
Understanding Competitiveness in Fellowships
Preparing for a competitive fellowship begins with knowing what you’re really up against. “Competitive” is more than just a reputation—it reflects a combination of applicant volume, program capacity, and the specificity of skills required.
Highly sought-after internal medicine subspecialties include:
- Cardiology fellowship match
- GI fellowship competitiveness (Gastroenterology)
- Heme onc fellowship (Hematology/Oncology)
- Pulmonary/Critical Care (especially in academic centers)
- Allergy/Immunology and Rheumatology (fewer spots, often high academic bar)
What Makes a Fellowship Competitive?
Several factors drive competitiveness:
Supply vs. demand
- Many residents want a given specialty (e.g., cardiology)
- Limited number of fellowship positions nationally
- Programs often prefer candidates with clear subspecialty commitment
Procedure-heavy and lifestyle considerations
- Cardiology and GI offer procedural skills, higher earning potential, and diverse career paths (academic, hospital-based, private practice)
- These attract residents across the country, not just from internal medicine but sometimes from preliminary or transitional backgrounds with strong credentials
Research and academic expectations
- Certain fields (like heme onc fellowship) are highly academic, with a strong expectation of research productivity and scholarly potential
- Programs use research output and letters from academic mentors as screening tools
Institutional reputation
- Top-tier programs (nationally known academic centers) attract heavy interest even in less traditionally “competitive” fields
- Such programs often receive several hundred applications for a handful of positions
The Two Levels of Competitiveness
Think in terms of two layers:
Getting into the specialty at all
- Matching to any accredited fellowship in your chosen field
- Driven by your basic application strength: exam scores (if applicable), evaluations, letters, and research
Getting into your target tier of program
- Matching to a specific type of program (e.g., top-20 academic cardiology fellowship match vs primarily clinical community program)
- Driven by fine distinctions: number/quality of publications, strength of mentors, networking, and fit with program priorities
Your preparation strategy should address both levels: create a solid floor (you’re a clearly acceptable candidate for the specialty) and then build a ceiling (you’re competitive for your dream programs).
Building a Strong Foundation During Residency
Strong fellowship preparation starts from Day 1 of residency—even if you’re not sure of your field yet. Competitive fellowships look for evidence that you are:
- Clinically sound
- Professional and reliable
- Committed to your specialty
- Capable of scholarly work
Prioritize Clinical Excellence First
Programs rarely take a risk on someone with marginal clinical performance, regardless of research output.
Key elements:
Rotation evaluations
- Aim for consistent “exceeds expectations” or equivalent on core rotations
- Be the resident others trust on call: reliable, safe, and proactive
Milestones and CCC (Clinical Competency Committee) reports
- These influence how your PD and faculty think of you, which shapes your letters
- Address any early concerns (communication, documentation, timeliness) quickly
Board exams and in-training exams
- USMLE/COMLEX scores are less central after residency starts, but for competitive fellowships they may still be used as a quick screen
- In-training exams show your knowledge trajectory; use them to identify gaps and create a study plan
Actionable step:
Ask your program director (PD) or advisor by mid-PGY1 for candid feedback:
- “What specific things do I need to do over the next 12 months to be a top-tier candidate for a cardiology fellowship match / GI fellowship / heme onc fellowship?”
Document their feedback and revisit it twice yearly.
Choose Rotations Strategically
As early as PGY1, think ahead about:
Exposure to your target field
- Cardiology: CCU, cath lab observation, heart failure, electrophysiology
- GI: inpatient consults, hepatology, advanced endoscopy observation
- Heme/Onc: malignant heme, solid tumor, BMT, outpatient infusion
Working with potential letter writers
- Schedule elective rotations with faculty who are known mentors or division leaders
- Aim to work with them longitudinally rather than just two weeks: clinic + consults + project if possible
Balancing depth and breadth
- You still need to be a strong general internist; fellowship programs value residents with well-rounded internal medicine skills
- Don’t sacrifice core rotations or ICU exposure just to add one more specialty elective
Example:
A PGY2 interested in GI might plan:
- CCU and MICU in early PGY2 (foundation)
- GI consults and hepatology clinic in mid-PGY2
- A research elective in late PGY2 focused on outcomes in IBD or liver disease
Timing: When to “Commit” to a Specialty
Rough guide for a 3-year internal medicine residency:
- Early PGY1: Explore; keep 2–3 specialties in mind.
