Understanding Step 2 CK in the Context of Emergency Medicine for IMGs
For an international medical graduate, Step 2 CK is often the pivotal exam that determines competitiveness for an emergency medicine residency. Unlike Step 1, which emphasizes basic sciences, Step 2 CK is a clinical knowledge exam that assesses how you think and act like a clinician—exactly what program directors in emergency medicine (EM) care about.
Why Step 2 CK Matters So Much for EM and IMGs
- Programs are exam-score sensitive. Many EM programs use Step 2 CK scores as an initial screening filter. A strong Step 2 CK score can significantly improve your EM match prospects, especially if Step 1 is pass/fail or weaker than you hoped.
- Clinical decision-making is central to EM. Step 2 CK aligns closely with patient care priorities in the ED—stabilization, triage, immediate life-saving interventions, and risk stratification.
- IMGs often rely more heavily on metrics. As an international medical graduate, you may have less familiarity with the U.S. system and fewer U.S. clinical experiences. A strong Step 2 CK score can help compensate for these gaps and demonstrate that you can safely and effectively care for acutely ill patients.
How Step 2 CK Blueprint Aligns With EM
While Step 2 CK covers all major specialties, several domains are especially high-yield for future emergency physicians:
- Internal Medicine and Cardiovascular disease – chest pain, heart failure, arrhythmias, ACS management
- Pulmonary and Critical Care – respiratory failure, asthma/COPD exacerbations, pulmonary embolism
- Trauma and Surgery – trauma protocols, acute abdomen, postoperative complications
- Neurology – stroke, seizures, altered mental status, meningitis/encephalitis
- Obstetrics and Gynecology Emergencies – ectopic pregnancy, preeclampsia, postpartum hemorrhage
- Pediatrics – pediatric sepsis, bronchiolitis, dehydration, congenital heart disease
- Psychiatry and Toxicology – agitation, overdose, withdrawal, suicidal patients
For EM residency ambitions, these are not just test topics—they mirror what you will see on your first day in the emergency department.
Building a Strategic Step 2 CK Study Plan as an IMG
Creating a structured, realistic USMLE Step 2 study plan is your foundation. As an IMG, you may be juggling visa issues, financial constraints, and varying levels of clinical activity, so intentional planning is critical.
Step 1: Define Your Timeline and Target Score
For an EM match, many applicants aim for a Step 2 CK score at or above the national mean, and ideally higher if you are an IMG without extensive U.S. clinical experience.
- Competitive target for EM IMGs: Often > 245 is considered strong, but context matters (research, USCE, SLOEs, etc.).
- Minimal acceptable range: Programs differ, but many will use a cutoff in the 220–230+ range; IMGs are often expected to be at or above this.
Timeline examples:
- If you are 6 months out:
- 4 months of part-time prep alongside clinical/other commitments
- 2 months of more intensive, exam-focused study
- If you are 3–4 months out (common for IMGs between rotations or jobs):
- 3 months of high-yield, question-heavy preparation
- Final 2–3 weeks focused on refinement and full-length practice exams
Step 2: Assess Your Baseline
Before you design a detailed USMLE Step 2 study schedule, you need to know where you’re starting from.
- Take a baseline self-assessment: NBME or UWorld self-assessment if you’re within 3–6 months of test day.
- Review:
- Overall score prediction vs. target Step 2 CK score
- Subject breakdown (e.g., internal medicine vs. OBGYN vs. psychiatry)
- Systems breakdown (cardio, neuro, GI, etc.)
- If your baseline is >10–15 points below your target, you’ll need a more intensive, longer preparation window.
