
When many future physicians picture their careers, they imagine themselves diagnosing complex cases, performing procedures, or leading clinical research. Yet one of the most powerful ways to shape the future of Healthcare is through medical education—specifically, by becoming a medical educator. These professionals do far more than give lectures; they design learning experiences, mentor trainees, advance educational research, and connect academic medicine with community needs.
This expanded guide explores the modern role of the medical educator—beyond the classroom—highlighting core responsibilities, required skills, and practical pathways for students, residents, and early-career clinicians who want to contribute to Medical Education and Curriculum Development while maintaining a meaningful clinical identity.
The Evolving Role of Medical Educators in Modern Healthcare
Medical educators sit at the intersection of clinical practice, education, and systems-based Healthcare improvement. They function as:
- Architects of training programs that determine what future clinicians know and can do
- Translators of evidence into practical teaching and assessment methods
- Mentors helping learners navigate high-stakes transitions (premed to medical school, medical school to residency, residency to practice)
- Leaders in Community Engagement, connecting academic centers to local health needs
Why Medical Educators Are Central to Healthcare Quality
The quality of patient care across a health system is directly tied to the quality of training clinicians receive. Thoughtful, evidence-based medical education:
- Improves diagnostic reasoning and patient safety
- Reduces preventable errors
- Supports health equity by embedding social determinants and bias mitigation into the curriculum
- Ensures clinicians are prepared for emerging challenges (AI, telemedicine, pandemics, climate-related health issues)
Becoming a medical educator is not a “step away” from medicine—it is a way to magnify your impact across hundreds or thousands of future practitioners and their patients.
Core Responsibilities of Medical Educators
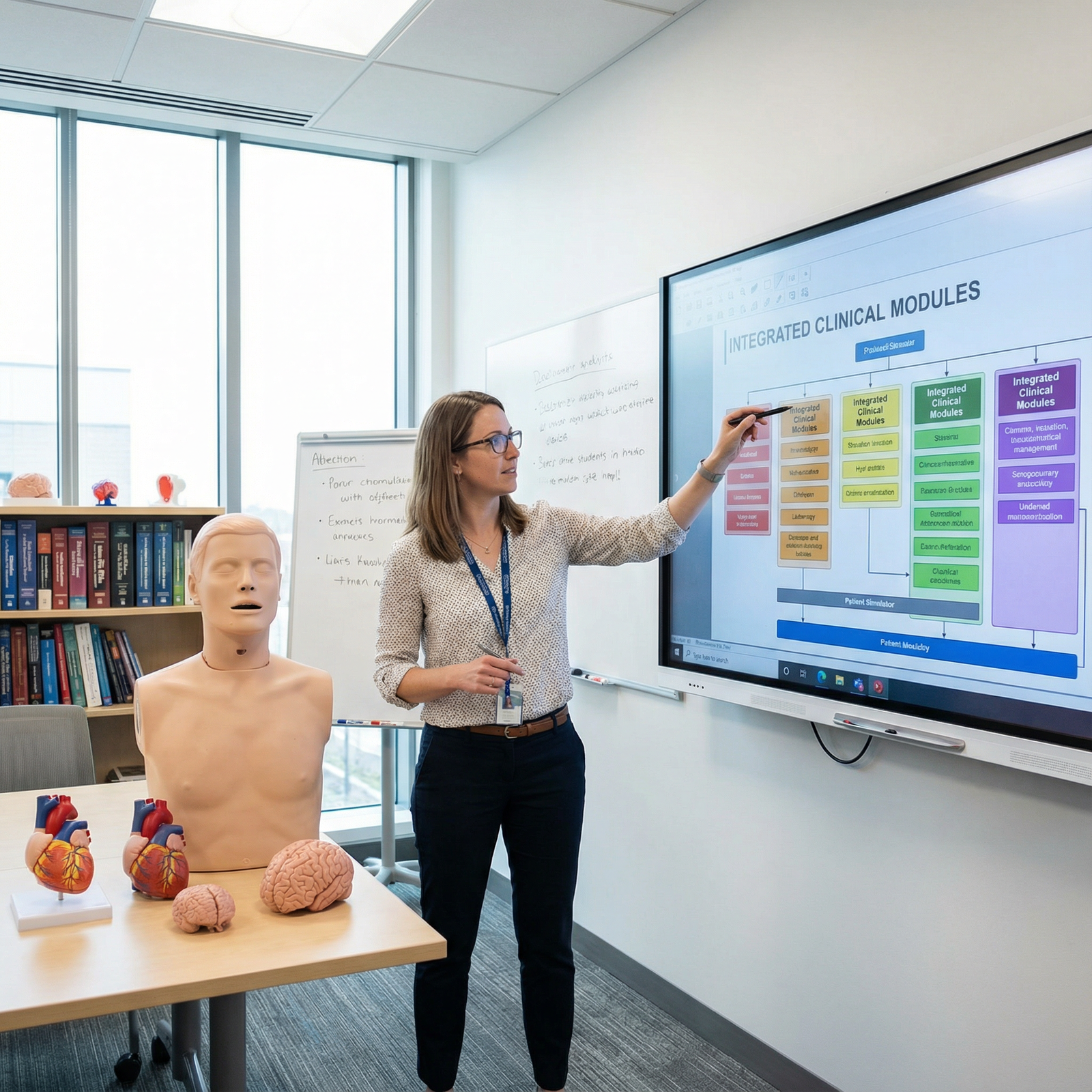
Medical educators work in medical schools, teaching hospitals, residency programs, simulation centers, public health departments, and community organizations. While job titles vary (clerkship director, residency program director, skills lab faculty, simulation director, Dean of Education), their responsibilities tend to cluster into several key domains.
1. Curriculum Development and Instructional Design
Curriculum Development is one of the most visible and strategic responsibilities of medical educators. Rather than simply “covering content,” today’s educators design competency-based curricula that are:
- Aligned with national standards (e.g., ACGME competencies, CanMEDS, EPAs)
- Integrated across basic science, clinical medicine, and systems-based practice
- Inclusive of health equity, ethics, professionalism, and communication skills
Key tasks include:
Designing and mapping courses
- Defining learning objectives that are specific, measurable, and tied to competencies
