
Understanding Residency Work Hours in General Surgery
Managing residency work hours in general surgery is one of the most challenging aspects of training—and one of the most critical to get right. The combination of long duty hours, high-acuity patients, and steep learning curves means that how you manage your time, energy, and well-being can make the difference between thriving and just surviving.
General surgery residency remains one of the most demanding programs in terms of schedule intensity. Program structures and expectations vary, but across the board, residents must learn to balance:
- Busy clinical services
- Operative experience and call
- Academic responsibilities
- Exam preparation
- Personal life and rest
This guide breaks down how general surgery residency work hours are structured, what the duty hour rules actually mean in practice, and specific strategies you can use to protect your learning, your performance, and your health. It’s written with surgery residency match candidates, current interns, and early residents in mind.
How General Surgery Residency Work Hours Are Structured
Before you can manage your time, you need a realistic understanding of how general surgery residency is organized and what “typical” duty hours look like.
Duty Hour Regulations: What the Rules Say
In the United States, accredited residency programs must follow ACGME duty hour standards. Key elements include:
- 80-hour work week, averaged over 4 weeks
- One day off in seven, free of clinical responsibilities (also averaged over 4 weeks)
- 10 hours off between shifts recommended; at least 8 hours off required
- Maximum shift length:
- 24 hours of continuous in-house call for all residents
- Up to 4 additional hours for transitions of care and educational activities
- No more than every third night call, when averaged over 4 weeks
These rules apply to total work hours, including:
- Daytime clinical work
- Night float
- In-house call
- Home call that leads to significant clinical activity
- Required conferences, didactics, and simulation
- Charting and administrative work related to patient care
Programs are monitored for compliance, but enforcement can feel variable at the resident level. The key is to understand what’s allowed and what your options are when the reality on your service doesn’t match the written rules.
Typical General Surgery Schedules: What It Feels Like
The reality of general surgery residency work hours varies by:
- PGY level (intern vs senior resident vs chief)
- Type of rotation (trauma, ICU, transplant, vascular, acute care surgery, electives)
- Call model (night float, 24-hour traditional call, home call)
- Program type (academic university program vs community-based vs hybrid)
A common pattern in many programs looks like this:
Intern year (PGY-1)
- Early mornings (4:30–6:00 AM pre-rounds)
- Long days (often until 6–7 PM, later on busy services)
- Night float rotations: 5–6 nights/week, 12–13 hour shifts
- In-house call on trauma or acute care services
- Heavy floor work, consults, and cross-cover
Mid-level (PGY-2–3)
- Mix of ICU rotations, subspecialty services, and increased operative time
- Night float blocks or Q4–Q5 call depending on rotation
- More responsibility for consults, ED evaluations, and team coordination
Senior/Chief years (PGY-4–5)
- Heavier OR schedules
- Service leadership and teaching responsibilities
- Usually less scut work but more cognitive and decision-making load
- Still long days; “operating all day, managing service before and after”
This structure means that your residency work hours often approach the 80-hour limit, especially on high-intensity rotations like:
- Trauma/acute care surgery
- Surgical ICU
- Transplant or vascular
- Night float months
You cannot completely control the demands of these rotations. But you can control your workflow, boundaries, preparation, and recovery.
Core Principles of Managing Surgery Residency Work Hours
Instead of thinking only in terms of “hours,” it helps to think in terms of energy, efficiency, and sustainability. The residents who cope best share a few core habits.
