
Understanding Combined vs Categorical Programs
Choosing between combined and categorical residency programs is one of the most strategic decisions you’ll make as you approach the Match. It affects everything from your day-to-day training to your board eligibility, fellowship options, lifestyle, and ultimately your career identity.
This guide breaks down the differences step-by-step, with a particular focus on internal medicine–pediatrics (med peds programs) and other popular combined pathways, and how to decide which structure fits your goals.
Basic Definitions
Categorical residency programs
- Traditional, single-specialty training
- Leads to board eligibility in one ACGME-accredited specialty
- Examples:
- Internal Medicine (3 years)
- Pediatrics (3 years)
- General Surgery (5 years)
- Emergency Medicine (3–4 years)
- You enter as a PGY-1 and remain in the same department until graduation
Combined residency programs
- Intentionally structured to train you in two distinct specialties over a slightly longer period than a single categorical residency
- Integrated from day one
- Designed to meet all ACGME and board requirements for both specialties
- Examples:
- Internal Medicine–Pediatrics (Med-Peds) – 4 years
- Internal Medicine–Psychiatry – 5 years
- Family Medicine–Psychiatry – 5 years
- Pediatrics–Psychiatry–Child & Adolescent Psychiatry (Triple Board) – 5 years
In short: categorical vs combined is about one core specialty vs a dual (or more rarely, triple) specialty pathway with a coordinated curriculum.
Types of Combined Residency Programs
Not all “combined” experiences are the same. It helps to separate formally accredited combined programs from other multi-specialty training paths.
1. Med-Peds Programs (Internal Medicine–Pediatrics)
The most common combined residency is the med peds program, recognized by both the American Board of Internal Medicine (ABIM) and the American Board of Pediatrics (ABP).
Key characteristics:
- Length: 4 years
- Board eligibility: Internal Medicine and Pediatrics
- Training structure:
- Roughly 50% adult medicine, 50% pediatrics
- Frequent switching between departments—often every 3–4 months
- Continuity clinics in both IM and Peds across all four years
- Career paths:
- Primary care across the lifespan
- Hospitalist work (adult, pediatric, or both depending on setting)
- Subspecialty fellowship in either medicine or pediatrics (e.g., cardiology, GI, ID)
- Med-peds focused academic, global health, or transitional care roles
Med-peds is a true combined residency, with a unified curriculum and a clearly defined identity. It is not just “doing both” an IM and Peds residency separately.
2. Other Formal Combined Programs
Several other combined programs are jointly approved by respective boards and have standardized curricula:
Internal Medicine–Psychiatry (IM-Psych)
- 5 years
- Board eligibility in both Internal Medicine and Psychiatry
- Good for those interested in integrated behavioral and medical care, consult-liaison, addiction, or complex chronic disease
Family Medicine–Psychiatry
- 5 years
- Emphasis on primary care + mental health
- Often used for community psychiatry, rural practice, or integrated behavioral health systems
Pediatrics–Psychiatry–Child & Adolescent Psychiatry (Triple Board)
- 5 years
- Board eligibility:
- Pediatrics
- General Psychiatry
- Child & Adolescent Psychiatry
- Designed for complex developmental, behavioral, and psychiatric conditions in children
All of these are integrated combined residencies, not sequential degrees. They differ from categorical vs combined simply in how many specialties and how long.
3. Sequential Dual Training (Not True “Combined”)
Some trainees pursue two specialties back-to-back, for example:
3-year Categorical Internal Medicine → 3-year Categorical Pediatrics
(Total: 6 years, not structured as med-peds)3-year Categorical Family Medicine → 4-year Psychiatry
(Total: 7 years)
This is not the same as a combined program:
- Longer total training time
- No integrated curriculum
- You are typically completing one categorical residency and then another
Sequential dual training is uncommon due to time and opportunity cost, but it’s an option for very specific career goals or late changes in direction.
Comparing Categorical vs Combined Training
When deciding between categorical vs combined programs, think in terms of structure, identity, time, and flexibility.