- Aligning lectures, small-group sessions, labs, and clinical encounters with those objectives
- Creating longitudinal threads (e.g., ethics, social determinants of health, quality improvement) that are revisited across the curriculum
Integrating technology and active learning
Medical educators increasingly use:- Learning management systems (e.g., Canvas, Moodle) to organize materials and track progress
- Virtual patients and online cases to supplement clinical exposure
- Simulation (mannequins, standardized patients, task trainers) to practice procedures and communication in a safe environment
- Flipped classroom approaches where students review key content before class and use in-person time for higher-level application
Ensuring regulatory and accreditation compliance
- Aligning courses and rotations with LCME, ACGME, or other accrediting body requirements
- Documenting how competencies are taught and assessed
- Responding to program evaluation data and accreditation feedback by revising curricula
Example: Transforming a Skills Course Through Simulation
Dr. Smith, a general surgeon and medical educator, recognized that students had limited hands-on practice with basic surgical skills before entering the OR. He led a curriculum redesign that:
- Introduced a longitudinal simulation-based skills lab (suturing, knot tying, sterile technique) starting in the pre-clinical years
- Embedded deliberate practice sessions with immediate faculty feedback
- Implemented objective skills checklists and milestones to track progress
Within two years, OSCE performance and resident evaluations of incoming interns showed marked improvements in procedural readiness and confidence. This is Curriculum Development directly translating into better patient care.
2. Teaching, Coaching, and Mentorship in Medical Education
Beyond course design, medical educators spend substantial time in direct teaching and Mentorship, often spanning the continuum from pre-medical learners to attending physicians engaged in continuing Medical Education.
Direct Teaching Responsibilities
Lecturing and large-group sessions
- Delivering high-yield, clinically integrated talks
- Using audience response systems or polling tools to keep learners engaged
- Framing content around clinical vignettes and cases rather than isolated facts
Facilitating small groups and case-based learning
- Leading problem-based learning (PBL) or team-based learning (TBL) sessions
- Encouraging clinical reasoning by having students articulate differentials, justify choices, and identify knowledge gaps
- Managing group dynamics, ensuring quieter learners participate and dominant voices do not overshadow others
Clinical teaching in real patient settings
- Bedside rounding that models patient-centered communication
- Teaching on-the-fly during admissions, consults, and procedures
- Demonstrating how to integrate evidence, guidelines, and patient preferences in decision making
Mentorship and Coaching
Mentorship is one of the most influential aspects of a medical educator’s work. It extends beyond answering academic questions to supporting learners’ professional identity formation.