1. Protect Your Sleep Like a Clinical Priority
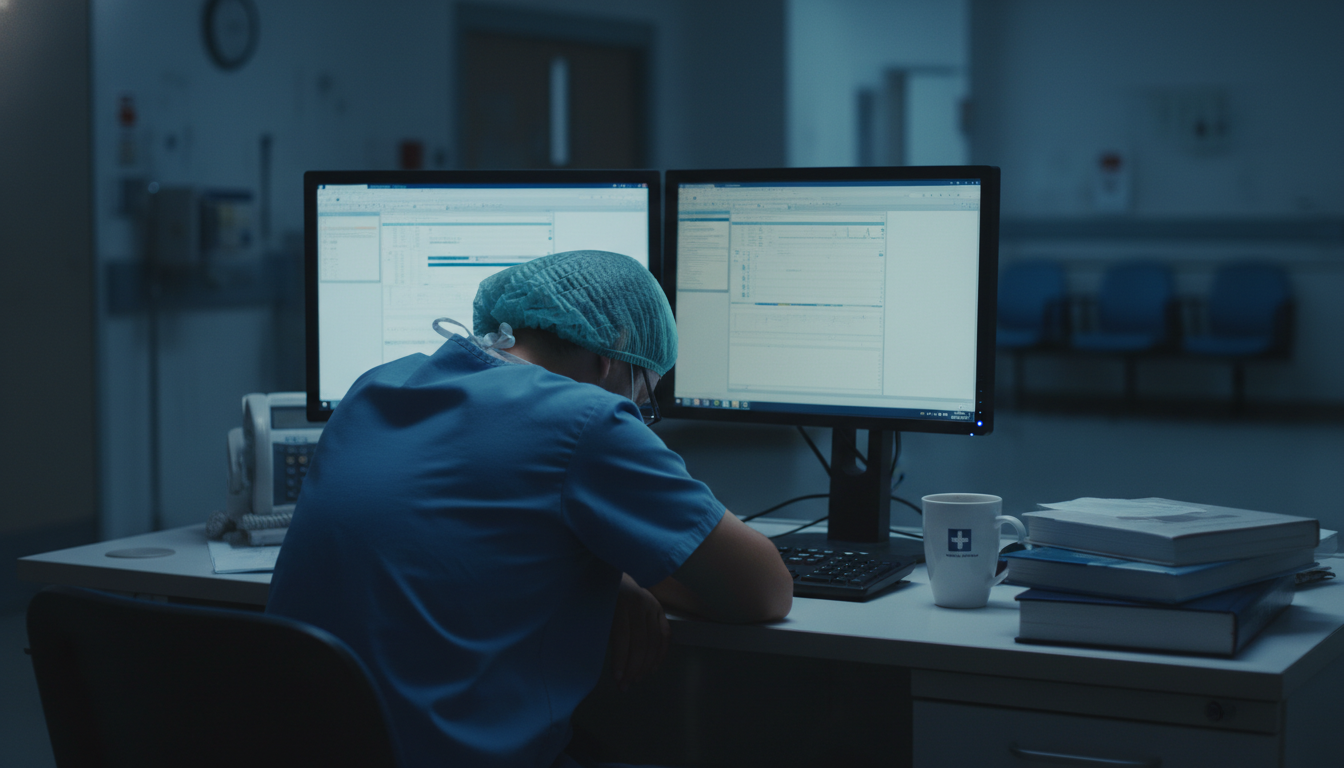
Sleep is not a luxury in general surgery residency; it’s a safety issue for you and your patients.
Evidence-based targets:
- Aim for 7–8 hours on lighter days, 5–6 on heavy days
- Use strategic naps: 20–30 minute naps before or during call if possible
- Maintain a consistent sleep anchor (a core period of sleep that’s stable across days) when night float makes full consistency impossible
Practical strategies:
Post-call rule:
When you get home post-call, go straight to bed. Don’t start laundry, don’t start a show “for 10 minutes,” don’t scroll your phone. Treat sleep like an emergency order: STAT.Sleep environment:
- Blackout curtains or eye mask
- White noise machine or fan
- Cool temperature (around 65–68°F / 18–20°C)
- Phone on “Do Not Disturb” with critical numbers on the exception list only
Transition routines:
- After nights: light breakfast, 10–15 minutes of sunlight exposure on the way home, then bed
- Before nights: short nap in the afternoon, caffeine timed early in the shift only
Residents often underestimate how fragmented, poor-quality sleep adds up to worse cognitive performance than simply having fewer hours. Small improvements make a real difference.
2. Work Smarter Within the Same Hours
You can’t remove patients from the census or stop traumas from rolling in, but you can meaningfully reduce wasted time and duplication of effort.