- Late PGY1: Narrow to 1–2; start talking to faculty in those divisions.
- Early PGY2: Commit to your top choice and begin targeted preparation (research, electives, mentor relationship).
- Late PGY2: Solidify your application (research output, letters, personal statement).
- PGY3 (application year): Apply, interview, and continue demonstrating commitment.
If you decide late (e.g., mid-PGY2), it’s still possible to build a competitive profile—but you’ll need a more focused and efficient strategy, especially around research and networking.
Research, Scholarship, and Academic Productivity
For the most competitive fellowships, scholarly work is often the main differentiator between a good candidate and a standout.
How Much Research Do You Really Need?
There is no absolute number, but patterns by field:
Cardiology fellowship match
- Stronger programs often expect at least a couple of PubMed-indexed publications or major abstracts
- Topic in cardiology is preferred but not mandatory if the work is rigorous
GI fellowship competitiveness
- GI often has fewer positions and high academic expectations, especially at tertiary centers
- Programs may favor applicants with GI- or hepatology-focused work: case reports, outcomes research, or QI projects
Heme onc fellowship
- Typically among the most research-oriented; many applicants have 3–6+ publications, sometimes from pre-residency
- Bench, translational, or clinical research are all valued; oncology-adjacent topics still count
General guidance:
- Aim for at least 2–3 tangible scholarly outputs (abstracts, posters, manuscripts) with at least 1–2 in your intended field by the time you apply.
- Quality and ownership matter more than raw count. Being first author or playing a central role in study design/analysis is powerful.
Types of Scholarly Work That Count
You don’t need to run a randomized trial. Consider:
Case reports and case series
- Faster timeline; good starter projects
- Best when linked to an educational or diagnostic dilemma
- Useful for building writing skills and relationships with mentors
Retrospective chart reviews and outcomes studies
- High yield in cardiology, GI, and heme/onc
- Requires basic familiarity with stats and IRB processes
- Ideal for research electives during PGY2
Quality improvement (QI) projects
- Often built into residency; with good design and dissemination (poster, publication), they count as scholarship
- Example: Reducing time to antibiotics in neutropenic fever on heme/onc service
Review articles or book chapters
- Great for building subject matter familiarity
- Can be initiated by mentors with ongoing projects; show reliability and writing ability
Conference abstracts and posters
- Regional/national conferences in your field (ACC, ACG, ASH, ASCO, CHEST, ATS)
- Presentations are strong CV items and networking opportunities
Finding and Working with Research Mentors
Effective mentorship is more important than the specifics of your project.
Steps to find a good mentor:
Ask targeted questions
- “Who in cardiology/GI/heme-onc is productive with residents and has a track record of getting projects finished?”
- Ask senior residents who successfully matched in your field.
Approach mentors professionally
- Email with a clear subject line (e.g., “PGY1 interested in cardiology research opportunities”)
- In 1–2 short paragraphs, describe your background, interests, time availability, and timeline (e.g., aim for an abstract by next spring’s conference deadline).
Clarify expectations early
- Frequency of meetings
- Your role (data collection, analysis, writing)
- Authorship expectations (ask respectfully)
Deliver relentlessly
- Meet deadlines or communicate early if you’re falling behind
- Take ownership of tasks that move the project forward without waiting for step-by-step instructions
Actionable tip:
Maintain a one-page “project tracker” listing each project, mentor, status (idea/IRB/data collection/analysis/writing/submission), and next action. Review it every 2–4 weeks.
