
Choosing a medical specialty during a transitional year residency (TY program) can feel both exciting and overwhelming. You’re finally a doctor, but you’re also staring at a near-final decision that will shape your career, lifestyle, and identity for decades. This guide is designed to help you use the transitional year intentionally so you can move from “What specialty should I do?” to a confident, well-reasoned decision.
Understanding the Transitional Year: What It Is and What It Isn’t
A transitional year residency is a one-year, broad-based clinical training program that typically precedes advanced specialty training. It’s commonly used as a prelim year for:
- Anesthesiology
- Radiology and interventional radiology
- Dermatology
- Neurology
- Physical medicine & rehabilitation (PM&R)
- Ophthalmology
- Radiation oncology
- Some advanced internal medicine or family medicine pathways
The Purpose of a Transitional Year
TY programs are designed to:
- Provide a solid foundation in inpatient and outpatient medicine
- Expose you to a variety of specialties and practice settings
- Help you refine clinical reasoning, professionalism, and procedural skills
- Allow flexibility in rotations and electives (in many, but not all, programs)
Because the curriculum can be more varied than a preliminary medicine or surgery year, a transitional year residency is uniquely suited to students who are still clarifying their long-term career path—even if they’ve already secured an advanced spot.
What a Transitional Year Is Not
- It is not a substitute for long-term specialty exploration you should have started in medical school. It’s a refinement phase, not the starting line.
- It is not a guaranteed way to “audition” for any and all specialties. Rotations must be scheduled strategically and are limited by program resources.
- It is not a year off. The clinical workload can be equivalent to other PGY-1 positions, with night float, call, and significant responsibility.
Understanding these boundaries helps you use your TY program effectively in your journey of choosing medical specialty rather than drifting through the year.
Foundations First: Clarifying Your Values, Strengths, and Constraints
Before you analyze individual specialties, step back and clarify who you are and what you want your life to look like. Your transitional year can give you data, but you need a framework to interpret that data.
1. Core Values: What Actually Matters to You?
Reflect honestly on the elements of work and life you care about most. Some key dimensions:
- Patient Relationship Style
- Longitudinal vs episodic care
- Acute vs chronic disease focus
- Procedural vs cognitive-heavy interaction
- Degree of Hands-On Procedures
- Do you enjoy using your hands and tools?
- Are you energized by procedures, or do they add stress?
- Intellectual Style
- Pattern recognition (e.g., radiology, dermatology)
- Complex diagnostic puzzles (e.g., internal medicine, neurology)
- Rapid decision-making under pressure (e.g., EM, critical care, surgery)
- Work–Life Integration
- Hours and call schedule
- Predictability vs variability
- Flexibility for family, hobbies, or non-clinical pursuits
- Team and Environment Preferences
- Large interdisciplinary teams vs small, focused teams
- OR-based vs clinic-based vs imaging suite vs bedside
- Amount of “alone time” vs constant interaction
Write these down. Rank your top 3–5 values. During your transitional year, use this as your “scorecard” for each rotation.
2. Strengths, Personality, and Skills
Some specialties are more forgiving of a mismatch than others. Still, you’ll be happiest where your natural strengths align with the core demands of the field.
Consider:
- Temperament
- Do you thrive under pressure or prefer controlled environments?
- Are you detail-obsessed, big-picture oriented, or both?
- Communication Style
- Love counseling and patient education? Think primary care, psychiatry, oncology.
- Enjoy high-yield, focused interactions? Think anesthesiology, emergency medicine.
- Cognitive Strengths
- Visual-spatial skills? Consider surgery, radiology, dermatology.
- Systems thinking and complexity? Consider internal medicine subspecialties, critical care, neurology.
- Manual Dexterity and Stamina
- Comfort standing for long OR cases
- Fine motor control and coordination
Personality metrics (e.g., Myers–Briggs, Big Five) are imperfect but may give clues. The key is honest reflection, not forcing yourself into a stereotype of “the typical ___ doctor.”
3. Constraints and Practical Realities
You cannot ignore real-life circumstances:
- Geographic limitations (family obligations, partner’s career)
- Financial pressure (educational debt, need for early earning potential)
- Length of training (e.g., dermatology vs family medicine timelines)
- Competitiveness and your application profile (scores, research, letters)
A TY year cannot change your past, but it can help you strategically reposition, strengthen your application, and build a realistic plan.
Using the Transitional Year Strategically to Explore Specialties
Once you’ve clarified your values and constraints, design your transitional year experience to gather targeted information about specialties.

Know Your TY Program’s Structure
Transitional year programs vary significantly. Early in PGY-1 (or even before starting), clarify:
- Required core rotations (e.g., inpatient medicine, ICU, emergency medicine)
- Available electives and how many months are flexible
- Policies on away rotations or external electives
- Opportunities for research, QI projects, or teaching
- Application support if you are applying (or re-applying) to a specialty
This helps you see how much room you have to explore and which months to protect for decision-critical experiences.