Step 3: Allocate Study Time by Weakness and EM Relevance
Not every subject is equally important if you’re targeting emergency medicine. While you must master all tested content, give extra time and emphasis to:
- Cardiology, Pulmonology, Neurology
- Critical care topics and shock
- Infectious diseases (especially sepsis, meningitis, pneumonia)
- OB emergencies and pediatrics (commonly underemphasized by IMGs)
- Trauma, orthopedics, and acute surgical abdomen
- Toxicology and psychiatric emergencies
Design your weekly schedule as a mix of:
- 60–70% Question-based learning (Qbank blocks + thorough review)
- 20–30% Focused content review (videos, notes, or concise textbooks)
- 10–20% Self-assessment and strategy refinement
Step 4: Example 12-Week Study Plan for an IMG Targeting EM
This is an illustrative framework; adjust according to your baseline and obligations.
Weeks 1–4: Foundation and Familiarization
- 20–40 questions/day on weekdays; 40–80/day on weekends
- One main resource for explanations (e.g., UWorld) + one concise review source
- Focus on:
- Internal medicine systems (cardio, pulmonary, GI, renal)
- Beginning emergency-oriented topics (shock, sepsis, ED triage-type vignettes)
- Start a formula: each question → diagnosis, next best step, why not others
Weeks 5–8: Acceleration and EM Integration
- 40–80+ questions/day, 5–6 days/week
- Add timed, random blocks to simulate test conditions
- Emphasize:
- Trauma, neurology, OB-GYN emergencies, toxicology, pediatrics
- Imaging interpretation (X-ray, CT, CT head, CXR, abdominal CT)
- Take at least 1–2 NBMEs or self-assessments
- Use score trajectory to adjust your strategy
- Prioritize weak systems and EM-relevant emergencies
Weeks 9–11: Refinement and High-Yield Review
- Near-full exam load: 160–200 questions every 2–3 days
- Focus on:
- Mixed blocks to mirror exam
- Mistake patterns and knowledge gaps
- Rapid and repeated review of:
- Algorithms (e.g., chest pain, stroke, PE, GI bleed)
- Must-not-miss diagnoses and red flags
- Work on time management under test-like conditions
Week 12: Taper and Exam Readiness
- 1 full-length self-assessment 5–7 days before test day
- Lighter Qbank review: 40–60 questions/day
- Revisit:
- Personal notes, flashcards, or concept lists
- Common EM differentials and life-threatening conditions
- Prioritize sleep, nutrition, and mental readiness
Core Resources and How to Use Them Effectively
The IMG residency guide for Step 2 CK is not about collecting more resources; it is about using a few high-yield tools very well. For emergency medicine aspirants, think in terms of “question mastery + targeted clinical thinking.”
Question Banks: Your Primary Learning Engine
UWorld Step 2 CK
- Should be your main Qbank. Aim to complete 100% of questions once, and if possible, review incorrects a second time.
- Use tutor mode initially for learning, then timed mode as you approach exam day.
- For EM, pay special attention to questions that involve:
- Rapid stabilization (“ABCs”)
- Next best step when vitals are unstable
- Disposition decisions (admit vs. observe vs. discharge)
Strategy Tips:
- Treat each question as a mini-patient in the emergency department:
- Identify life threats: airway, breathing, circulation, CNS compromise.
- Ask: “Is this patient sick or not sick?” before diving into details.
- Decide what immediate intervention cannot be delayed (e.g., IV fluids, airway, antibiotics).
- Maintain a “Concept Log”:
- Instead of copying entire explanations, write:
- What the question was testing
- Why your choice was wrong
- The key takeaway you must remember
- Instead of copying entire explanations, write:
If your baseline is lower or you finished UWorld early, you may consider a secondary Qbank (e.g., AMBOSS, Kaplan) for additional practice; however, depth and quality of review matter more than volume.
