
Understanding the Challenge: Low Step Scores as an IMG in Appalachia
For many international medical graduates, a low Step 1 score or below average board scores can feel like an insurmountable barrier. When you add the complexity of being an IMG and your interest in Appalachian residency programs—especially in West Virginia and Kentucky—the path can seem even narrower.
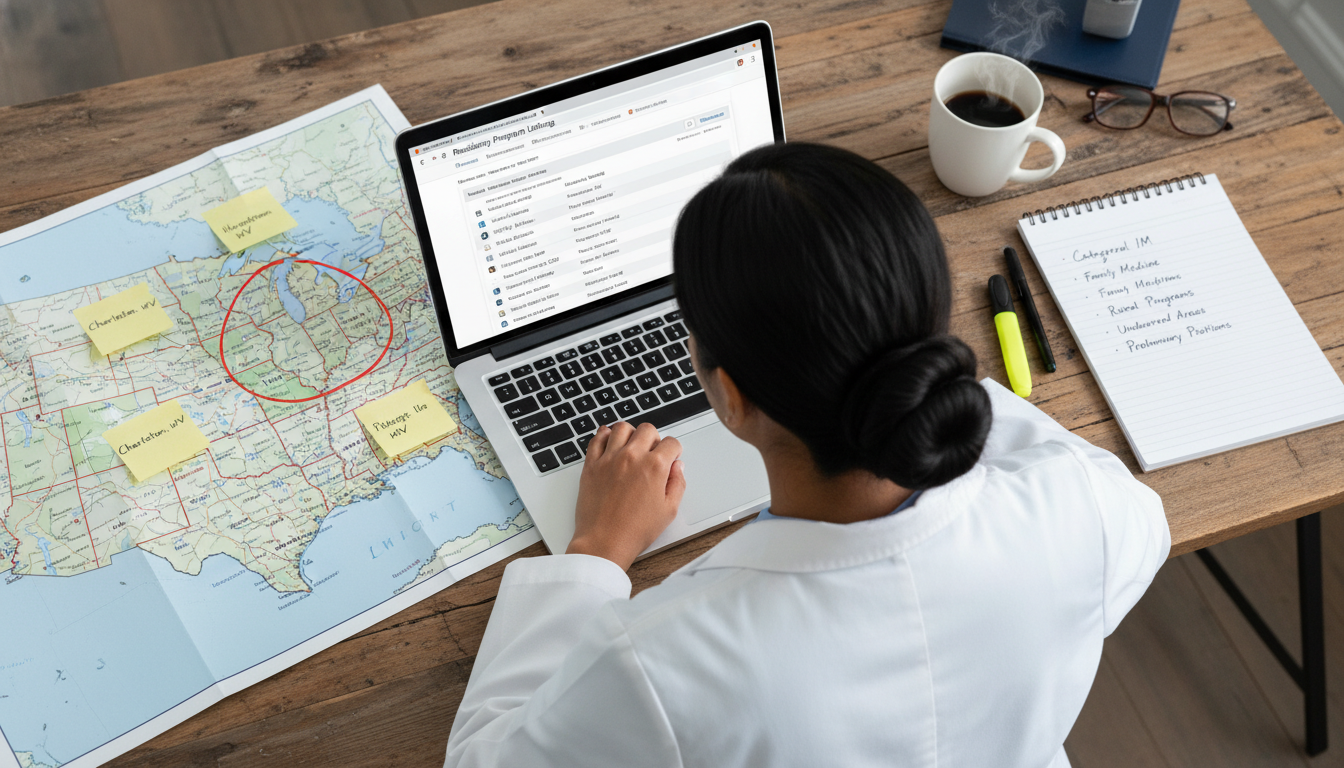
Yet, each year, IMGs with imperfect scores successfully match into solid programs across Appalachia. The key is not to “hide” your score, but to strategically build a profile that makes programs look past it.
This IMG residency guide is tailored specifically for:
- IMGs with a low Step 1 score or below average Step 2 CK
- Applicants targeting Appalachian residency programs (internal medicine, family medicine, psychiatry, pediatrics, prelim/transitional year, etc.)
- Those particularly interested in West Virginia and Kentucky residency opportunities
We’ll cover concrete, realistic strategies that focus on:
- Where to apply (and where not to)
- How to compensate for low scores
- How to communicate your story
- How to use the unique context of Appalachia to your advantage
1. Reframing “Low Scores”: What It Means in the Appalachian Context
Before designing a strategy, you need to understand how programs in Appalachia think about scores—and how you can still be competitive.