Think in terms of systems, not just effort.
Examples of systems-level time savers:
Batching tasks:
- Complete all orders for one patient while you’re in their chart
- Return non-urgent pages in clusters every 20–30 minutes rather than one at a time
- Consolidate calls to consulting services—know what you want, and call once
Standardizing workflows:
- Use templates for progress notes, consult notes, and discharge summaries
- Create checklists for common scenarios (post-op orders, pre-op orders, transfers to ICU)
- Keep a personal “smart phrase library” in your EMR
Optimizing rounds:
- Pre-round with a clear data checklist (vitals, labs, I/Os, imaging, drains)
- Identify “discharge candidates” before attending rounds and pre-write orders
- Clarify each patient’s plan as “today’s goal(s)” so you can execute efficiently
The more predictable you make your routine tasks, the more mental bandwidth you have for critical decisions and operative learning.
3. Align Your Effort With Learning, Not Just Survival
During intense rotations, it’s easy to slip into pure survival mode: just make it to sign-out, just make it to the weekend. But general surgery residency is finite; you’re building skills every day.
Use your limited time and energy to maximize high-yield learning moments:
- Prioritize being present in the OR and procedures when safe and possible
- Delegate and redistribute low-yield tasks when your presence elsewhere would mean significant learning (e.g., ask if the intern can manage dressing changes while you scrub)
- When possible, protect at least one focused reading block per day (even 20–30 minutes) linked to a current patient or operation you saw
The synergy between clinical exposure + focused reading is far more powerful than adding another hour of unfocused, exhausted study.

Day-to-Day Tactics to Manage Long Duty Hours
Translating principles into daily habits is where your quality of life really shifts. Below are concrete strategies, tailored to common general surgery rotations and scenarios.
Managing Busy Day Shifts
On heavy services, the volume of pages, orders, and tasks can feel endless. Control what you can by structuring your day tightly.
1. Morning routine (pre-rounds + data capture)
- Log in and print/refresh your patient list immediately
- For each patient, quickly gather:
- Vitals and trends
- Overnight events from nursing and overnight team sign-out
- Labs/imaging
- I/Os, drain outputs, NG tube output
- Jot down “problem-focused” bullets rather than re-writing the whole history. For example:
- “POD#2 lap sigmoid; pain controlled; tolerating clears; needs ambulation x3 + IS coaching; possible DC tmw if tolerating diet.”
A well-prepared list shortens rounds and reduces backtracking all day.
2. Rounds: drive clarity and next actions
During rounds, aim to leave each room with clarity on:
- Today’s primary goal(s)
- Pending tasks
- Ownership (who is doing what)
- Anticipated disposition (home vs rehab vs TICU, etc.)
Immediately after rounds, batch your order entry. Focus first on:
- Time-sensitive orders (stat labs, imaging, consults)
- Discharge planning tasks
- Pain and nausea control
3. Midday: protect at least one focused block
Even on chaotic days, look for:
- A 10–15 minute block to return all non-urgent pages and consolidate decisions
- A 20–30 minute window (during lunch or a lull) to:
- Skim a chapter related to your most complex OR case or ICU patient
- Review one procedure video for tomorrow’s case
- Work on a small chunk of research or QI if your rotation allows
If you treat every small gap as only “scroll time,” the day will feel like pure depletion instead of training.
4. Handoffs and sign-out
Effective sign-out protects your patients and your sleep.
- Use a structured handoff tool (e.g., I-PASS)
- Flag:
- Sickest patients and “what could go wrong tonight”
- Pending labs/imaging and expected actions
- Patients at risk for deterioration (borderline vital signs, active bleeding, early sepsis)
High-quality sign-out reduces overnight calls and avoids unnecessary “check-ins” from anxious cross-cover.
Surviving and Learning on Night Float
Night float is physically and mentally taxing, but it can be an excellent time to build decision-making skills.