Medical educators may:
- Help students choose specialties and navigate the residency application process
- Guide residents through career decisions (fellowship vs. general practice, academic vs. community career paths)
- Support mentees in research, quality improvement, or Community Engagement projects
- Provide longitudinal coaching around wellness, resilience, and workload management
Real-World Mentorship Example
Dr. Johnson, a hospitalist and medical educator, mentored Maria, a third-year medical student interested in internal medicine but unsure about an academic career. Over two years, Dr. Johnson:
- Co-designed a clinical research project with Maria on hospital readmissions
- Coached her through writing an abstract and presenting at a regional meeting
- Provided honest feedback on clinical skills and communication style
- Discussed lifestyle, career satisfaction, and leadership opportunities in academic medicine
Maria ultimately matched into an internal medicine residency with a strong medical education track and later became a chief resident—continuing the Mentorship chain with her own students.
For residency applicants and early trainees, identifying and working with medical educators as mentors can transform your trajectory. Seek out faculty who are clearly invested in education and ask how you can get involved in teaching or scholarly projects.
3. Assessment, Feedback, and Program Evaluation
High-quality assessment is central to safe and effective Healthcare. Medical educators are responsible not only for testing knowledge but for ensuring learners achieve clinical competence and professional behaviors.
Designing Robust Assessments
Medical educators develop and oversee:
Knowledge assessments
- Multiple-choice exams, SAQs, and open-book assessments
- Question banks aligned with board exam blueprints
- Integrated exams that test across disciplines
Skills and performance assessments
- OSCEs (Objective Structured Clinical Examinations) for history taking, physical exams, and counseling
- Direct observation tools (e.g., Mini-CEX, workplace-based assessments) during real clinical encounters
- Simulation-based assessments for emergencies, procedures, and teamwork
Competency and milestone tracking
- Using standardized frameworks (e.g., EPAs—Entrustable Professional Activities) to document readiness for unsupervised practice
- Working with Clinical Competency Committees (CCCs) to review resident progression and identify struggling learners early
Providing Effective Feedback
One of the most powerful educational tools is timely, specific feedback. Skilled medical educators:
- Use structured frameworks (e.g., pendleton rules, SBI—Situation, Behavior, Impact)
- Balance reinforcing strengths with targeted areas for growth
- Co-create improvement plans with learners, setting clear, achievable goals
- Normalize feedback as a routine, growth-oriented part of training—not a punitive event
Evaluating Educational Programs
Beyond individual learner assessment, medical educators also:
- Analyze exam scores, OSCE performance, and survey data to identify curricular gaps
- Conduct program evaluations using quantitative and qualitative methods
- Implement quality improvement cycles (Plan–Do–Study–Act) to refine teaching methods and rotation structures
For those interested in academic leadership, expertise in assessment and evaluation is a major asset and often leads to roles such as course director, clerkship director, or program director.
4. Research, Scholarship, and Innovation in Medical Education
Medical educators are also scholars. Educational scholarship is now recognized as a core pathway to promotion in many academic centers, on par with traditional clinical or basic science research.
Types of Educational Scholarship
Medical educators contribute through:
Educational research
- Studying the effectiveness of teaching strategies (e.g., flipped classroom vs. traditional lectures)
- Evaluating simulation-based training impact on patient outcomes
- Investigating burnout, wellness, and learning climate
Curricular and program innovation
- Designing new learning experiences (e.g., interprofessional education with nursing and pharmacy students)
- Developing assessment tools, rubrics, or evaluation frameworks
- Creating e-learning modules, podcasts, or interactive cases that are widely disseminated
Scholarship of integration and application
- Synthesizing literature to create best-practice guidelines for teaching or assessment
- Applying educational theory to clinical teaching (e.g., cognitive load theory, deliberate practice, mastery learning)
Example: Research Impact on Early Clinical Exposure
Dr. Lee, a pediatrician and medical educator, studied whether introducing structured clinical exposure in the first year of medical school improved later clerkship performance. His multi-year study found that:
- Students with early, guided patient contact performed better in communication OSCEs
- They reported less anxiety transitioning to clinical rotations
- Faculty rated them as more patient-centered and professional
These findings led his institution to redesign the preclinical curriculum to embed early clinical experiences, and his work was adopted as a model by other schools internationally—illustrating how educational research can reshape training at scale.