1.1 What Counts as a “Low” Score?
While numeric Step 1 scores are now pass/fail, many IMGs still have legacy numeric Step 1 scores on their transcripts. Even for those with pass/fail Step 1, a comparatively low Step 2 CK can trigger similar concerns.
Rough benchmarks (these are approximate, not rules):
- Step 2 CK
- 265+: Exceptional
- 250–264: Very strong
- 240–249: Competitive
- 230–239: Average to slightly below average at many academic programs
- <230: Often considered low at university programs, but still workable for many community and some university-affiliated programs—especially in underserved regions like parts of Appalachia
If you have:
- Step 1 (legacy numeric): <220 or
- Step 2 CK: <230
you’re realistically in the “matching with low scores” category and must approach the process strategically.
1.2 Why Some Appalachian Programs Are More Flexible
The Appalachian region—covering large parts of West Virginia, Kentucky, Eastern Tennessee, Western Virginia, and surrounding areas—has:
- High physician shortages, especially in primary care, psychiatry, and rural medicine
- Populations with complex social determinants of health, substance use, and chronic disease
- Difficulty attracting graduates from “top” coastal or large urban programs
Because of this:
- Many programs are mission-driven: they prioritize candidates committed to working with underserved or rural populations.
- Some programs are more flexible on scores if you demonstrate:
- Strong clinical performance
- Genuine regional commitment
- Maturity and professionalism
- Strong letters and work ethic
Your lower scores may still be a hurdle, but they are not automatically disqualifying, especially in West Virginia and Kentucky community-based or university-affiliated community programs.
1.3 The IMG Advantage in Appalachia
As an international medical graduate, you may bring:
- Multilingual skills
- Experience with resource-limited settings
- Resilience, adaptability, and cultural humility
If you’re able to show how these strengths fit the needs of Appalachian communities—rural poverty, health literacy challenges, opioid crisis—you become more than “an IMG with low scores.” You become exactly the type of physician many programs are trying to recruit.
2. Strategic Program Targeting: Where and How to Apply
Your application list is your single biggest lever as an IMG with below average board scores. You cannot afford a random or prestige-driven approach.
2.1 Types of Programs More Open to Lower Scores
In Appalachia, prioritize:
Community-Based Internal Medicine / Family Medicine / Psychiatry Programs
- Often affiliated with a regional university
- Serve large rural catchment areas
- More holistic evaluation of applicants, especially with strong clinical histories
University-Affiliated Community Programs
- Example structures: “X Medical Center / University of Y Partnership”
- Moderate research, but heavy service orientation
- Frequently have active interest in IMGs and underserved care
Newer or Recently Expanded Programs
- Newer family medicine, internal medicine, or psychiatry residencies in West Virginia and Kentucky may be growing quickly
- They often have more flexibility and are eager to fill positions with motivated candidates
Primary Care or Rural Track Programs
- Programs with rural or underserved tracks often value mission-fit strongly
- They may explicitly highlight interest in applicants with diverse backgrounds and commitment to underserved populations
2.2 Reducing Applications with Low Yield
Be cautious about:
- Highly research-oriented, top-tier academic centers that heavily advertise:
- “Strong emphasis on research”
- Multiple fellowships, NIH funding, high subspecialty match rates
- Programs with explicit score cutoffs higher than your scores on their website, such as:
- “We require a Step 2 CK ≥ 240 for interview consideration”
- Programs with:
- “No IMG” or “very limited IMG” history
- Very low IMG percentage over the last 3–5 years
You can still apply to a small number of “stretch” programs, but most of your application budget should go to realistic options.
2.3 How to Research Programs Effectively
For a strong IMG residency guide strategy, use this structured approach:
Freida, program websites, and NRMP data
- Filter for West Virginia, Kentucky, and neighboring Appalachian states.
- Check:
- Percentage of IMGs in current residents
- Apparent cutoff scores (if listed)
- Mission statements: terms like “rural,” “underserved,” “community-focused,” “Appalachian,” “primary care,” “addiction medicine”
Current Resident Rosters
- Look for names suggesting international backgrounds
- Note countries/medical schools represented
- This reveals whether the program routinely trusts IMGs
Social Media (program Instagram, Twitter/X, LinkedIn)
- Observe how they highlight resident life, rural rotations, community work
- Programs emphasizing service over prestige may be more holistic
Networking
- Reach out politely to current IMG residents via LinkedIn or email
- Ask:
- “Do you know if the program considers applicants with lower Step scores?”
- “What do they value most in applications from IMGs?”
