you are at higher risk and use intensive strategies:
Engage Institutional Support
- Use your med school’s learning specialists, tutoring programs, or Step 2 CK remediation pathways.
- Ask for a formal study plan letter if available—this can later support your personal statement or advisor letter by showing that you took proactive steps.
Scenario B: Step 2 CK is Already Low
When your Step 2 CK is already low or below average:
- You can’t erase the number.
- But you can provide evidence of growth and improved knowledge:
Take COMLEX or Additional Assessments?
- As an MD, you won’t take COMLEX, but you can:
- Use NBME Comprehensive Clinical Science exams or institutional exams to show internal progress.
- Ask an advisor or clerkship director to mention in their letter that your knowledge base has noticeably improved through dedicated effort.
- As an MD, you won’t take COMLEX, but you can:
Highlight In‑Training Exam Surrogates (If a Reapplicant)
- If you did a preliminary year (e.g., Transitional Year or Preliminary IM) and performed well on in-training exams, ask your PD to mention that in their letter.
- This directly reassures EM PDs about board risk.
Formal Statement of Remediation
- In your personal statement or supplemental ERAS essay, briefly but clearly describe:
- What contributed to your low scores (without making excuses).
- The specific, structured changes you made (e.g., meeting with learning specialists, systematic UWorld use, dedicated reading).
- Evidence of improvement (e.g., shelf exams, honors in clerkships, strong SLOEs).
- Keep this to one focused paragraph; do not let your application become a wall of apologies.
- In your personal statement or supplemental ERAS essay, briefly but clearly describe:
Core Strategy 2: Maximize EM Rotations and SLOEs
In emergency medicine, SLOEs are often as important—or more important—than your board scores. With low Step scores, strong SLOEs become absolutely critical.
Target: 2–3 High-Quality SLOEs
Most EM applicants aim for:
- 2 SLOEs from academic EM programs where you completed visiting or home EM rotations.
- A possible 3rd SLOE if feasible, from another EM rotation or high-acuity setting.
With low Step 1 or Step 2 CK scores, plan for:
- At least 2 strong SLOEs where you are ranked in the top third of students, or at worst, solidly in the middle with enthusiastic narrative comments.
How to Perform Exceptionally on EM Rotations
Treat every EM shift as a months-long job interview.
Arrive Early, Leave Late
- Demonstrate reliability and stamina.
- Offer to stay for one more patient or help with sign-out tasks.
Be Proactive—but Safe
- See patients quickly, present concisely:
- 2–3 sentence HPI summary
- Focused differential and plan
- Always confirm with the resident/attending before major decisions.
- Show that you appreciate safety, triage, and disposition, core EM skills.
- See patients quickly, present concisely:
Master EM-Specific Knowledge
- Focus on bread-and-butter EM:
- Chest pain, abdominal pain, shortness of breath, sepsis, trauma basics, overdose, stroke, pediatric fevers.
- Before or after each shift, read focused EM texts (e.g., EMRA Basics, Rosen’s Chapters, Tintinalli summaries).
- Focus on bread-and-butter EM:
Ask for Feedback Mid-Rotation
- Around the halfway point, ask: “What’s one thing I could do better to be a strong candidate for EM?”
- Then implement that feedback. This gets noticed and can improve your final evaluation and SLOE language.
Clarify Your Score Context if Appropriate
- If you build rapport with an attending or clerkship director, you may briefly explain your low Step scores and how you’ve addressed them.
- Don’t lead with this, but if they ask about your performance or background, be honest and emphasize your trajectory and current performance.
- Some faculty will specifically advocate for you in the SLOE narrative if they understand your story.
Choosing Where to Rotate
If your scores are low, choose EM rotations strategically:
- Mid-tier or smaller academic programs may be more open to applicants with below average board scores if your clinical performance is strong.
- Community EM programs with academic affiliations can also be excellent for SLOEs.
- Avoid relying solely on hyper-competitive academic powerhouses for SLOEs unless you have internal connections—those environments often have more applicants than they can strongly support.

Core Strategy 3: Build a Program List That Matches Your Profile
With low Step scores, where you apply and how broadly you apply matter almost as much as how strong your application is.
Calibrating Your Competitiveness
For MD graduates in EM, consider these general guidelines (not absolute cutoffs):
- Relatively safer range: Step 2 CK ~220–230 with strong SLOEs and solid clinical record.
- Borderline/concern range: Step 2 CK ~205–219; requires strong supporting evidence—SLOEs, narrative explanations, and robust application strategy.
- High-risk range: Step 2 CK <205, or Step failures; still possible, but you must be extremely strategic, open to alternative paths, and realistic.
Program Tiers & Types to Target
Mid- and Lower-Tier Academic EM Programs
- Often have a mix of trauma, academic exposure, and community-style practice.
- May be more flexible about low scores if SLOEs and interviews are strong.
Community EM Programs
- Sometimes more willing to consider applicants with matching with low scores, especially if you show commitment to their region and can articulate why community EM fits you.