Build a Thoughtful Rotation Strategy
If you’re undecided or between multiple options, don’t simply take “whatever’s open.” Instead:
Identify 2–3 serious specialty contenders
Use your pre-residency experiences plus your value framework to narrow your list. If you’re between, say, anesthesiology, EM, and IM, that’s manageable. Ten options is not.Plan at least one focused elective in each contender specialty
Ideal timing:- Early/mid-year if you might apply for that year’s match or SOAP
- Mid/late-year if you’re planning to apply in the next cycle, allowing time to gather letters and insight
Include “adjacent” specialties
For example:- Considering surgery but unsure? Add surgical subspecialty clinics, anesthesia, or critical care.
- Thinking radiology? Consider neurology, cardiology, or emergency medicine to see how imaging fits clinically.
Preserve at least one “values check” rotation
Take a rotation that emphasizes what you think you don’t like to confirm your assumptions. You might be surprised.
Questions to Ask Yourself on Every Rotation
Carry a small notebook or use a notes app. For each rotation, reflect weekly on questions like:
- Am I energized or drained at the end of the day?
- Do I look forward to this work when I wake up?
- How do I feel about:
- The pace of the day?
- The types of decisions I’m making?
- The patient population?
- Can I imagine doing this core work most days for 20–30 years?
- How do attendings/fellows talk about their career satisfaction?
Record specific anecdotes:
- “Loved coordinating complex care for a sick ICU patient.”
- “Dreaded clinic days.”
- “Felt most alive in the OR.”
These details are much more informative than vague impressions remembered months later.
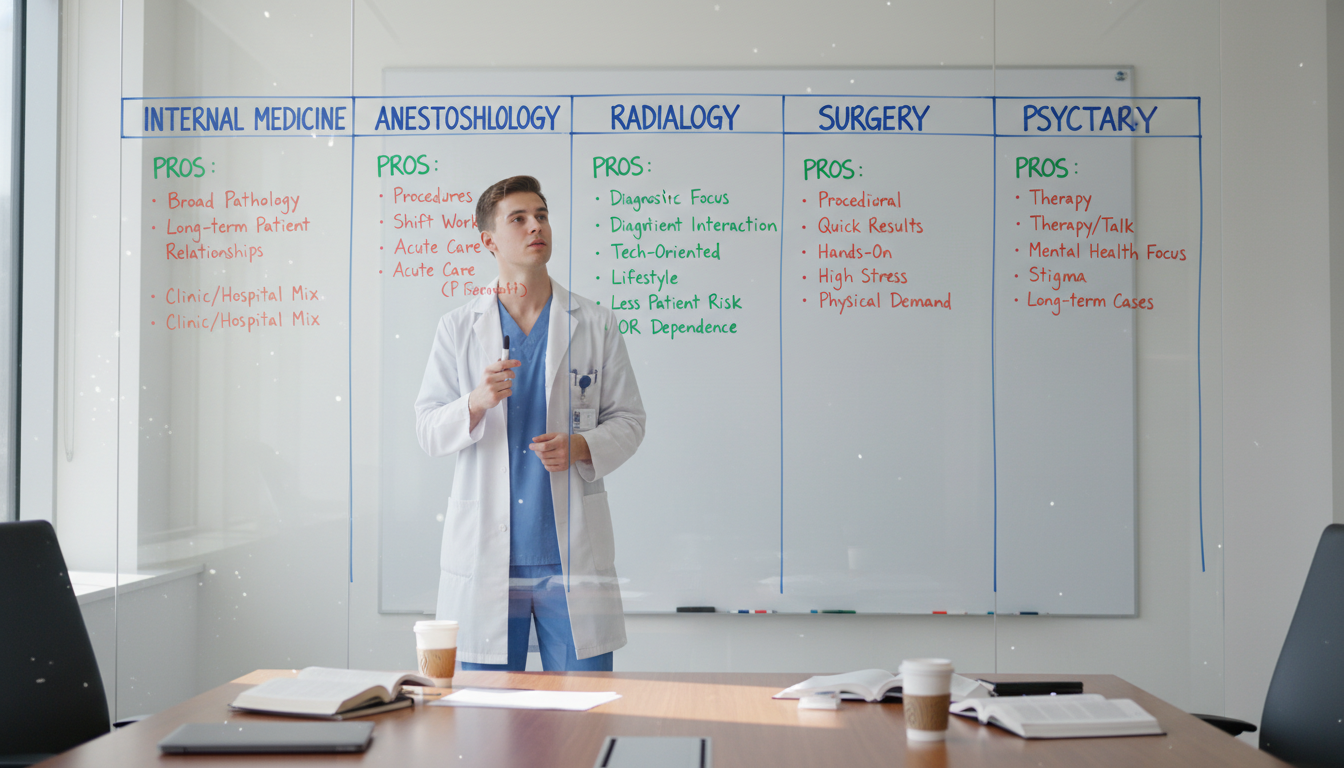
Deep Dive: How to Compare and Evaluate Potential Specialties
This is where “how to choose specialty” becomes concrete. Instead of ranking specialties by reputation, use structured criteria.