Content Review: Efficient, Not Exhaustive
You do not need a giant textbook. For a focused USMLE Step 2 CK preparation, choose:
- Concise review resources (e.g., high-yield Step 2 CK notes, videos, or outlines)
- EM-oriented tools like brief algorithms from EM texts or clinical handbooks for:
- Chest pain
- Shortness of breath
- Abdominal pain
- Trauma and head injury
- Sepsis and shock
As an IMG, you may have gaps in guideline-based management compared with U.S. graduates. Pay particular attention to:
- ACS (NSTEMI/STEMI) management steps
- Stroke pathways (time windows for thrombolysis, thrombectomy)
- Sepsis bundles and broad-spectrum antibiotic choices
- Evidence-based use of CT scans and imaging in trauma and abdominal pain
Practice Exams and NBMEs
Use these strategically:
- First NBME: ~8–10 weeks before your test, to ground your timeline
- Second NBME: 3–5 weeks before your test, to evaluate if you’re near your target Step 2 CK score
- Final NBME/UWSA: 5–10 days before test day
Review not only what you got wrong, but why you chose wrong:
- Misread vital signs?
- Ignored a red-flag symptom?
- Followed an “outpatient” mindset instead of an “emergency/acute” mindset?
High-Yield EM Clinical Thinking for Step 2 CK
This USMLE Step 2 CK preparation strategy section is specifically tailored to the way EM programs expect you to think—pattern recognition plus immediate, safe decision-making.
Principle 1: Stabilization Before Diagnosis
On the exam, just as in the ED, you often must act before knowing the exact diagnosis.
Example: Hypotensive Trauma Patient
A 25-year-old male after a motor vehicle collision, hypotensive with tachycardia and altered sensorium.
- Wrong mindset: “Let’s order a CT scan first to find the source of bleeding.”
- Right Step 2/EM mindset: “Recognize hemorrhagic shock → Immediate IV access, fluid resuscitation, blood products, and activate trauma protocol; imaging only when patient is stabilized or as per protocol.”
Always ask:
- Are there signs of shock?
- Is airway protected?
- Are breathing and oxygenation adequate?
- Is there a need for emergent intervention (intubation, pericardiocentesis, chest tube, etc.)?
Principle 2: Recognize Red Flags and Do Not Delay Care
Step 2 CK often tests your ability to detect dangerous presentations and escalate promptly.
- Chest pain + diaphoresis + ST-elevation → immediate reperfusion, do not delay with extra testing.
- Sudden severe headache, “worst of my life” → consider subarachnoid hemorrhage; CT head and emergent evaluation, not outpatient follow-up.
- High fever, neck stiffness, altered mental status → treat as meningitis; start antibiotics immediately after (or even before) LP when indicated.
As an IMG, train yourself away from a purely “theoretical” approach and toward risk-based decision making.
Principle 3: Learn Adult and Pediatric Pearls
Emergency departments see all ages; Step 2 CK expects you to manage both adequately.
Adult vs Pediatric Considerations:
Dehydration:
- Adults: Oral or IV fluids based on severity; watch comorbidities.
- Children: Weight-based fluid boluses; recognize signs like sunken fontanelles, poor tears, delayed capillary refill.
Respiratory Distress:
- Adults: COPD exacerbation, PE, pneumonia; emphasize ABGs, imaging, oxygen strategy.
- Children: Bronchiolitis, croup, foreign body aspiration; evaluate stridor vs wheeze, use appropriate imaging and interventions (racemic epinephrine, steroids, etc.).