Funding and Dissemination
Medical educators often:
- Apply for educational grants (institutional, foundation, or government) to support innovation
- Present at regional, national, and international conferences in Medical Education
- Publish in education-focused journals (e.g., Academic Medicine, Medical Teacher, Medical Education)
If you are a resident or student, joining an education research project is an excellent way to explore academic career paths while strengthening your CV for residency or fellowship.
5. Community Engagement, Equity, and Social Accountability
Modern medical education increasingly emphasizes Community Engagement and social accountability. Medical educators play a crucial role in ensuring that training programs reflect the needs of the populations they serve.
Key Activities in Community Engagement
Designing community-based rotations
- Partnering with community clinics, FQHCs, rural hospitals, and public health departments
- Building experiences where learners understand social determinants of health, resource limitations, and culturally responsive care
Leading public health and education initiatives
- Organizing health fairs, screening campaigns, vaccination drives, and school-based health education
- Training students and residents to communicate health information effectively to non-medical audiences
Advocating for health equity
- Integrating topics like structural racism, implicit bias, LGBTQ+ health, disability, and migrant health into the curriculum
- Supporting service-learning projects and longitudinal community partnerships
- Encouraging learners to engage in policy advocacy and health system improvement
Community Example: Health Fair as a Teaching Platform
Dr. Ramirez, a family medicine educator, spearheaded an annual community health fair focusing on hypertension, diabetes, and preventive care in an underserved neighborhood. Her role included:
- Training students and residents to take blood pressure, counsel patients on lifestyle changes, and connect community members to follow-up care
- Collaborating with local organizations, faith leaders, and advocacy groups
- Using the event as a practical teaching platform for communication skills, cultural humility, and interprofessional teamwork
The health fair improved community screening rates while also giving trainees a deeper understanding of real-world barriers patients face—an essential component of comprehensive Medical Education.
For residents and students, engaging in such projects can demonstrate commitment to Community Engagement and health equity, which is increasingly valued in residency and faculty recruitment.
Essential Skills and Competencies for Effective Medical Educators
To succeed in these varied roles, medical educators need a broad, evolving skill set that goes beyond clinical excellence.
1. Advanced Communication and Teaching Skills
- Explaining complex topics at the appropriate level for learners
- Storytelling to make abstract concepts memorable
- Using questioning strategies that promote critical thinking rather than pure recall
- Adapting explanations based on real-time learner feedback
2. Leadership, Collaboration, and Change Management
Medical educators frequently lead multidisciplinary teams and projects, requiring:
- Skills in team building and collaborative decision-making
- Negotiation and conflict resolution among faculty, departments, and learners
- Change management abilities to implement new curricula or assessment systems in often resistant environments
Participation in committees (Curriculum Committees, Graduate Medical Education Committees) and educational leadership programs can build these competencies.
3. Critical Thinking, Problem-Solving, and Systems Perspective
Educational challenges are often complex and systems-based:
- Addressing high failure rates in a course may require examining assessment design, teaching methods, and learner supports
- Improving resident handoffs may demand coordination across departments, not just one lecture
Medical educators must analyze data, identify root causes, and design interventions with measurable outcomes.
4. Adaptability, Lifelong Learning, and Professional Development
Medical Education and Healthcare are rapidly changing:
- New technologies (AI, clinical decision support tools, VR/AR for simulation) regularly emerge
- Accreditation standards and competency frameworks evolve
- Learner expectations and diversity continue to shift
Effective educators commit to lifelong learning, attending faculty development workshops, pursuing advanced degrees or certificates in education, and regularly updating their teaching practices based on evidence.