- Many produce excellent, well-trained emergency physicians.
Geographic Strategy
- Apply heavily (20–30+ programs) in regions where you have:
- Ties (family, prior schooling, previous work).
- Existing relationships (mentors, prior research).
- Programs are more likely to bend on scores for candidates who are likely to stay and thrive in their environment.
- Apply heavily (20–30+ programs) in regions where you have:
Avoid Over-Concentrating on Elite Programs
- While it’s fine to include a few “reach” academic EM programs, do not anchor your application there if you have low Step scores.
- Your priority is to maximize interview invitations, not prestige.
How Many Programs Should You Apply To?
For an MD graduate with low Step scores, a reasonable approximate range might be:
- If Step 2 CK 220+ but Step 1 low: 25–35 programs.
- If Step 2 CK 205–219: 35–50 programs, weighted toward community and mid-tier academic sites.
- If Step 2 CK <205 or any failure: often 45–60+ programs, plus serious consideration of backup strategies (see below).
Individual circumstances vary; work with your school’s EM advisor or EMRA/CORD advising resources to fine-tune.
Core Strategy 4: Strengthen the Rest of Your Application to Offset Low Scores
Beyond test scores and SLOEs, EM PDs look at the whole picture. Every part of your application can either reinforce “this applicant is risky” or “this applicant is resilient and reliable.”
1. Personal Statement: Address, Don’t Obsess
Your personal statement should:
- Focus on why emergency medicine fits your skills, personality, and experiences.
- Provide a brief, targeted explanation of low scores, if they’re a major outlier:
- One paragraph: cause → response → result.
- Emphasize growth, insight, and durability under stress.
- Avoid over-defensiveness or long, emotional narratives about testing problems.
Example framing:
“Early in medical school, I struggled with time management and test-taking strategies, which is reflected in my lower Step 1 score. Recognizing this, I sought academic support, developed a structured study plan, and changed how I approached clinical learning. Since then, my clerkship evaluations, EM rotation performance, and Step 2 CK improvement have reflected this growth. More importantly, these changes have made me a more diligent, reflective, and reliable teammate in the ED.”
2. Experiences and CV
Highlight experiences that show:
- Comfort in acute care settings: ED scribing, EMT work, ICU volunteering, paramedic background.
- Teamwork and leadership: leadership in interest groups, QI projects, simulation teaching.
- Resilience under stress: jobs or roles that required sustained effort and reliability (e.g., working full-time while in school, military service, significant family responsibilities).
These can reassure PDs that:
- You’ve functioned well in demanding environments.
- You can handle the pressures of an emergency medicine residency despite lower exam scores.
3. Letters of Recommendation Beyond SLOEs
While SLOEs are critical, 1–2 additional letters can help:
- From internal medicine, surgery, ICU, or EM-related electives.
- Ideally from attendings who specifically comment on:
- Your clinical reasoning and improvement over time.
- Your work ethic, professionalism, and ability to learn from feedback.
Ask letter writers:
- To address any concerns about exams by highlighting your current competency and likelihood to succeed in residency.
4. Research and Scholarly Work
You don’t need extensive research to match EM, but it can help offset concerns:
- EM-related QI projects, case reports, or retrospective studies show engagement and academic curiosity.
- If your school has limited EM research, consider:
- Participating in multi-center EM research networks.
- Working with hospitalists, ICU, or trauma surgery on ED-related topics.
The goal is not sheer volume, but evidence of commitment and follow-through.
Core Strategy 5: Interview Season and Backup Planning
Even with low scores, once you get an interview, many PDs will reassess you primarily on your in-person (or virtual) performance. At the same time, realistic backup planning is essential.
A. Excelling in EM Interviews
Own Your Narrative
- Be ready for variations of:
- “Can you tell us about your board performance?”
- Use a consistent, confident, and concise explanation:
- Brief cause → clear remediation → demonstrated improvement → why you’re now prepared.
- Be ready for variations of:
Emphasize Fit and Work Ethic
- EM is team-based; highlight:
- Times you supported overwhelmed teammates.
- How you handle simultaneous demands.
- Be specific about:
- Why community vs academic EM suits you (based on the program).
- How your experiences align with the population they serve.
- EM is team-based; highlight:
Show Knowledge Growth Without Being Defensive
- If asked about how you’re maintaining or improving your knowledge:
- Mention ongoing reading, EM podcasts, EM-specific resources, or simulation.
- Frame yourself as constantly learning and coachable.
- If asked about how you’re maintaining or improving your knowledge:
Prepare Questions That Reflect Insight
- Ask about:
- Support for boards/in-training exam prep.
- Feedback mechanisms and resident wellness.
- This can subtly signal that you are aware of your previous struggles and are proactively seeking supportive environments.
- Ask about:
B. Ranking Strategy
When ranking:
- Place programs where you have strong SLOEs and felt comfortable higher, assuming you would genuinely be happy there.
- Do not over-prioritize prestige if it risks going unmatched.