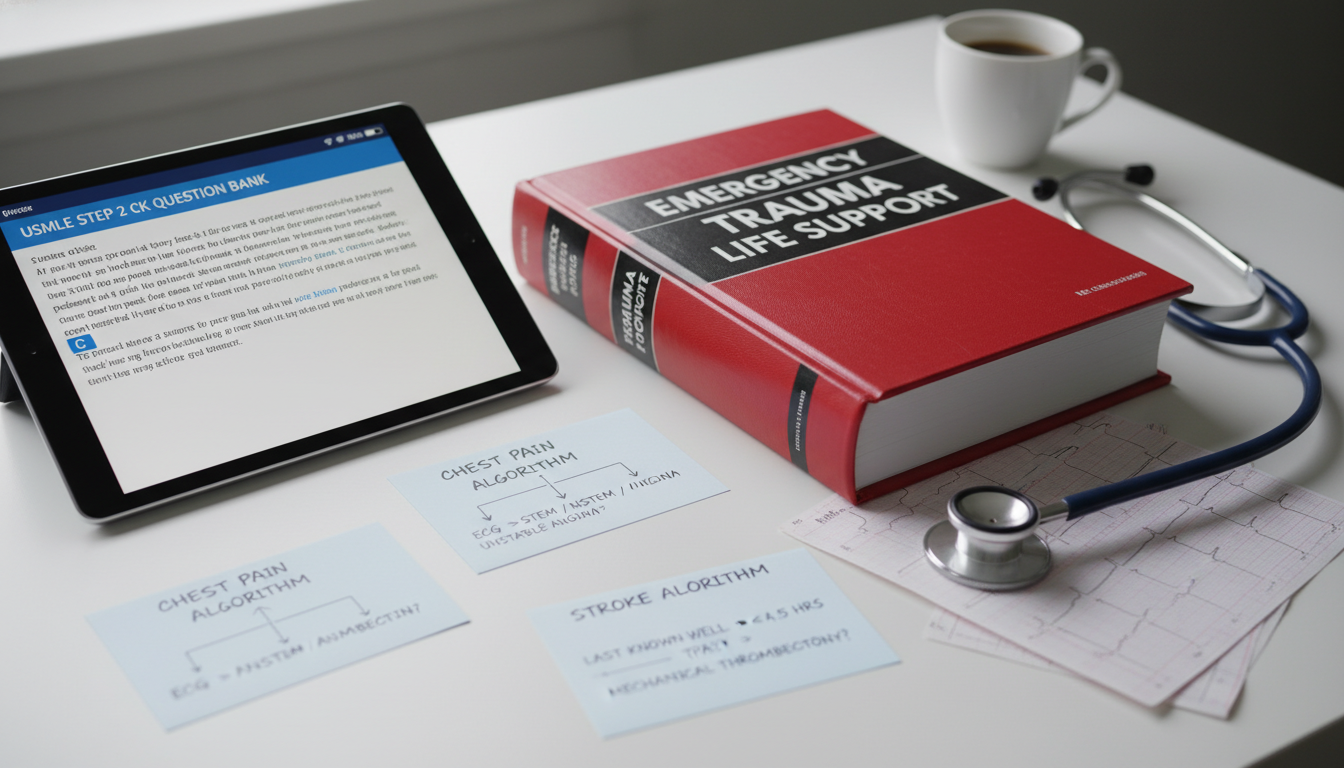
Principle 4: Master ED Algorithms for Common Complaints
In USMLE Step 2 study, build mental algorithms for the most common EM presentations.
Key complaint-based frameworks:
- Chest pain:
Rule out ACS, PE, aortic dissection, tension pneumothorax, pericarditis. Use risk factors, ECG, troponins, and vitals to triage urgency. - Shortness of breath:
Differentiate between pulmonary (PE, asthma, COPD), cardiac (CHF, ACS), and metabolic (DKA) causes. - Altered mental status:
Use AEIOU TIPS (Alcohol, Endocrine/Electrolytes, Infection, Opiates, Uremia, Trauma, Insulin, Poisoning, Stroke/Seizure etc.). - Abdominal pain:
Localize (RUQ vs RLQ vs epigastric vs diffuse); consider appendicitis, cholecystitis, pancreatitis, ectopic pregnancy, perforation, obstruction, etc.
Writing and reviewing such algorithms regularly during Step 2 CK preparation helps internalize ED-style reasoning.
Integrating Step 2 CK Preparation With the EM Match as an IMG
Your Step 2 CK score doesn’t exist in isolation; it interacts with every other aspect of your EM residency application.
Timing Step 2 CK Around ERAS and Interviews
For the EM match, consider:
- Taking Step 2 CK early enough that your score is available by:
- ERAS application opening (ideally), or
- At least before program rank list decisions.