5. Educational Scholarship and Reflective Practice
Strong medical educators:
- Reflect critically on their teaching, seeking feedback from learners and peers
- Collect data on the outcomes of their educational interventions
- Share their work with the broader Medical Education community, contributing to collective improvement
For residency applicants and new attendings, demonstrating these behaviors early—through teaching electives, certificate programs in medical education, or local workshops—can distinguish you as a future leader in academic medicine.

Pathways Into a Career in Medical Education
Whether you are a medical student, resident, fellow, or practicing clinician, it is possible to intentionally cultivate an education-focused career.
During Medical School
- Serve as a peer tutor or anatomy TA
- Volunteer to lead review sessions or develop study resources
- Join curriculum committees or student-faculty education workgroups
- Seek mentorship from faculty known for their teaching and ask to assist with educational projects
During Residency and Fellowship
- Participate in “resident-as-teacher” programs
- Lead teaching rounds and intern teaching conferences
- Collaborate on education research or quality improvement projects with an educational component
- Explore formal tracks or fellowships in Medical Education if available
Early Faculty Career
- Negotiate for protected time for teaching and educational scholarship
- Enroll in certificate programs, a Master’s in Health Professions Education, or similar degrees
- Take on roles such as course director, clerkship director, or associate program director when ready
- Build a coherent portfolio highlighting teaching excellence, curriculum contributions, and scholarship for promotion
FAQs About Careers in Medical Education
1. What qualifications do medical educators typically need?
Most medical educators hold an MD, DO, or equivalent degree and maintain some level of clinical practice. Increasingly, institutions value additional training in education such as:
- Master’s degrees in Medical Education, Health Professions Education, Public Health, or related fields
- Graduate certificates in curriculum design, assessment, or educational leadership
- Participation in faculty development programs focused on teaching, feedback, and assessment
However, you do not need an advanced degree to begin teaching. Many clinicians start by informally teaching students and residents, then build their educational expertise over time.
2. How do medical educators balance teaching, clinical work, and research?
Workload balance varies by role:
- Some educators are primarily clinicians with a smaller teaching component (e.g., precepting on wards or in clinic).
- Others have education-focused positions with significant protected time for Curriculum Development, assessment, and research.
- Academic contracts often specify percentages (e.g., 60% clinical, 30% education, 10% research/administration).
Balancing these roles requires clear communication with department leadership, time management, and strategic choices about which projects to pursue. Many educators integrate teaching with clinical care (e.g., bedside teaching, case discussions in real time) to maximize impact.
3. What impact can a medical educator have on student and patient outcomes?
Medical educators influence:
- Individual learners: shaping knowledge, skills, professional identity, and resilience
- Training programs: improving curricula, learning climate, and assessment systems
- Patient care: by ensuring that graduates are competent, compassionate, and prepared for complex healthcare systems
Research has shown that high-quality education and supervision are linked to better patient outcomes, fewer errors, and improved team communication—making the educator’s role directly relevant to patient safety and quality.
4. Are there clear opportunities for advancement and leadership in medical education?
Yes. Medical education offers robust leadership pathways, including:
- Course, clerkship, and rotation director roles
- Residency or fellowship program director and associate program director positions
- Director of Simulation or Skills Lab
- Vice Chair for Education in a department
- Associate Dean or Dean for Undergraduate, Graduate, or Continuing Medical Education
Progression typically involves building a portfolio of successful teaching, Curriculum Development, mentorship, and scholarship.
5. How can I get started if I’m interested in becoming a medical educator?
Actionable steps include:
- Tell a trusted faculty member or program director about your interest in education
- Volunteer for small teaching roles (case discussions, review sessions, skills labs)
- Join education committees or workgroups at your institution
- Participate in local or national Medical Education conferences and workshops
- Seek mentors who have built successful education careers and ask to collaborate on a small project (curriculum, assessment, or community initiative)
Over time, you can grow from enthusiastic teacher to recognized expert, contributing meaningfully to Medical Education, Healthcare quality, and Community Engagement.
By understanding the full scope of what medical educators do—beyond delivering lectures—you can better appreciate their essential role in shaping the next generation of clinicians and in improving Healthcare systems. Whether you aspire to a full-time career in Medical Education or simply want to integrate teaching and Mentorship into your clinical life, the opportunities to make a lasting impact are substantial, meaningful, and deeply rewarding.




















