
Understanding the Fellowship Landscape in Emergency Medicine
Applying for fellowship after an emergency medicine residency has become increasingly common. Whether you’re interested in critical care, ultrasound, toxicology, EMS, sports medicine, or another niche, a clear fellowship application strategy can dramatically improve your chances in the fellowship match.
Unlike the EM match you navigated as a medical student, the fellowship process is more fragmented. Some fellowships use ERAS and the NRMP (or other formal match systems), while others rely on direct applications and individualized timelines. Planning ahead is essential.
Why Pursue a Fellowship in Emergency Medicine?
Common reasons EM residents pursue fellowship include:
Skill and expertise development
Subspecialty training offers deeper procedural, diagnostic, and academic skills (e.g., advanced echocardiography in ultrasound, ventilator management in critical care).Career differentiation and job market advantage
Fellowship training can open doors to leadership roles, academic appointments, and specialized clinical positions.Long-term career satisfaction
Many fellows report increased job satisfaction from having a clear niche and new career avenues (research, medical education, administration, policy).Compensation and flexibility
Some subspecialties offer improved earning potential or more controllable schedules over time, though this varies widely by region and specific niche.
Major Fellowship Pathways in Emergency Medicine
Common fellowship tracks for EM graduates include:
- Critical Care Medicine (CCM)
- Emergency Medical Services (EMS)
- Medical Toxicology
- Ultrasound / Point-of-Care Ultrasound (POCUS)
- Sports Medicine
- Palliative Care
- Research fellowships
- Medical Education fellowships
- Administration / Healthcare Leadership
- Global Health / International EM
- Pediatric Emergency Medicine (via pediatric or EM route, depending on program)
Each carries different accreditation pathways, board eligibility routes, and match mechanisms. Your strategy should be tailored to the specific field(s) you’re targeting.
Step 1: Clarify Your Fellowship Goals and Timeline
Before you think about ERAS fellowship logistics or letters of recommendation, clarify why you’re applying and what you want out of training. This will guide every other decision.
Define Your “Why”
Ask yourself:
- What gap in my current training am I trying to fill?
- Example: “I want advanced ultrasound skills to lead a hospital-wide POCUS program.”
- What do I want my practice to look like 5–10 years from now?
- Example: “50% clinical EM, 25% ultrasound education, 25% research and administration.”
- Do I need a fellowship to reach that vision?
- Some goals (e.g., becoming an ultrasound director at a large academic center) almost always require fellowship. Others (like community ED leadership) may not.
Write down your answers. These will form the backbone of your personal statement and will help you evaluate programs.
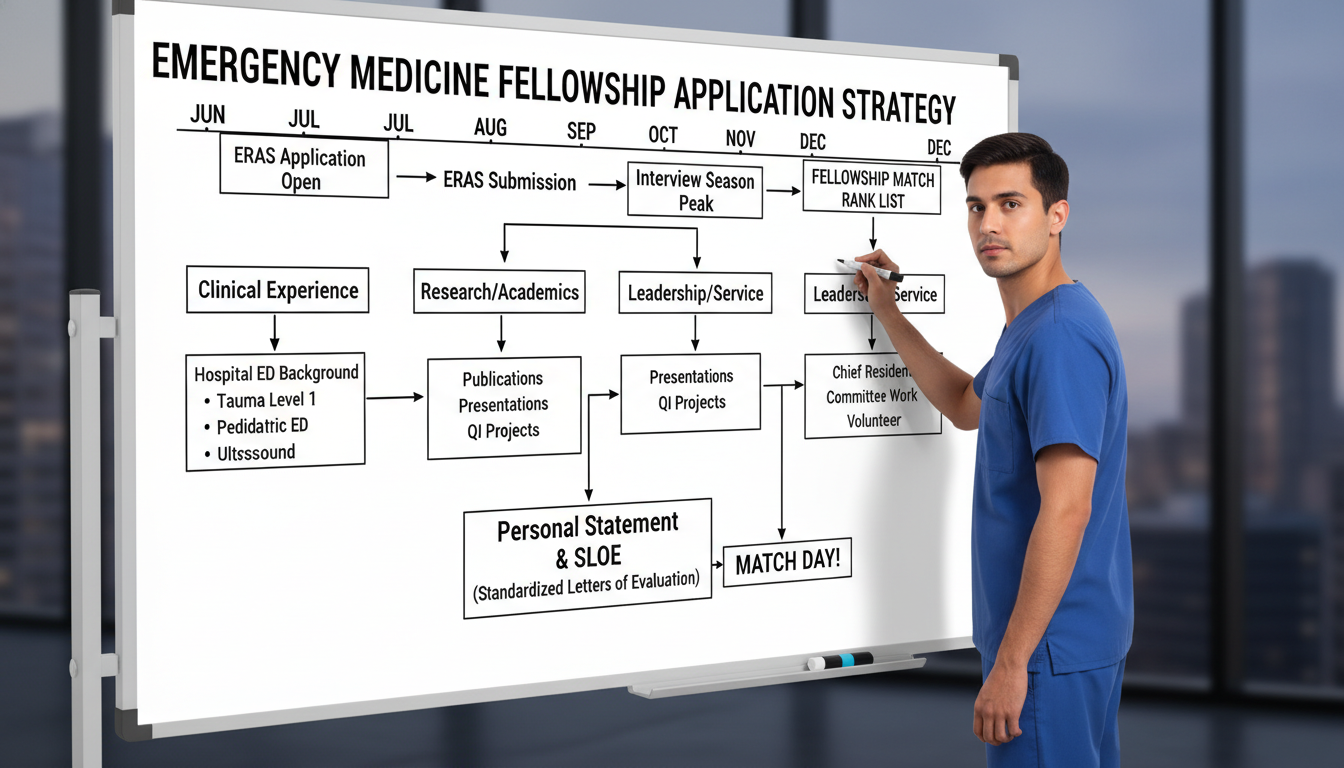
Know the Typical Timeline
Most EM residents who pursue fellowship follow one of these paths:
- Apply during PGY-3 (or PGY-4) for fellowship starting the summer after graduation.
- Apply after a year or two as attending, once career interests solidify.
For those applying during residency:
- PGY-2 (early-mid year):
- Clarify fellowship interests, begin informal mentorship conversations.
- Start building your CV toward your intended niche (research, teaching, QI projects).
- PGY-2 (late) – PGY-3 (early):
- Identify target programs.
- Request letters of recommendation.
- Begin drafting personal statement.
- PGY-3 (summer/fall):
- Submit ERAS fellowship or other applications.
- Interview season.
- PGY-3 (late fall/winter):
- Rank lists and fellowship match (depending on specialty).
Because timelines and systems differ by fellowship type and specialty board (ABEM, ABIM, ABP, etc.), verify the specific schedule for your chosen track at least 12–18 months before you plan to start fellowship.
Step 2: Map the Application Systems and Match Processes
Understanding the mechanics of the fellowship match is critical. Not all EM fellowships follow the same process.
Fellowships Using ERAS Fellowship and Formal Match Systems
Some EM-related fellowships use ERAS fellowship applications and an associated match (often through NRMP, occasionally another matching body). Examples (subject to change; always verify current details):
- Sports Medicine fellowships
- Pediatric Emergency Medicine (some programs)
- Palliative Care (as Hospice and Palliative Medicine)
- Certain Critical Care tracks (especially IM-based CCM that accept EM grads via ERAS)
Key implications:
- Standardized timeline for application, interview season, and rank list submission.
- Structured application materials similar to residency: CV, personal statement, LoRs, USMLE/COMLEX, etc.
- Fellowship match rules analogous to the EM match—binding acceptance if matched.
Fellowships Using Non-ERAS or Early Match Systems
Many EM subspecialties still rely on:
- Direct applications through program websites or email.
- Specialty-specific application portals.
- Informal or early offers outside a centralized fellowship match.
Common examples:
- Medical Toxicology
- Ultrasound / POCUS
- EMS (some use match-like processes, others don’t)
- Research, Medical Education, Administration, and Global Health (often institution-specific fellowships)
- Some Critical Care tracks (particularly anesthesia or surgery-based with EM pathways).
Implications for strategy:
- Timelines can be earlier or more variable. Some programs review applications on a rolling basis.
- Networking and mentorship play a larger role.
- You may have to navigate multiple application platforms simultaneously.
Action Steps: Building Your Logistics Plan
Create a fellowship matrix.
Build a spreadsheet with:- Program name and institution
- Fellowship type
- Application platform (ERAS fellowship vs program-specific)
- Match participation (NRMP, San Francisco Match, or none)
- Application open/close dates
- Interview window
- Contact info and special requirements
Identify critical dates early.
Backward-plan when to finalize your CV, personal statement, and letters based on the earliest deadlines.Align with your residency program.