Letters of Recommendation, Mentorship, and Networking
Letters and relationships are critical in competitive fellowship preparation. For many program directors, they are the single most important part of your application.
Who Should Write Your Letters?
Most fellowships want 3–4 letters, typically:
- Program Director (PD) – often required
- Subspecialty Division Chief or senior faculty in your target field
- Primary research mentor in your chosen specialty
- Additional clinical faculty who know your work well
For cardiology, GI, and heme/onc fellowships, it is ideal to have at least two letters from within the specialty if possible.
Priority qualities in a letter writer:
- Knows you well clinically and/or academically
- Has a reputation in the field or within your institution
- Can comment on your growth, resilience, and future potential
How to Earn Strong, Detailed Letters
Strong letters are built over time:
Work longitudinally with key faculty
- Be on their service, then join clinic, then collaborate on a project
- Show progression: from learner to junior colleague
Make your work visible
- Send brief updates on project progress
- Share positive feedback you’ve received (e.g., “Dr. X mentioned my work on Y rotation; I’m grateful for your mentorship in that area.”)
Ask for a “strong” letter explicitly
- “Would you feel comfortable writing a strong letter of recommendation for my GI fellowship applications?”
- This gives faculty a chance to decline if they can’t write positively
Provide a “letter packet”:
- Updated CV
- Personal statement draft
- List of programs or program types you’re targeting
- Brief bullet list of key points you hope they can address (clinical strengths, research contributions, professionalism)
Networking Beyond Your Home Institution
For the most competitive fellowships, especially in GI or heme onc, external visibility helps:
Conferences
- Present posters or oral abstracts
- Introduce yourself to faculty whose work you admire; be specific about what you found valuable in their research
- Attend trainee or early-career sessions
Away electives or visiting rotations (where available)
- Particularly impactful if your home program lacks a strong division in your chosen field
- Treat them as “extended interviews”—be early, prepared, and professional every day
Email introductions
- Your PD or division chief may be willing to email colleagues at other institutions on your behalf
- These “soft endorsements” can make your application more memorable when reviewed