1. Training Structure and Curriculum
Categorical programs:
- You live almost entirely in one department (e.g., Internal Medicine)
- Rotations are all within that specialty, with occasional electives in related fields
- Continuity clinic is focused on one patient population (adult or pediatric)
- Educational conferences, mentors, and colleagues are all centered in one discipline
Combined programs:
- Intentionally alternate between two departments
- Med peds example:
- 4 years split between Internal Medicine and Pediatrics
- Often 3–4 month blocks alternating between departments
- Dual continuity clinics (adult and pediatric) throughout
- Educational conferences in both departments
- Two sets of mentors, chiefs, and program leadership
Implications for you:
- If you like depth and immersion in one field, categorical may feel more comfortable.
- If you enjoy variety, switching contexts, and building a broad skill set, a combined program may be more satisfying.
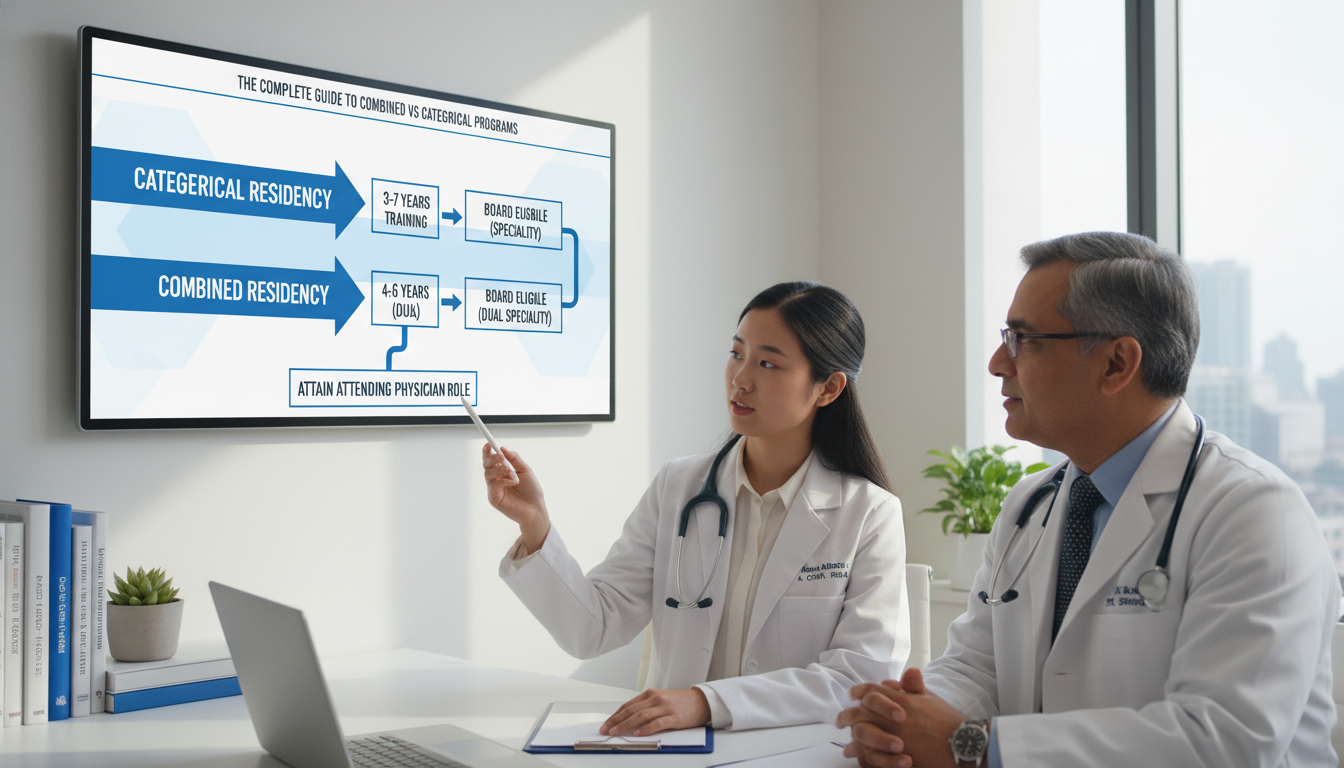
2. Length of Training and Board Eligibility
Categorical vs combined: Time to completion
- Categorical IM or Peds: 3 years
- Med-Peds: 4 years (only 1 additional year to be board-eligible in both)
- IM–Psych or FM–Psych: 5 years
- Triple Board: 5 years
Combined programs are more time-efficient than doing two full categorical residencies sequentially. With med peds, for example, you earn dual board eligibility in 4 years vs 3 + 3 = 6 years if done separately.