- Rank all programs you interviewed at where you would be willing to train. With low scores, you can’t afford to play “rank list games.”
C. Backup and Parallel Plans
With particularly low or failing boards, consider backup strategies in the same application cycle:
Applying to a Backup Specialty
- Fields sometimes considered more flexible with scores (though this changes over time) include:
- Family Medicine
- Internal Medicine (community programs)
- Psychiatry (varies by region)
- If EM is your clear long-term goal, you can:
- Do a preliminary or transitional year while building your profile, then reapply to EM.
- Use that year to excel clinically and perform well on in-training exams, getting powerful letters.
- Fields sometimes considered more flexible with scores (though this changes over time) include:
Dedicated Post-Graduate Year
- Options may include:
- A formal EM research fellowship/position with substantial clinical exposure.
- Working as an ED scribe or PA/NP assistant while enhancing your EM visibility and studying.
- Options may include:
Reapplication Strategy
- If you go unmatched:
- Seek immediate feedback from EM advisors or PDs (through advisors, EMRA, or CORD resources).
- Strengthen your SLOEs, knowledge base, and experiences.
- Expand your application breadth geographically and by program type in the next cycle.
- If you go unmatched:
Putting It All Together: A Sample Roadmap
To make this more concrete, here’s a sample strategy for an MD graduate with a low Step 1 and modest Step 2 CK aiming for an emergency medicine residency:
Profile Example
- MD graduate from a US allopathic school.
- Step 1: 204 (first attempt).
- Step 2 CK: 218.
- Strong third-year clerkship evaluations, especially in IM and surgery.
- One good EM rotation so far with a “middle third” SLOE.
Strategic Actions
- Schedule one more EM away rotation at a mid-tier academic or community-affiliated program known to be supportive of diverse candidates.
- On that rotation, aim for:
- High engagement, proactive learning.
- A SLOE ideally in the top third with very positive narrative comments.
- Meet with a faculty EM advisor to:
- Craft a concise personal statement that explains your exam trajectory.
- Generate a realistic program list (e.g., 35–45 programs, heavily community/mid-tier).
- Strengthen the rest of the application:
- Ask for an additional letter from IM or ICU highlighting your knowledge growth and reliability.
- Add any ED-related experience (volunteering, quality improvement project) to your CV.
- During interviews:
- Consistently own your story: early test struggles, structured remediation, and evidence of improvement.
- Highlight how your clinical performance and work ethic will make you a safe, dependable EM resident.
- Create a backup:
- Consider applying simultaneously to a limited number of community Internal Medicine programs where you have ties, just in case.
- If unmatched, use SOAP strategically or plan for a year of clinical/research work in EM, then reapply with stronger support and updated letters.
This kind of focused, honest, and proactive approach will not eliminate the impact of low Step scores, but it maximizes your chances of a successful EM match.
FAQs: Low Step Scores and Emergency Medicine Residency
1. Can I still match EM with a low Step 1 score if my Step 2 CK is average or slightly above average?
Yes. For an MD graduate, a low Step 1 but more solid Step 2 CK is often acceptable, especially if you have 2 strong SLOEs, strong clinical evaluations, and a well-calibrated program list. Programs are increasingly looking at Step 2 CK as the primary numeric benchmark, and many PDs care more about your trajectory than a single early score.
2. I have both low Step 1 and low Step 2 CK scores. Do I still have a shot at an emergency medicine residency?
You do, but you are in a higher-risk category. Your path will depend on:
- How low the scores are (e.g., 205 vs 190).
- Whether there were any failures.
- The strength of your SLOEs, clinical performance, and letters.
You’ll need:
- Exceptionally strong SLOEs.
- A broad application strategy, focusing on community and mid-tier programs.
- Possibly a backup specialty or plan (e.g., a preliminary year, research year with clinical exposure).
3. Should I explain my low scores in my personal statement or during interviews?
Briefly, yes—especially if they are a clear outlier. The key:
- Be concise and factual, not defensive.
- Emphasize what you did to address the issue and how your later performance shows improvement.
- In interviews, be ready with a consistent explanation and pivot quickly to what you’ve learned and how you now perform clinically.
4. How many EM programs should I apply to if I’m matching with low scores?
There is no one-size-fits-all number, but general guidance for MD graduates might be:
- Step 2 CK around 220+ with strong SLOEs: ~25–35 EM programs.
- Step 2 CK 205–219: ~35–50 EM programs, heavily weighted toward community and mid-tier.
- Step 2 CK <205 or failures: 45–60+ EM programs, plus backup options.
Always adjust based on your advisor’s input, geographic flexibility, and the rest of your application strength.
Low Step scores complicate the road to an emergency medicine residency, but they do not close it. By maximizing your clinical performance, securing powerful SLOEs, crafting a realistic program list, and clearly demonstrating growth and resilience, you can still carve a successful path into EM as an MD graduate—despite the numbers.






