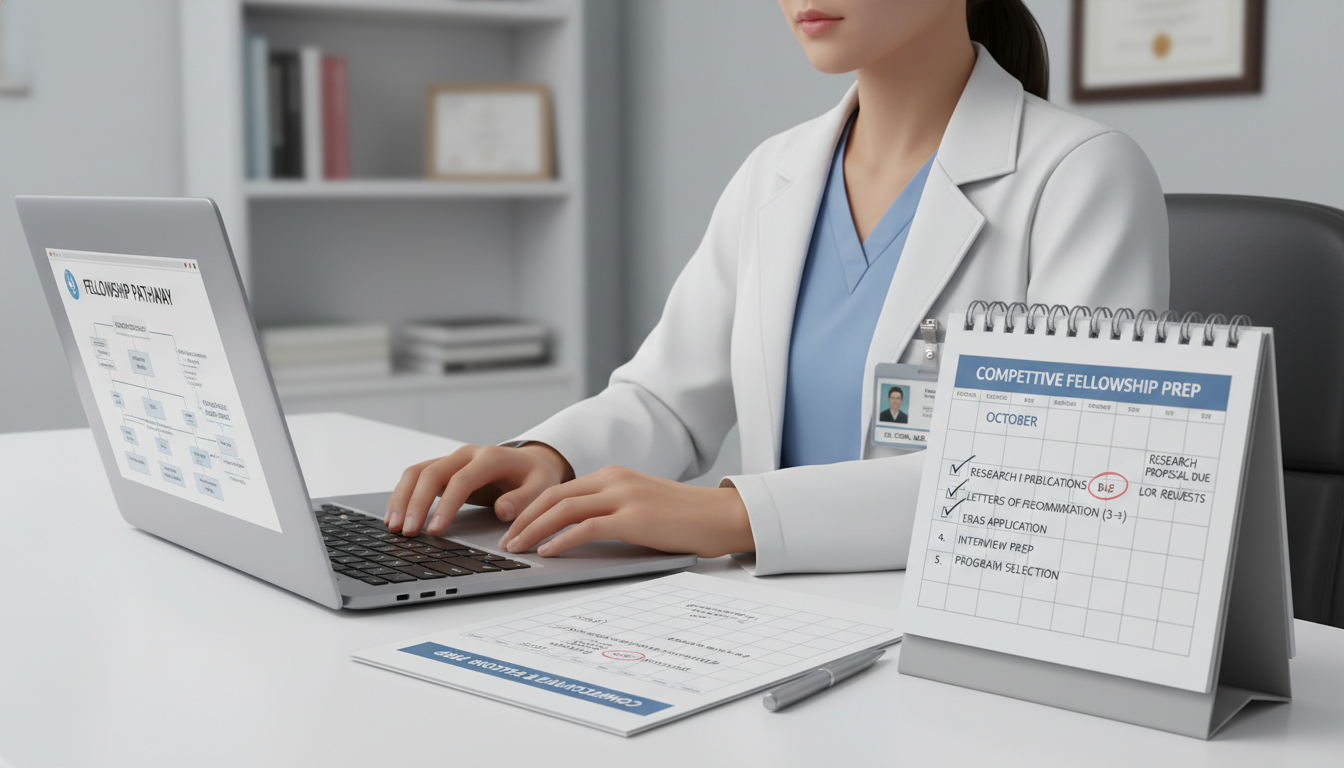
Crafting a Fellowship-Ready Application: Strategy and Execution
When application season arrives, your job shifts from building credentials to packaging them coherently.
CV and ERAS Application Strategy
Your CV should tell a consistent story: “I am a capable internist with clear, sustained commitment to [cardiology/GI/heme-onc] and the skills to contribute to your program.”
Key sections:
- Education and training
- Highlight honors, distinguishing achievements
- USMLE/COMLEX and in-training exams
- No need to over-emphasize; just list accurately
- Research and publications
- Organize consistently (peer-reviewed articles, abstracts, posters, book chapters)
- Use standard citation format; bold your name to highlight your role
- Presentations
- Local, regional, national—especially in your specialty
- Leadership and teaching
- Chief resident roles, curriculum development, teaching awards
- Volunteer work and advocacy
- Especially relevant for heme/onc and GI (e.g., cancer support groups, Crohn’s & Colitis Foundation events)
Writing a Convincing Personal Statement
Your personal statement should do three things:
- Explain why this specialty
- Demonstrate your preparation and trajectory
- Communicate what you will bring to their program
Structure:
- Opening vignette
- A concise, specific clinical experience that illustrates why the field matters to you (avoid generic “I realized the power of medicine” narratives)
- Development
- Show how your experiences (rotations, research, teaching) built your interest into a commitment
- Current strengths
- Highlight 2–3 concrete strengths: communication, analytic thinking, procedural aptitude, resilience
- Future goals
- Outline a realistic career vision (academic vs community, research vs clinical emphasis) while staying flexible
Tailoring by specialty:
- Cardiology: Emphasize analytic thinking, comfort with acuity, interest in longitudinal chronic disease management plus technology/procedures.
- GI: Highlight procedural interest, patient relationships in chronic GI/liver conditions, and multidisciplinary collaboration.
- Heme/Onc: Focus on communication, navigating uncertainty, longitudinal patient relationships, and interest in evolving therapies/research.
Avoid:
- Overly dramatic or tragic stories that center on you rather than the patient
- Rehashing your entire CV; choose 2–3 representative experiences instead
- Mentioning a specific program by name unless you are customizing for that program
Program List: How Broad Should You Apply?