2.4 Suggested Distribution for Low-Score IMGs Targeting Appalachia
This is a general template, adjust to your situation:
- Total programs: 80–120 (common for IMGs with low scores)
- 60–70%: Community or community-affiliated programs in Appalachia and similar underserved regions
- 20–30%: Other regions with high IMG friendly reputations (Midwest, some Southern states)
- 5–10%: “Stretch” academic or hybrid programs where you have strong ties or unique fit
For West Virginia and Kentucky residency specifically:
- Identify:
- 5–10 programs in each state where IMGs are clearly present
- 5–10 additional programs in neighboring Appalachian states (e.g., Eastern Tennessee, Western Pennsylvania, parts of Ohio and Virginia) that share similar rural/underserved missions
3. Compensating for Low Scores: Building a Stronger Application
Your strategy should be: scores are one data point—overwhelm them with stronger data everywhere else.
3.1 Maximize Step 2 CK and OET/English Proof
If your Step 1 score is low, your Step 2 CK becomes critical.
If you haven’t taken Step 2 CK yet:
- Treat it as a redemption exam:
- Give yourself adequate study time (3–6 months if needed)
- Use high-yield question banks aggressively (UWorld, AMBOSS)
- Consider a short dedicated period away from work if possible
- Target:
- Ideally ≥235 if your Step 1 was weak
- But even an improvement of 20+ points over Step 1 is significant evidence of growth
- Treat it as a redemption exam:
If Step 2 CK is already low:
- You cannot change the number, but you can:
- Highlight improvement between Step 1 and Step 2 (if any)
- Emphasize strengths in other parts of the application
- Show concrete clinical excellence (clerkships, USCE, letters)
- You cannot change the number, but you can:
Ensure strong English language evidence:
- If applicable, a high OET or TOEFL (where still relevant)
- Flawless written communication in all application documents
3.2 U.S. Clinical Experience (USCE) with Appalachian Relevance
For matching with low scores as an IMG, USCE is essential. To align with your regional interest:
Seek:
- Rotations or observerships in:
- Community hospitals
- Federally Qualified Health Centers (FQHCs)
- Rural clinics in or near Appalachia
- Rotations or observerships in:
Focus on:
- Internal medicine, family medicine, psychiatry, or pediatrics (based on your target specialty)
- Sites that serve underserved, rural, or low-income populations
Ask supervisors to comment on:
- Your reliability and work ethic
- Your rapport with patients from low-resource backgrounds
- Your adaptability to U.S. healthcare and EHR systems
These experiences help programs believe you will thrive in their Appalachian context, not just survive.
3.3 High-Impact Letters of Recommendation
Strong U.S.-based letters can significantly counterbalance lower scores.
Aim for:
- 3–4 letters from U.S. physicians, ideally:
- At least 2 in your target specialty
- 1 from a setting similar to Appalachian practice (rural, community, underserved)
- 3–4 letters from U.S. physicians, ideally:
Ask letter writers to be specific:
- “Despite below average board scores, Dr. X consistently demonstrated clinical reasoning and bedside decision-making superior to many U.S. graduates I’ve worked with.”
- “Dr. X quickly adapted to our resource-limited environment and built excellent rapport with patients from rural West Virginia.”
Provide writers with:
- Your CV
- A short personal statement or “summary of my story”
- A reminder of interesting cases or experiences you shared
3.4 Research, QI, and Community Service with a Rural/Underserved Angle
You don’t need first-author NEJM papers. You do need evidence that you care deeply and act on that care.
Examples that fit an Appalachian residency narrative:
Community projects:
- Health education workshops about diabetes, hypertension, or substance use in rural or low-resource settings
- Work with NGOs or clinics serving underserved populations in your home country
Quality improvement:
- Small QI projects in clinics (improving blood pressure follow-up, screening rates, vaccination tracking)
- Presenting posters at regional or local meetings
Research:
- Projects related to addiction, chronic disease, mental health, telemedicine, or rural health access
These experiences help programs see you as a future community-focused physician, not just a test taker.
4. Crafting Your Narrative: Personal Statement, CV, and Interviews
Your story must tie everything together: low scores, IMG background, and Appalachian interest.

4.1 Personal Statement: Turning a Weakness into Maturity
For an international medical graduate with low scores, your personal statement can:
- Acknowledge but not obsess over your low scores.
- Emphasize:
- Growth
- Reflection
- Your mission in Appalachia
Structure example:
Opening story: A brief clinical moment that shaped your interest in rural or underserved care—could be from your home country or U.S. experience.
Your journey as an IMG:
- Specific challenges you’ve faced and overcome
- How these experiences shaped your resilience, adaptability, and humility
Address low scores briefly and strategically:
- 2–3 sentences only
- Example:
“My Step 1 score does not fully reflect my capabilities as a clinician. During that period, I was simultaneously [brief reason if appropriate—family illness, system change, adjustment to a new country]. Since then, I have improved my study strategies and time management, as reflected in my stronger clinical evaluations and [Step 2 CK improvement / USCE performance]. More importantly, these challenges deepened my empathy for patients who face barriers and setbacks in their own lives.”