1. The Nature of the Daily Work
Shadowing in med school shows you moments; residency shows you patterns. During TY, assess:
Internal Medicine / Primary Care Pathways
- Core activities: Diagnostic reasoning, chronic disease management, frequent communication and coordination.
- Ask: Do I enjoy synthesizing complex histories and data into a plan? Do long-term relationships matter to me?
Surgical Specialties
- Core activities: OR time, perioperative care, procedures, physical stamina.
- Ask: Do I genuinely like being in the OR? How do I feel about the culture and hierarchy? Does the satisfaction of a technically successful case outweigh long hours?
Anesthesiology
- Core activities: Pre-op assessment, intra-op monitoring, airway management, acute pain management.
- Ask: Am I comfortable with high-acuity events and rapid response? Do I like short, focused patient interactions and procedural work?
Radiology
- Core activities: Image interpretation, pattern recognition, communication with clinicians, often less direct patient contact.
- Ask: Am I comfortable working in relatively lower face-to-face patient contact? Do I like long stretches of focused visual work and “spot the abnormality” thinking?
Emergency Medicine
- Core activities: Rapid triage, acute care, broad differential diagnoses, shift work.
- Ask: Does the continuous influx of undifferentiated patients feel exciting or exhausting? How do I tolerate night shifts and schedule variability?
Neurology, Psychiatry, PM&R, etc.
- Consider the core patient populations, disease trajectories, and procedural vs cognitive balance in each.
Use a simple scoring system (1–5) for each specialty on dimensions like “Enjoyment of daily tasks,” “Fit with personality,” and “Sustainable lifestyle.”
2. Lifestyle and Work–Life Integration
Avoid relying solely on stereotypes (“Dermatologists leave at noon”). Instead, during rotations:
Ask attendings at different career stages:
- What does your average week look like?
- How often are you on call, and what does call look like?
- How flexible is your schedule for family or outside interests?
Observe residents:
- Are they chronically exhausted or generally steady?
- How do they talk about their hours and stress?
Remember: within any specialty, job structure (academic vs private, inpatient vs outpatient) can drastically change lifestyle. Focus on the range of realistic options, not just extremes.
3. Training Length and Competitiveness
Your transitional year is a good time to be brutally honest about where you stand:
Training length
- IM/FM: typically 3 years
- Pediatrics: 3 years
- EM: typically 3–4 years
- Surgical specialties: 5–7+ years with fellowships
- Subspecialties of IM: 3 + 2–3 years fellowship
Competitiveness and your profile
- Board scores (if still relevant for your application year)
- Medical school performance and class rank
- Research output in the field
- Strength and specificity of letters of recommendation
Consult mentors and program leadership early in your transitional year: “Given my file, how realistic is [specialty X] and what can I do this year to strengthen my application?”
4. Career Prospects and Flexibility
Look beyond residency:
- Job market in your desired geographic area
- Flexibility to shift practice focus (e.g., outpatient vs inpatient, academic vs community)
- Non-clinical opportunities: administration, education, research, industry, health policy
For example:
- Internal medicine offers broad flexibility (hospitalist, clinic-based, subspecialties).
- Radiology and anesthesia offer strong demand in many regions with varied practice styles.
- EM faces local market variations and evolving workforce concerns.
You don’t need perfect certainty, but a general sense of long-term viability helps prevent late-career dissatisfaction.
Making the Decision: From Exploration to Commitment
By mid-to-late transitional year, you’ll likely be down to 1–2 serious specialty contenders. This is where you move from data gathering to decision-making.
Step 1: Synthesize Your Experiences
Create a simple comparison table for your top choices. Columns as specialties; rows as:
- Enjoyment of daily work
- Alignment with top 3–5 values
- Lifestyle fit (hours, call, predictability)
- Training length vs personal timeline
- Competitiveness vs your current CV
- Long-term career flexibility
Assign a rating (1–5) and write short justifications. This exercise often clarifies things more than ruminating.
Step 2: Seek Targeted Mentorship
Move beyond generic advice:
- Identify 2–3 attendings or fellows in each specialty you’re considering who:
- Enjoy their work
- Are honest and approachable
- Have seen multiple career paths
Ask them:
- What do you love about this specialty—and what frustrates you?
- For someone with my interests and strengths [briefly describe], how do you think this field fits?
- If you were choosing again today, would you pick the same specialty? Why or why not?