3. Career Identity and Day-to-Day Practice
This is often the deciding factor.
Categorical residency graduates:
- Typically develop a clear, focused professional identity:
- “I’m an internist”
- “I’m a pediatrician”
- “I’m a psychiatrist”
- Most practice within a single patient population
- Fellowship options and job searches are streamlined and specialty-specific
Combined residency graduates:
- Carry dual identities:
- “I’m med-peds trained” (internist + pediatrician)
- “I’m an internist and psychiatrist”
- Clinical practice patterns vary:
- Some split time between adult and pediatric care
- Some primarily practice in one of their specialties but use the dual background for complex patients, systems roles, or niche positions
- Unique opportunities:
- Transitional care (adolescents with chronic childhood diseases entering adult care)
- Complex comorbid patients (e.g., medical–psychiatric overlap)
- Community or rural settings wanting broad coverage
Reflect on this question:
Do you envision yourself wanting to be “an expert in one area” or “a bridge between two worlds”?
Your honest answer guides categorical vs combined decisions better than any checklist.
4. Flexibility, Fellowship, and Long-term Options
Fellowship training from categorical vs combined
- Combined programs like med peds allow you to pursue fellowship in either home specialty, as long as you meet that specialty’s board and training requirements.
- Med peds → cardiology, GI, heme/onc, ID, etc. (adult or pediatric)
- IM–Psych → consult-liaison psychiatry, addiction medicine, etc.
- You typically cannot enter a dual-specialty fellowship (there are very few combined fellowships), so you’ll choose one direction at that stage.
Job market considerations
- Categorical graduates:
- Straightforward alignment with traditional positions (e.g., hospitalist, outpatient clinic, subspecialty group)
- Combined graduates:
- Eligible for most of the same jobs as categorical peers in either specialty
- Plus:
- Hybrid roles (e.g., 60% adult hospitalist, 40% pediatric hospitalist)
- Complex care clinics
- Leadership positions in systems that value integrated care (e.g., behavioral + primary care, lifespan chronic disease programs)
Flexibility trade-off:
- A combined pathway broadens potential roles but may make your story more complex:
- You’ll need to be ready to explain to employers how you want to use both aspects of your training.
- A categorical pathway typically yields a simpler, more linear narrative.
Advantages and Disadvantages of Combined Programs
Looking specifically at combined residencies (especially med peds programs), several patterns emerge.
Advantages of Combined Residency Training
- Dual Board Eligibility with Minimal Extra Time
- Med peds: 4 years vs 6 years if separately
- IM–Psych/FM–Psych: 5 years vs 7 if done sequentially
- This is a major advantage if you truly want competence and recognition in both fields.
- Breadth of Clinical Skill
- You become comfortable managing:
- Neonates to geriatric patients (med peds)
- Complex medical illness with co-occurring psychiatric disorders (IM–Psych, FM–Psych)
- Employers often appreciate this versatility, especially in:
- Rural or resource-limited settings
- Academic or tertiary centers with complex patient populations
- Systems trying to build integrated care models
- Unique Niche Opportunities
Examples for med peds:
- Transition clinics for patients with childhood-onset conditions (e.g., cystic fibrosis, congenital heart disease, sickle cell, diabetes)
- Combined adult-pediatric hospitalist roles
- Global health positions where you’re expected to care for all ages
Examples for IM–Psych or FM–Psych:
- Integrated behavioral health clinics
- Collaborative care programs
- Leadership in psychiatric units embedded in general hospitals
- Intellectual Variety
- Many combined residents thrive on the constant challenge of shifting contexts:
- One month: adult MICU
- Next month: pediatric wards
- This can stave off burnout for those who crave diversity in their practice.
Disadvantages and Challenges of Combined Programs
- Longer Training vs a Single Categorical
- You must accept at least one additional year compared to a standard 3-year categorical IM or Peds residency.