Why Appalachia specifically:
- Mention:
- Rural health challenges
- Opioid epidemic
- Economic hardship
- Access issues in West Virginia and Kentucky
- Show you’ve learned about:
- Local health disparities
- Rural hospital closures
- Shortages in primary care and mental health
- Mention:
Why this specialty in this region:
- Tie your goals to:
- Working long term in a rural or medically underserved community
- Possibly pursuing addiction medicine, rural tracks, or community leadership roles
- Tie your goals to:
Conclusion:
- Emphasize your commitment, not perfection
- Reassure programs you are ready to work hard and stay long-term in underserved regions
4.2 CV: Highlighting What Matters Most
Organize your CV to draw attention away from test scores and toward:
USCE first
- Clear, detailed descriptions:
- “Hands-on sub-internship in Internal Medicine at [Hospital], caring for largely rural patient population from [state], with substantial comorbid mental health and substance use conditions.”
- Clear, detailed descriptions:
Leadership and service
- Positions in:
- Community health projects
- Rural clinics
- Advocacy for underserved groups
- Positions in:
Skills relevant to Appalachia
- Languages spoken
- Training in addiction medicine, motivational interviewing
- Experience with telehealth
4.3 Interview Strategy: Answering the Low Score Question
You will almost certainly hear:
“Can you tell us about your board scores?”
“We noticed your Step 1 score was lower; what happened and what have you learned from that?”
Your response should be:
- Honest
- Brief
- Forward-looking
A strong framework:
Own it:
- “You’re right, my Step 1 score is lower than I hoped.”
Context, not excuses:
- “At that time, I struggled with [brief factor: language transition, ineffective study methods, adjusting to a new academic system].”
Concrete learning:
- “I changed my approach by [joining study groups, using question banks more effectively, creating spaced repetition systems].”
Evidence of improvement:
- “This led to better performance on Step 2 CK, and more importantly, consistent strong feedback from my U.S. clinical rotations.”
Tie to patient care:
- “This experience also helped me better understand my patients’ struggles with learning and behavior change—especially in communities facing multiple barriers like many in Appalachia.”
Avoid:
- Over-long explanations
- Blaming others
- Appearing defensive or ashamed
Your tone should communicate: “I faced a setback, I learned, and I’m now much stronger because of it.”
5. Appalachia-Specific Strategies: Showing True Regional Commitment
Programs in Appalachia are very skeptical of candidates who appear to be using them as a “backup” or “stepping stone.” You must demonstrate that you specifically want to train and likely remain in the region.
5.1 Learn the Region’s Real Health Needs
Before applying and every time you interview, study:
Major health issues in West Virginia and Kentucky:
- High rates of opioid and other substance use disorders
- Obesity, diabetes, chronic lung disease (coal-related disease in some areas)
- Limited mental health access
- Transportation barriers and hospital closures in rural counties
Healthcare system features:
- Role of critical access hospitals
- Use of nurse practitioners and PAs in rural care
- Telemedicine expansion in mountainous areas
Being able to discuss these topics concretely shows serious interest in Appalachia.
5.2 Practical Ways to Build True Regional Ties
If possible:
- Do an elective or observership in Appalachia
- Even 4–8 weeks in West Virginia or Kentucky can significantly strengthen your application
- Attend regional conferences (even virtually)
- Topics on rural health, addiction medicine, or Appalachian health
- Network with physicians practicing there
- Reach out to speakers or authors who work in Appalachian health
- Politely express your interest in their work and region
If you cannot physically go to the area before applying:
- Show thematic alignment:
- In your personal statement, letters, and CV, emphasize:
- Your comfort in small-town settings
- Experience in rural or under-resourced environments in your home country
- Interest in long-term relationships with patients and families
- In your personal statement, letters, and CV, emphasize:
5.3 Answering: “Why Appalachia?” in Interviews
Your answer should not sound generic like: “I want to serve underserved populations.” It should sound specific and informed.
Stronger version:
“I am particularly interested in training in Appalachia because of the unique combination of rural geography, economic challenges, and high disease burden. In my rotations, I’ve seen how patients facing poverty and limited transportation struggle with chronic disease and access to care. When I learned more about health indicators in West Virginia and Kentucky, especially the opioid crisis and shortages in primary care and mental health providers, I felt that this is exactly the type of community I want to serve long-term. I believe my background working in resource-limited settings and my comfort in small communities would be a good fit here.”