1. Before the block starts:
- Adjust your sleep gradually over 2–3 days if possible (later nights, later wake-ups)
- Meal prep or arrange simple, healthy food options
- Communicate with important people in your life about your “off-hours” during the block
2. During the block:
- Use a task board or running list for admissions, cross-cover, and consults
- Triage ruthlessly:
- True emergencies and unstable patients first
- Then pain control, fevers, active bleeding, new abdominal pain, etc.
- Whenever safe, cluster bedside checks to minimize repeated trips to the same area
3. Learning on nights:
- For each admission or urgent consult, commit to learning one high-yield teaching point:
- Ex: for SBO admission, read for 10 min about operative vs non-operative indications
- For GI bleed consult, review transfusion thresholds and initial resuscitation
- If there’s a pause after a big case or trauma, ask the attending or senior:
- “What was the main decision point in that case?”
- “What should I read about this before tomorrow?”
4. Protecting your off-time:
- Avoid long daytime commitments (social or academic) on a night float block
- Anchor a core 4–5 hour sleep period you protect aggressively, then add naps around it
- Use blue-light-blocking settings or glasses on your commute home to help with sleep onset
Call Days and 24-Hour Shifts
On traditional call rotations (trauma, acute care surgery), you may have 24-hour (or 24+4) in-house calls.
Planning a call day:
Pre-call:
- Arrive early, ensure your day list is organized before call ramps up
- Eat a solid meal and bring snacks that are easy to grab (nuts, protein bars, fruit)
- Identify high-risk patients you want to personally check before night
During call:
- Triage consults and ED cases in collaboration with your senior
- Use mental or written algorithms for common emergencies (appendicitis, cholecystitis, SBO, GI bleed, trauma activations)
- When possible, power nap in 15–20 minute segments during quieter stretches
Post-call:
- Sign out thoroughly, emphasizing overnight changes and pending items
- Leave the hospital as soon as you are safely able and permitted—do not linger
- At home, hydrate, eat something small, and go straight to sleep
Maintaining Resident Work–Life Balance in a Demanding Specialty
“Resident work life balance” in general surgery will never mean a 9-to-5 schedule. But it also doesn’t have to mean complete personal sacrifice. The goal is sustainable integration, not perfection.
Setting Realistic Expectations
You will have:
- Rotations where you feel almost balanced and human
- Rotations where work dominates nearly everything else
Balance is best measured over months, not days. During a trauma month, it may look like:
- Sleeping whenever you’re not at work
- Minimal social life
- Very intentional time with one or two close people on your day off
- Short, efficient workouts rather than long gym sessions
During lighter rotations, you can rebalance:
- More exercise
- More time with family and friends
- Progress on research or hobbies
Accepting the cyclical nature of balance can reduce guilt and frustration.
Protecting Your Non-Negotiables
Even in general surgery, you can usually protect a few core “non-negotiables” if you define them clearly and communicate appropriately.
Examples:
- 2–3 short exercise sessions per week (20–30 min runs or bodyweight workouts)
- Weekly connection with a key family member or partner (in person or video)
- A standing therapy, coaching, or mentorship session when the schedule allows
Tips:
- Use your calendar aggressively—schedule your priorities, don’t just “fit them in”
- Be honest with important people:
- “On my ICU month, I will likely only be available on Sunday mornings. After that, things ease up.”
- On your day off, decide consciously:
- “Today is recovery-focused” vs “Today I want to be social/active”
Mixing too many expectations into one day off can leave you more exhausted.
- “Today is recovery-focused” vs “Today I want to be social/active”
Mental Health and Burnout Prevention
General surgery residency carries a real risk of burnout, depression, and anxiety. Managing duty hours isn’t just about fatigue; it’s about psychological safety and resilience.
Warning signs you should not ignore:
- Persistent thoughts of quitting or feeling trapped
- Loss of interest in surgery or anything outside of work
- Increasing cynicism, irritability, or emotional numbing
- Reliance on alcohol or substances to cope or sleep
- Thoughts of self-harm or that others would be better off without you
If these appear:
- Contact your program’s confidential counseling services or employee assistance program
- Reach out to a trusted faculty mentor or chief who is known to be supportive
- Use external resources (national helplines, therapy outside the institution) if internal options feel unsafe or political
Using support is not a sign of weakness; it’s a professional step to protect your career and your patients.