- Financial and personal implications:
- One extra year of resident salary instead of attending pay
- Delayed loan repayment at a higher income level
- Impact on partner, family plans, or geographic stability
- Less Depth in Each Field? (Perception vs Reality)
- Some worry combined trainees are “jacks of all trades, masters of none.”
- In reality, combined curricula are carefully structured to meet full board requirements in both specialties.
- However:
- Your time in each department is split, so:
- Fewer consecutive months on one service
- Relationships and reputation in each department may build a bit more slowly
- Your time in each department is split, so:
- You must be pro-active to ensure robust mentorship and case volume in your areas of interest.
- Identity Complexity and Decision Fatigue
- During and after training, you may feel pulled between two fields:
- Should I focus my career on adults or children?
- Do I identify more as a psychiatrist or internist?
- Many combined residents say this is a feature, not a bug, but it does require repeated reflection and career conversations.
- Scheduling and Administrative Complexity
- Two sets of:
- Program directors
- Chiefs
- Evaluation systems
- You must:
- Track requirements for both boards
- Attend two different sets of conferences (often with some flexibility)
- Navigate block switches between departments, which can be stressful
Advantages of Categorical Programs
- Shorter Time to Independent Practice (in 3-year fields)
- Internal Medicine, Pediatrics, Family Medicine, Psychiatry can be completed in 3–4 years.
- You become a fully trained attending sooner, with higher income and flexibility.
- Focused Identity and Mentorship
- One department, one primary program director
- Easier to:
- Build a reputation
- Get leadership opportunities (chief resident, QI lead)
- Find mentors aligned with highly specialized goals
- Simpler Lifestyle and Logistics
- No constant transitioning across departments
- A single educational culture and administrative system

How to Decide: Practical Steps for Applicants
The choice between combined vs categorical programs should be driven by who you are, not just abstract pros and cons. Here’s a structured way to approach it.
Step 1: Clarify What You Want to Do Clinically
Ask yourself:
- Do I truly want to regularly care for two distinct patient populations or domains (e.g., adults and kids, medical and psychiatric)?
- Can I see myself:
- Splitting clinic sessions across specialties?
- Working in a setting that explicitly needs dual-trained physicians?
- If I had to choose one population forever:
- Which would it be?
- How strongly do I feel about that?
If you feel strongly called to just one domain (e.g., “I only love adult medicine”), a categorical program is likely the better fit.
If you repeatedly find yourself unable to choose because you love caring for multiple groups and integrating perspectives, a combined residency may be worth serious consideration.
Step 2: Consider Your Tolerance for Complexity and Change
Combined programs reward people who:
- Enjoy frequent changes in environment and team
- Adapt quickly to new systems and workflows
- Can manage slightly more complex schedules and requirements
If you know that constant switching drains you or disrupts your learning, a categorical setting may be more conducive to your success.
Step 3: Explore Programs Early and Honestly
Use your clinical years and application season strategically:
- During core rotations:
- Notice where you feel “at home”:
- Adult wards vs pediatric floors
- Outpatient vs inpatient
- Medical vs psychiatric
- Notice where you feel “at home”:
- Schedule electives that test combined interests:
- Med-peds clinics
- Consult-liaison psychiatry
- Transition-of-care clinics
- Integrated behavioral health
On the interview trail:
- Apply to both categorical and combined programs if you’re undecided.
- Ask combined residents:
- What made you choose combined?
- What do you see as the biggest trade-offs?
- How did your interests evolve during training?
- Ask categorical residents:
- Do you know colleagues who started combined and switched, or vice versa?
- How do faculty view combined-trained colleagues here?
Step 4: Understand Application Logistics
For most ACGME-accredited combined residencies:
- They have separate NRMP codes from categorical programs.
- Med peds programs are listed under internal medicine but clearly labeled as “Medicine-Pediatrics.”
- IM–Psych and FM–Psych are usually listed under one of the parent specialties.
Strategic tips:
- Tailor your personal statement:
- You can write a combined-focused personal statement and a more categorical-focused one, then assign them appropriately in ERAS.
- Letters of recommendation:
- For med peds:
- At least one letter from internal medicine and one from pediatrics (if possible)
- For psych-combined:
- Letters from both primary care/IM/FM and psychiatry helpful
- For med peds:
- Ranking strategy:
- Decide how you’ll prioritize combined vs categorical on your rank list before last-minute stress sets in.