Your application strategy should be realistic and diversified:
- Assess your competitiveness honestly
- Feedback from PD and subspecialty mentors is crucial
- Group programs into tiers
- Stretch: top-tier academic centers or highly renowned programs
- Target: solid academic or strong hybrid programs where your profile fits the typical matched applicant
- Safety: less research-heavy or community-focused programs that still provide robust training
Rule of thumb for highly competitive specialties:
- Cardiology fellowship match: many applicants apply to 40–60+ programs
- GI fellowship competitiveness: similar or slightly more, depending on your profile and region flexibility
- Heme onc fellowship: 30–50+ programs, with particular attention to research alignment if you’re academically focused
Adjust based on:
- Geographical flexibility
- Strength of your home institution
- Research portfolio and letters
Interview Season: Performing Effectively
Interviews are where your preparation is converted into impressions.
Before interviews:
- Review each program’s:
- Strengths (clinical volume, procedures, research infrastructure)
- Unique features (tracks, combined fellowships, global health, QI emphasis)
- Rehearse common questions:
- Why this specialty?
- Tell me about your research project.
- Describe a challenging patient or ethical dilemma.
- What are your career goals in 5–10 years?
- Prepare 3–5 specific questions for each program:
- About mentorship structure, scholarly requirements, procedural exposure, and alum outcomes
During interviews:
- Be authentic and consistent with your application narrative
- Balance confidence with humility; emphasize what you want to learn
- In group or social settings (virtual or in-person), be collegial and engaged—programs evaluate “fit” here
After interviews:
- Take structured notes within 24 hours: pros/cons, culture, research fit, location considerations
- Send short, sincere thank-you emails where appropriate (some programs may request you not do this; follow instructions)
Rank List Strategy
When it’s time to submit your rank list:
- Rank programs in your true preference order, not based on where you “think” you’ll match; the algorithm favors applicant preference.
- Incorporate:
- Training quality (breadth of exposure, procedural volume)
- Mentorship and research opportunities
- Culture and support (wellness, fellow autonomy, collegiality)
- Geography and personal life considerations
If you are couples matching with another fellowship applicant, work through scenarios early and be strategic—but still abide by genuine preferences as much as possible.
Frequently Asked Questions (FAQ)
1. If I don’t have any publications yet, can I still match into a competitive fellowship?
Yes, but your strategy must be focused. Start projects early in PGY2 at the latest, emphasize conference presentations, case reports, and QI that can move quickly, and lean heavily on strong clinical performance and letters. You may be less competitive for the very top programs but still a solid candidate overall, especially if your home program knows and supports you strongly.
2. How important are Step scores and ITE scores for cardiology, GI, or heme onc fellowships?
They matter most as a screening tool. Extremely low scores may raise concerns; very high scores can be a plus but won’t compensate for weak clinical performance or no specialty commitment. Fellowship PDs focus most on residency performance, letters, and specialty-specific achievements.
3. Do I need an away rotation to match into a competitive fellowship?
Not necessarily. Many applicants match without one, especially if their home institution has a strong division in that specialty. Away rotations are most helpful when your home program lacks that fellowship or when you want focused exposure at a particular external institution. If you do an away, treat it like an extended audition.
4. Should I take a research year or chief year before applying?
It depends on your goals and current profile:
- A dedicated research year can significantly strengthen applications for top-tier academic cardiology, GI, or heme onc programs, especially if you currently lack research.
- A chief year signals leadership and teaching strength and is highly respected, but adds less pure research time unless structured that way.
Discuss these options with your PD and mentors; for some, applying in PGY3 is appropriate, while for others, a delayed application yields a much stronger and more aligned match.
By approaching competitive fellowship preparation as a multi-year, strategic process—centered on clinical excellence, focused scholarship, strong mentorship, and thoughtful application planning—you greatly improve both your chances of matching and the odds that you end up in a program that truly fits your goals.






