Mentors in your transitional year residency program can also help you understand how others in your shoes made their decisions—and what they regret.
Step 3: Visualize a Day, a Week, and a Life
For each specialty, close your eyes and envision:
- Your typical day as an attending
- Your week in terms of clinic/OR/call/administration
- Your life 10–20 years out:
- Family situation, hobbies, community involvement
- Physical and mental bandwidth
Ask: Which future feels like a version of myself I’d be proud and happy to become?
Step 4: Accept Imperfection and Committing
No specialty will score a perfect “5” on all metrics. At some point, you choose:
- A working hypothesis: “Given everything I know, [specialty X] is the best fit, not a perfect fit.”
- A commitment to make that specialty work by choosing job settings aligned with your values.
For most physicians, satisfaction comes not from the “perfect specialty” but from building a practice, team, and lifestyle within a field that fits well enough.
Practical Application Timelines and Scenarios During TY
How you use your transitional year also depends on where you stand in the application process.
Scenario 1: You Matched an Advanced Specialty But Feel Unsure
Example: You’re in a TY program with a guaranteed PGY-2 spot in radiology, but you’re suddenly drawn to anesthesiology.
Actions:
- Use electives early in TY to test your doubts (e.g., anesthesia, critical care).
- Speak to your TY program director and the advanced program’s leadership as early as possible if your doubts persist.
- Explore feasibility of switching:
- Internal transfer within the same institution
- Re-applying to a different specialty in the next Match
- Clarify logistical and visa/contract implications.
Even if you ultimately stay in your advanced specialty, you’ll either:
- Confirm it’s the right choice, or
- Make a thoughtful plan for transition later (e.g., fellowship that shifts your practice focus).
Scenario 2: You’re Using TY as a Bridge After an Unmatched Cycle
You may be in a transitional year residency as a bridge after not matching into your desired specialty.
Actions:
- Early in PGY-1, reassess your specialty choice using the framework above: Was it truly the right fit, or mainly prestige-driven?
- Meet with advisors to recalibrate your specialty list if needed.
- Schedule key electives in your new or reaffirmed target specialty before ERAS opens, if you’re reapplying this cycle.
- Use your TY year to:
- Complete meaningful research or QI projects
- Build strong relationships for letters
- Demonstrate clinical excellence and professionalism
Scenario 3: You’re Genuinely Undecided Starting TY
If you’re still asking, “What specialty should I do?” at the start of transitional year:
- Narrow down to no more than 3 likely fits using values, strengths, and prior exposure.
- Front-load broad, high-yield rotations (medicine, EM, ICU) and then follow with targeted electives.
- Set a personal decision deadline (e.g., January if applying next cycle) to avoid endless indecision.
Use each month as a focused “data-gathering” period with written reflections and structured comparison.
Frequently Asked Questions (FAQ)
1. Can a transitional year residency really help me decide my specialty if I was unsure in medical school?
Yes—if you use it intentionally. A TY program offers more specialty variety than many categorical PGY-1 positions. By planning electives strategically, reflecting on each rotation, and seeking targeted mentorship, you can gather much more mature and realistic insight than you had as a medical student. What it cannot do is make the choice for you; it provides data, but you must interpret it using your values and priorities.
2. If I change my mind about specialty during my TY year, is it too late?
Not necessarily. The feasibility depends on:
- Whether you already have an advanced position
- The competitiveness of the new specialty
- Timing relative to the Match cycle
If you’re considering a switch:
- Talk early with your TY program director and mentors.
- Clarify options: internal transfer, re-entering the Match, or planning a later transition via fellowship.
- Use any remaining electives to get exposure and letters in the new field.
The earlier you act in the year, the more options you’ll have.
3. How many specialties should I realistically consider during my transitional year?
For meaningful exploration, limit yourself to 2–3 serious contenders. More than that tends to dilute your experience and create decision paralysis. Use your pre-TY experiences and self-reflection to create a short list, then test those options deeply rather than sampling every possible field superficially.
4. What if I still feel uncertain even after my transitional year?
Some degree of uncertainty is normal. Many physicians are ~70–80% sure when they commit. If you’ve:
- Honestly assessed your values and strengths
- Gained robust exposure to your leading contenders
- Spoken with trusted mentors
- Considered lifestyle, training, and long-term flexibility
…then choose the specialty that looks like the best overall fit, not a perfect one. Remember that within most specialties, you can refine your practice (e.g., outpatient vs inpatient, academic vs community) to better match your preferences over time. Career satisfaction is built over years, not decided in a single moment.
By approaching your transitional year residency as a structured exploration rather than a holding pattern, you can transform uncertainty about “what specialty should I do” into a grounded, confident answer. Use your TY program to gather real-world evidence, align your decision with your values and strengths, and chart a specialty path that supports not only the physician you want to be—but the life you want to live.






