Navigating Duty Hour Violations and Program Culture
Even with regulations, resident experiences vary widely based on program culture and how seriously leadership takes work hours and wellness.
Recognizing Patterns vs One-Off Bad Weeks
Individual heavy weeks happen in general surgery—massive traumas, staff shortages, unexpected service surges. Distinguish these from systemic issues:
Red flags suggesting a systemic duty hour problem:
- Routinely averaging >80 hours/week over multiple months
- Never getting a true 24-hour period off in 7 days
- Regularly staying >4 hours beyond call end for non-educational reasons
- Pressure (implicit or explicit) to under-report hours
If this is truly the culture, it affects not just your comfort but your safety and education.
What You Can Do as a Resident
Steps to consider, escalating as needed:
- Track your hours honestly for yourself first, even if your reporting system feels flawed.
- Talk to your immediate senior/chief:
- Frame concerns around patient safety and compliance, not just personal comfort.
- Example: “We’ve been averaging 90 hours the last 3 weeks and not getting days off. I’m concerned about our ability to safely care for these patients.”
- Approach your program leadership or chief residents with specific data, not vague complaints.
- Use anonymous reporting mechanisms (GME office, ACGME surveys) if internal feedback is ineffective or retaliatory behavior appears.
Residency programs are obligated to remain compliant. Repeated, documented duty hour violations are taken seriously by accrediting bodies.
Evaluating Programs Before the Match
For medical students planning the surgery residency match, work hour culture should be a core selection factor.
During interviews and second looks, ask:
- “On your heaviest rotation, what does a typical week look like—start and end times included?”
- “How often are people actually at 80 hours, and how often under?”
- “Do residents feel comfortable reporting true hours without fallout?”
- “What is post-call really like here?”
Pay close attention to:
- How consistently residents answer
- Body language—do they hesitate, joke nervously, or look at each other before answering?
- Differences between intern and senior responses
Programs that talk openly about protecting duty hours and resident work life balance are more likely to be sustainable environments.
FAQs: Managing General Surgery Residency Work Hours
1. Are 80-hour weeks really typical in general surgery residency?
On many high-acuity services, yes—general surgery residency often pushes close to the 80-hour limit, especially early on. Some rotations may average 70–75 hours; others may hit the 80-hour cap consistently. The key is that over a 4-week period you should not consistently exceed 80 hours and should be getting at least one day off in seven on average.
2. How can I study for ABSITE with such long duty hours?
Link your studying directly to your clinical work:
- Read 10–20 minutes daily about the operations or pathologies you saw that day.
- Use question banks during short breaks rather than long, unfocused sessions.
- On lighter rotations or vacation, plan focused ABSITE blocks (2–3 hours at a time).
Consistency matters more than marathon sessions; even 30 focused minutes a day adds up over months.
3. Is it possible to have a family or relationship and still do a general surgery residency?
Yes, but it requires planning, flexibility, and honest communication. Many residents successfully have partners, children, or caregiving responsibilities. Strategies include:
- Aligning expectations with your partner about your availability on different rotations
- Using days off very intentionally for quality time
- Leveraging support systems (family, childcare, friends) and being willing to ask for help
The idea that you “can’t have a life” in general surgery is outdated—challenging, yes; impossible, no.
4. What should I do if my program pressures residents to under-report work hours?
This is a serious professionalism and accreditation issue. Steps you can take:
- Document your actual hours privately.
- Talk with trusted senior residents or faculty mentors to understand whether others share your concerns.
- Use formal and anonymous reporting pathways (GME office, institutional compliance, ACGME resident survey).
Your safety and patient safety come first. Programs are required to foster a culture where trainees can report concerns without retaliation.
Managing residency work hours in general surgery is less about escaping long days and more about creating sustainable patterns—protecting sleep, working efficiently, maximizing learning, and defending the boundaries that keep you healthy. With deliberate strategies and a supportive program culture, you can not only endure the workload but grow into the surgeon you set out to become.






