Inform your PD and APDs early—particularly if interview travel or complex scheduling is expected. Their support can be crucial.
Step 3: Build a Fellowship-Ready Portfolio During Residency
To stand out in the fellowship match, you need more than a solid EM residency performance. You need a portfolio that matches the specific subspecialty you’re targeting.
Core Elements Every Fellowship Director Evaluates
Clinical performance and trajectory
- Strong evaluations, particularly in high-acuity settings.
- Evidence that you can function as an independent EM attending.
- Growth over time and responsiveness to feedback.
Subspecialty alignment
- Projects, electives, QI work, or leadership roles connected to your fellowship interest.
- Clear narrative of commitment to that niche, not a last-minute decision.
Academic and scholarly work
- Publications, abstracts, posters, or QI projects.
- For research-heavy fellowships, more is better; for others, 1–3 well-executed projects can suffice.
Teaching and leadership
- Chief resident roles, committee work, curriculum design, simulation teaching, etc.
- Especially important for education, administration, and global health fellowships.
Tailoring Your Activities by Fellowship Type
Below are examples of targeted strategies for common EM fellowships:
Critical Care Medicine
- Clinical:
- Maximize time in MICU, SICU, Neuro ICU, and CCU.
- Seek out advanced airway, ventilator, and hemodynamic management opportunities.
- Projects:
- ICU-based QI (sepsis bundle adherence, ventilator protocols).
- Research in resuscitation, ARDS, sepsis, or ECMO.
- Leadership:
- Design or lead code blue or RRT simulations.
- Letters:
- At least one from a critical care attending who has worked closely with you.
Ultrasound / POCUS
- Clinical:
- Take on ultrasound leadership roles within the residency (e.g., ultrasound chief).
- Aim for far above minimum scan numbers with high-quality image acquisition.
- Projects:
- POCUS-based research (diagnostic accuracy, workflow impact, education studies).
- Develop teaching sessions or curricula for medical students and junior residents.
- Leadership:
- Help maintain QA/QI of ED ultrasound.
- Letters:
- From your ultrasound director or fellowship-trained POCUS faculty.
EMS
- Clinical:
- Participate in ride-alongs, mass casualty drills, and disaster response planning.
- Projects:
- Prehospital protocol development or evaluation.
- Research in out-of-hospital cardiac arrest, trauma systems, or prehospital triage.
- Leadership:
- Work with your hospital’s EMS director or local EMS agencies.
- Letters:
- From an EMS medical director or EMS fellowship-trained faculty.
Medical Toxicology
- Clinical:
- Rotate on poison control consult services if available.
- Seek out tox consults in your ED and follow them longitudinally.
- Projects:
- Cases reports/series on interesting poisonings.
- Database reviews with poison control centers.
- Leadership/Teaching:
- Tox lectures for residents and students.
- Letters:
- From toxicologists who have directly supervised your clinical work or scholarly projects.
The same tailored thinking applies to global health, palliative care, sports medicine, and others: align your day-to-day work with your future identity.
Practical Tips to Strengthen Your Portfolio
- Start early (PGY-1 or PGY-2).
Even one project or leadership role, started early and carried through, can anchor your entire application. - Document impact.
Instead of “Participated in sepsis QI,” write:
“Led ED sepsis QI project that increased bundle compliance from 68% to 87% over 12 months.” - Seek mentorship in your specific niche.
Ideally you’ll have:- A primary mentor in your fellowship area.
- A secondary mentor for career guidance and wellness.
- Present regionally or nationally.
SAEM, ACEP, AAEM, SCCM, NAEMSP, ACMT, and other societies offer venues to present; even a poster can significantly strengthen your CV.
Step 4: Crafting a Competitive Application: CV, Personal Statement, and Letters
Once your portfolio is in place, the next step is translating it into a compelling application for the fellowship match or direct recruitment process.
Building a Fellowship-Ready CV
Your CV should:
Be clearly structured and easy to scan
Use sections: Education, Training, Certifications, Clinical Experience, Research/Scholarship, Teaching, Leadership, Service, Professional Memberships, Skills.Highlight fellowship-relevant content prominently
- Create a subsection like “Subspecialty-Focused Experience: Emergency Ultrasound” or “Critical Care Experience.”
- List key projects, roles, and outcomes.
Include metrics where possible
- “Supervised 50+ medical student shifts as senior resident.”
- “First-author publication in peer-reviewed journal (impact factor X.X).”
Be meticulously accurate
- Dates, titles, and authorship positions should be consistent with PubMed or institutional listings.