- If your Step 1 is weaker, or pass/fail with no numeric score:
- Programs may heavily rely on Step 2 CK as your main standardized metric.
- Earlier exam + strong score can help you secure more interview invitations.
Using Your Step 2 CK Experience in EM Interviews
You can turn your exam preparation into a strength:
- Describe how question-based learning sharpened your clinical reasoning in acute care.
- Mention specific EM-related topics that you mastered (e.g., sepsis bundles, ACS algorithms) and how you applied them during U.S. clinical experiences or observerships.
- Highlight how you learned to think in algorithms and risk-stratification, mirroring EM workflows.
Common IMG Challenges and Solutions
Challenge 1: Differences in Guidelines and Practice Patterns
- Your home country may use different antibiotics, imaging access, or triage systems.
- Solution:
- Rely on U.S.-oriented resources (UWorld, NBME, U.S. guidelines).
- Compare “how I was trained” vs “how U.S. guidelines recommend acting” and deliberately switch to the latter for exam questions.
Challenge 2: Language and Reading Speed
- Long vignettes in English can slow you down.
- Solution:
- Practice reading question stems actively: underline or mentally note vitals, risk factors, time course.
- Reduce subvocalization; train by timed reading exercises with Qbanks.
- Practice “skimming for danger” first: look at vitals, age, key symptoms before details.
Challenge 3: Limited U.S. Clinical Exposure
- You may lack real-life EM context.
- Solution:
- Watch high-quality EM cases or lectures online (e.g., emergency medicine grand rounds, case-based conferences).
- Mentally simulate how you would manage the patient in a U.S. ED before checking the answer.
Frequently Asked Questions (FAQ)
1. What Step 2 CK score do I need as an IMG to match into emergency medicine?
There is no universal cutoff, but for an IMG, a Step 2 CK score at or above the national mean is often considered a minimum to be broadly competitive. Many strong EM applicants, especially IMGs, aim for > 240–245 to strengthen their profiles, especially if they have limited U.S. clinical experience or average Step 1 performance. Remember that your entire application—SLOEs, USCE, research, and interviews—also heavily influences match outcomes.
2. How early should I take Step 2 CK if I’m applying for the EM match as an IMG?
Ideally, take Step 2 CK at least 2–3 months before ERAS applications open, so that your score appears on your initial application. If that’s not possible, try to have your score released before most interview invites are sent (usually by late fall). For IMGs, earlier and stronger Step 2 CK scores can be especially beneficial, as programs may use this to compensate for unfamiliar schools or limited U.S. experience.
3. Can I prepare for Step 2 CK while doing U.S. clinical rotations or observerships in emergency medicine?
Yes, and this can be very powerful if managed well. Use clinical experiences to reinforce your studying:
- After a shift, review conditions you saw (e.g., sepsis, chest pain) using your Qbank or notes.
- Apply ED algorithms from your study resources to real patients.
- Ask supervising physicians about why certain decisions were made; compare this with what you’ve learned from UWorld or NBMEs.
Time management is critical—consider slightly extending your exam timeline if your rotations are very demanding.
4. I already did poorly on Step 1. Can a strong Step 2 CK score still help me get an EM residency as an IMG?
Yes. A strong Step 2 CK score is one of the most effective ways to rebuild your academic narrative. EM programs value clinical performance and decision-making; Step 2 CK reflects that more directly than Step 1. If you can show a significant upward trend (for example, from a below-mean Step 1 to a strong Step 2 CK), combined with solid SLOEs, good USCE, and a coherent story in your personal statement, many programs will consider you seriously.
By structuring your USMLE Step 2 CK preparation around emergency medicine–relevant thinking, focusing on high-yield question-based learning, and aligning your test timing with the EM match cycle, you can turn this exam into a major asset in your journey as an international medical graduate seeking an emergency medicine residency in the United States.






