- Some applicants rank combined programs first, followed by categorical “backup” options in their preferred single specialty.
Step 5: Visualize Your Future Self
Picture yourself 10 years from now:
- Where are you working?
- Academic center, community hospital, private practice, global health setting?
- Who are your patients?
- Only adults? Only children? A mix?
- Medically complex? Psychiatrically complex?
- What do you want to say when someone asks, “What kind of doctor are you?”
If the most satisfying answer in your mind is something like:
- “I’m a med-peds doc who runs a transition clinic for young adults with congenital heart disease,”
then a med peds program may be the right call.
If you immediately think:
- “I’m a cardiologist working in a high-volume tertiary center,”
then a clear categorical internal medicine route with cardiology fellowship may be more direct—though med peds can also get you there if you still want the pediatric foundation.
Common Pitfalls and How to Avoid Them
Pitfall 1: Choosing Combined as a “Hedge”
Some applicants choose combined residency because they feel:
- “I can’t decide, so I’ll just get trained in everything.”
This can backfire if:
- You don’t actually enjoy the daily reality of both specialties
- You feel resentful of the extra training time
- You never develop a satisfying narrative of how you’re using your dual skills
Solution: Only choose a combined program if you have a positive reason to do so—not just fear of missing out.
Pitfall 2: Underestimating the Lifestyle and Emotional Load
Combined residents often:
- Manage more transitions (new teams, new expectations)
- Spend energy on maintaining competence in two knowledge domains
Solution:
- Talk to current combined residents about burnout and coping strategies.
- Assess your support system and resilience honestly.
Pitfall 3: Overlooking Categorical Excellence
Some of the best training for complex populations still happens in categorical programs that are very strong in:
- Medically complex children (tertiary pediatrics centers)
- Co-morbid psychiatric and medical illness (high-volume psychiatric hospitals with robust consultation services)
- Transitional care (adult medicine programs with specialized clinics)
Solution:
- Evaluate specific programs, not just training structures.
- Ask: “Can I achieve my career goals with a strong categorical program plus targeted electives, or do I truly need dual residency training?”
FAQs: Combined vs Categorical Residency Programs
1. Is it harder to match into combined programs like med peds than categorical programs?
It depends on the specialty and institution. Med peds programs are relatively small in number and class size, so individual spots can feel competitive. However, the applicant pool is also smaller and more self-selected. In many hospitals, categorical internal medicine spots outnumber med peds positions by a large margin. Strong applicants with clearly articulated interest in combined training generally match well. It’s wise to apply to a mix of combined and categorical programs if you’re uncertain.
2. Can I still do a fellowship after a combined residency?
Yes. Graduates of combined programs like med peds are eligible for fellowships in either of their parent specialties as long as they meet board and ACGME requirements. For example, med peds graduates routinely match into adult cardiology, adult or pediatric infectious disease, pediatric endocrinology, etc. You will typically pursue fellowship in one of the fields, not both simultaneously, though your dual background often becomes an asset within that fellowship.
3. Do combined residents get paid differently than categorical residents?
No. Resident salary is usually determined by PGY level, not by program type. A PGY-1 med peds resident and a PGY-1 categorical internal medicine resident at the same institution receive the same pay. The financial difference comes from the additional year(s) of training—meaning you spend extra time at resident salary instead of attending-level income.
4. Can I switch from combined to categorical (or vice versa) once I start?
Switching from combined to categorical (e.g., from med peds to categorical pediatrics) is more common and often feasible, especially early in training, because many of your rotations count toward the categorical requirements. Switching from categorical to combined can be more complicated and depends on program capacity, timing, and board requirements. Any switch requires careful coordination with program leadership and the relevant boards, and it is never guaranteed—so you should enter residency with the assumption that you’ll complete the track you start.
Choosing between categorical vs combined residency programs is ultimately about aligning the structure of your training with the physician you want to become. If you invest time in self-reflection, honest conversations with mentors, and careful exploration of programs, you’ll be able to make a deliberate choice that supports both your professional growth and your long-term satisfaction.






