Have mentors in your chosen subspecialty review your CV and suggest field-specific enhancements.
Writing a Strong Personal Statement
Your personal statement is not a rehash of your CV; it’s the story of how and why you’re pursuing fellowship.
Structure suggestions:
Opening vignette or theme
A brief, specific clinical scenario or experience that sparked your interest (e.g., a pivotal resuscitation, an impactful prehospital case, a complex tox consult).Development of your interest
- How you explored and tested this interest during residency.
- Roles, projects, and mentorship that solidified your choice.
What you bring to the fellowship
- Skills, experiences, and personal qualities (resilience, team leadership, teaching ability).
- Concrete contributions you’ve already made (e.g., curricula, protocols, research findings).
What you are seeking from training
- Specific skills, exposure, or roles (e.g., advanced echo, health systems leadership).
- How the fellowship will bridge the gap between where you are and where you want to be.
Long-term goals
- Your 5–10 year vision and how this fellowship is a necessary step.
Tips:
- Keep it 1 page for most specialties (occasionally 1.5 pages is acceptable in more academic fellowships).
- Avoid generic statements (“I like to help people in critical times.”).
- Tailor the core statement to the fellowship type, not necessarily each individual program (unless a program allows customized statements and you have strong reasons to differentiate).
Securing Impactful Letters of Recommendation
Letters are pivotal in fellowship applications and often weigh more than in the EM match.
Aim for:
- 3–4 letters total, with:
- At least one letter from your program director (often required).
- At least one letter from a leader in your fellowship area (fellowship director, division chief).
- Additional letters from faculty who know you well clinically and academically.
Best practices:
- Ask early—at least 2–3 months before the first submission deadline.
- Schedule a brief meeting with each letter writer to:
- Discuss your career goals and target fellowships.
- Provide your updated CV and draft personal statement.
- Highlight specific projects or cases they might mention.
- Choose depth over prestige.
A detailed letter from someone who worked closely with you is better than a generic letter from a famous name who barely knows you.
When possible, aim for letters that address:
- Clinical excellence and reliability.
- Teamwork and communication.
- Response to feedback and trajectory of growth.
- Specific subspecialty-relevant strengths.

Step 5: Strategic Program Selection, Interviews, and Ranking
Even the strongest application can fall short without a thoughtful approach to choosing programs and navigating the interview and fellowship match process.
Selecting Programs Strategically
When choosing where to apply, think beyond prestige. Consider:
Training environment
- Volume and case mix.
- Balance of supervision and autonomy.
- ED- versus ICU- or field-based time (depending on fellowship).
Faculty and mentorship
- Depth and breadth of fellowship-trained faculty.
- Track record of successful graduates in roles you want.
Scholarly infrastructure
- Access to statisticians, research coordinators, simulation centers, global partnerships, etc.
- Protected time for research and conferences.
Culture and fit
- Collegiality.
- Support for wellness and reasonable schedules.
- Diversity, equity, and inclusion efforts.
Logistics
- Geographic preferences and family considerations.
- Compensation and benefits during fellowship.
- Moonlighting opportunities and whether they are allowed.
Apply broadly enough to ensure a robust set of interviews, but not so widely that you dilute your enthusiasm or ability to prepare. Many applicants target 8–15 programs, depending on competitiveness of the field and their own application strength.
Excelling in Fellowship Interviews
Common themes in fellowship interviews:
- “Why this fellowship and why now?”
- “Why our program?”
- “Tell me about a challenging case or project and what you learned.”
- “What are your long-term career goals?”
- “How do you handle conflict, feedback, or failure?”
Preparation tips:
Know your application cold.
Be ready to discuss every project and role in detail, including methodology and outcomes.Research each program.
- Key faculty interests.
- Unique program features (e.g., ECMO program, city-wide EMS oversight).
- Recent publications from the department.
Prepare thoughtful questions.
Examples:- “How do you support fellows in developing independent research projects?”
- “What types of leadership roles do graduates typically assume?”
- “How are fellows involved in teaching and curriculum development?”
Be authentic about limitations and growth areas.
Fellowship directors appreciate self-awareness and a desire to improve, as long as there’s evidence of follow-through.
Ranking Programs in the Fellowship Match (and Handling Offers Outside Match)
For fellowships participating in a formal fellowship match (e.g., NRMP, SF Match):
Rank programs by genuine preference, not speculation.
The algorithms favor applicant preference; don’t try to game the system based on where you think you’ll match.Consider long-term goals.