6. Application Logistics, Timing, and Backup Plans
Even with strong strategy, matching with low scores as an IMG is challenging. You need to manage logistics and expectations carefully.
6.1 Apply Early and Completely
- Submit ERAS on the first possible day if you can
- Late applications hurt IMGs more than U.S. graduates
- Ensure:
- All letters uploaded early
- MSPE (Dean’s letter) available at release if possible
- ECFMG certification process is underway as early as you qualify
6.2 Specialty Selection Strategy
Your chances improve if you choose specialties that are:
- Needed in Appalachia
- Historically more IMG friendly
These usually include:
- Family Medicine
- Internal Medicine (categorical)
- Psychiatry
- Pediatrics (somewhat less than IM/FM but still possible)
- Preliminary/Transitional Year (if you have a longer-term plan)
If you have very low scores and no U.S. experience, it may not be realistic to aim for:
- Dermatology
- Orthopedic surgery
- Ophthalmology
- Radiation oncology
- Integrated plastics
- Neurosurgery
However, internal medicine or family medicine in Appalachia can still lead to:
- Hospitalist careers
- Outpatient primary care
- Addiction medicine
- Geriatrics
- Palliative care
- Other fellowships from solid community programs
6.3 Realistic Expectations and Backup Options
Even with strong planning, some applicants will not match on first attempt. Plan proactively:
Consider:
- Research positions in areas like addiction, rural health, or health services
- Clinical research fellowships at institutions with ties to Appalachian programs
- U.S. clinical jobs that IMGs can hold (e.g., clinical research associate, scribe, clinical assistant in some settings)
Use this time to:
- Strengthen your CV
- Gain more U.S. references, ideally from Appalachia or similar communities
- Improve any weak language or communication skills
Do not:
- Take Step exams repeatedly without a realistic improvement plan
- Accumulate long gaps without explanation or productive activity
If you reapply:
- Update your personal statement to show growth in the last year
- Highlight any new experiences specifically tied to rural or underserved care
FAQs: Low Step Score Strategies for IMGs in Appalachia
1. Can I match into a West Virginia or Kentucky residency with a very low Step 1 score if my Step 2 CK is stronger?
Yes, it is possible—especially in primary care–oriented Appalachian residency programs—if:
- Your Step 2 CK shows clear improvement over Step 1
- You have solid U.S. clinical experience, ideally in community or underserved settings
- Your letters strongly endorse your clinical competence and work ethic
- You clearly articulate your commitment to Appalachia and rural health in your personal statement and interviews
While no program can guarantee an interview, some West Virginia and Kentucky residency programs are open to candidates with uneven exam histories if the rest of the application is strong and mission-aligned.
2. How many programs should I apply to as an IMG with below average board scores targeting Appalachia?
Most IMGs with low Step scores should apply broadly, usually 80–120 programs total, with:
- 60–70% in community-based or community-affiliated programs in Appalachia and similar regions
- 20–30% in other IMG-friendly states (e.g., parts of the Midwest and South)
- 5–10% in slightly more competitive or academic programs where you have a unique connection or fit
Within Appalachia, aim to apply to all realistically IMG-friendly programs in West Virginia, Kentucky, and neighboring states that do not explicitly screen out your score range.
3. Should I directly explain my low score in my personal statement?
Yes, but briefly and strategically:
- One short paragraph is usually enough
- Acknowledge the low score and, if appropriate, provide concise context
- Focus more on what you learned, how you changed your approach, and how your later performance and clinical work reflect that growth
- Avoid over-focusing on it; the main theme of your statement should be your motivation, resilience, and commitment to Appalachia, not your exam history
Programs want to see insight and maturity, not excuses.
4. Is it necessary to have clinical experience specifically in Appalachia to match there?
Not absolutely necessary, but it helps considerably. If you cannot secure rotations in Appalachia, you should:
- Obtain USCE in similar community or underserved settings elsewhere in the U.S.
- Demonstrate knowledge of Appalachian health issues (rural access, substance use, chronic disease) in your essays and interviews
- Show that you genuinely prefer rural or semi-rural communities over large urban centers
Actual time spent in West Virginia, Kentucky, or nearby Appalachian areas—even for short electives, conferences, or observerships—can significantly strengthen your credibility and signal that you’re likely to stay and serve the region long-term.
By combining thoughtful program targeting, a clear Appalachian-focused narrative, strong U.S. clinical experiences, and confident, honest communication about your low Step scores, you can create a competitive application that resonates with the needs and values of residency programs across Appalachia—especially in West Virginia and Kentucky.






