A program that aligns closely with your career vision may be preferable to a more “prestigious” name with a mismatched training focus.
For fellowships outside a centralized match:
- Clarify each program’s offer timeline and decision window.
- Avoid accepting an offer while still actively interviewing elsewhere unless you are truly sure; once you give your word, you should consider it binding.
- Be transparent with mentors so they can help you navigate competing offers ethically.
Step 6: Common Pitfalls and How to Avoid Them
Even strong candidates can stumble in the fellowship application process. Awareness of common errors can help you avoid them.
Pitfall 1: Late Discovery of Interest
Waiting until late PGY-3 to decide on fellowship can leave:
- Insufficient time to build a subspecialty portfolio.
- Rushed letters and personal statement.
- Missed application or fellowship match deadlines.
Prevention:
Explore early through electives, attending national conferences, and meeting subspecialty faculty in PGY-1/2.
Pitfall 2: Misaligned Narrative
Example: CV is heavily focused on ultrasound, but personal statement claims a newfound passion for critical care with minimal supporting experiences.
Prevention:
Align your “story” across CV, experiences, and statement. You can maintain secondary interests, but your primary fellowship narrative should be consistent and well-supported.
Pitfall 3: Weak or Generic Letters
Letters that merely state you are “nice and hard-working” without concrete examples do little to advance your candidacy.
Prevention:
Choose letter writers who:
- Have observed you in subspecialty-relevant settings.
- Can speak to specific competencies and growth. Provide them with data (CV, statement, project summaries) to write a rich letter.
Pitfall 4: Undervaluing Fit
Choosing a program solely for its name, location, or a single star faculty member without assessing overall fit can lead to dissatisfaction.
Prevention:
Ask current fellows candid questions about:
- Day-to-day workload and call.
- How conflicts are handled.
- Actual versus promised research and leadership opportunities.
Pitfall 5: Inadequate Communication with Residency Leadership
Surprising your PD with last-minute requests for time off, letters, or advocacy can strain relationships.
Prevention:
Loop in your PD and APDs early. Many are enthusiastic advocates and can provide inside knowledge of programs and fellowship match dynamics.
Frequently Asked Questions (FAQ)
1. Do I need a fellowship to have a successful career in emergency medicine?
No. Many EM physicians build fulfilling careers without additional training. Fellowship is most valuable when you have a clear subspecialty interest (e.g., critical care, EMS, ultrasound) that requires advanced skills or when you are targeting specific career endpoints—academic positions, leadership roles, or highly specialized practice—where fellowship training is expected or strongly preferred.
2. How many programs should I apply to for an emergency medicine fellowship?
It depends on the competitiveness of your chosen field and the strength of your application. As a general guide, many applicants apply to 8–15 programs. Very competitive fellowships or applicants with weaker portfolios may benefit from applying to more, while exceptionally strong candidates in less competitive fields may target fewer. Discuss numbers with mentors who know both you and the subspecialty well.
3. I’m interested in more than one fellowship area. Can I apply to multiple types of fellowships in the same cycle?
It’s possible, but tricky. You must ensure your CV and personal statement for each type present a coherent narrative. Applying broadly across very different fellowships (e.g., toxicology, ultrasound, and sports medicine) in the same season can dilute your message and raise concerns about commitment. If you have two closely connected interests (e.g., critical care and resuscitation research), it may be more feasible. Seek tailored advice from your mentors.
4. How different is the fellowship application process from the EM match I did for residency?
In some ways it’s similar—especially for fellowships using ERAS fellowship and a formal fellowship match (NRMP or similar). You’ll submit a centralized application, interview, and then rank programs. But overall, the fellowship ecosystem is more heterogeneous:
- Some fellowships use ERAS and the fellowship match; others rely on direct applications.
- Timelines can vary more widely.
- Letters, mentorship, and subspecialty experiences carry even more weight.
- Your personal fit with the program’s niche and faculty is often more important than in residency.
Planning early, understanding each fellowship’s specific process, and leveraging strong mentorship are the best ways to navigate these differences effectively.
By approaching the fellowship application with a deliberate strategy—clarifying your goals, aligning your experiences, understanding ERAS fellowship and non-ERAS systems, and engaging mentors—you position yourself to succeed in the fellowship match and beyond. Your ultimate aim is not just to match, but to choose a fellowship that will shape the emergency medicine career you genuinely want.






















