
Understanding Residency Work Hours in a Transitional Year
Transitional Year (TY) programs occupy a unique space in graduate medical education. For many residents, this is the bridge between medical school and a chosen advanced specialty (anesthesiology, dermatology, radiology, radiation oncology, PM&R, etc.). The transitional year residency is often described as “lighter” than categorical programs—but that can be misleading. You’ll still be working hard, navigating residency work hours, and trying to protect your resident work life balance in an unfamiliar environment.
Managing residency work hours effectively during your TY program is not just about surviving; it’s about using this year strategically to grow, build professional habits, and enter your advanced specialty healthy and prepared.
This guide will walk you through:
- What to expect from duty hours in a transitional year
- How ACGME work hour rules apply to you
- Common rotation structures and pitfalls
- Concrete strategies to manage your time, energy, and burnout risk
- How to advocate for yourself when work hours become unsustainable
The Framework: ACGME Duty Hours and How They Apply to You
Before you can manage work hours, you need to understand the rules that govern them. These rules are often referred to as “duty hours” or “ACGME duty hour standards.”
Core ACGME Duty Hour Rules (for TY Residents)
While exact wording can vary, the following principles typically apply to transitional year residency programs accredited under the ACGME:
80-hour work week limit
- Averaged over 4 weeks
- Includes all in-house clinical duty, required conferences, and at-home call that results in hospital work
- Moonlighting usually counts toward the 80-hour limit
1 day off in 7
- Also averaged over 4 weeks
- “Day off” means a continuous 24 hours free of clinical and educational duties
Maximum shift length (in-hospital)
- For most TY residents (PGY-1), scheduled continuous duty is no more than 16–24 hours, depending on the program’s specific interpretation and updates. Many TY programs have moved away from very long 24+4 shifts for interns and toward shorter in-hospital shifts.
Time between shifts (rest periods)
- Generally, at least 8 hours free between scheduled duty periods for PGY-1
- Programs often aim for 10 hours of rest whenever feasible
Night float and call systems
- Night float rotations are structured to comply with maximum weekly hours and minimum rest periods
- At-home call (pager call) still has limitations, especially when it leads to substantial in-hospital time
These rules are designed to protect you, your learning, and your patients. However, how they are implemented in a specific TY program can vary dramatically.
How TY Programs Differ from Categorical Programs
Transitional year residency programs:
- Often emphasize diversity of rotations: internal medicine, emergency medicine, ICU, ambulatory, electives, sometimes surgery or OB
- Typically have fewer heavy inpatient months than categorical IM or surgery programs
- May offer more elective time, which can create better flexibility and work life balance
- Still must satisfy similar ACGME duty hour requirements as other preliminary or categorical intern years
This mix means that your residency work hours may swing widely from month to month. Medicine wards and ICU can feel intense, while electives and ambulatory blocks may be comparatively lighter. Effective management is about planning for both the heavy and the light months.
What Does a Transitional Year Schedule Actually Look Like?
Understanding the common schedule patterns in TY programs will help you anticipate challenges and opportunities for maintaining a healthy resident work life balance.
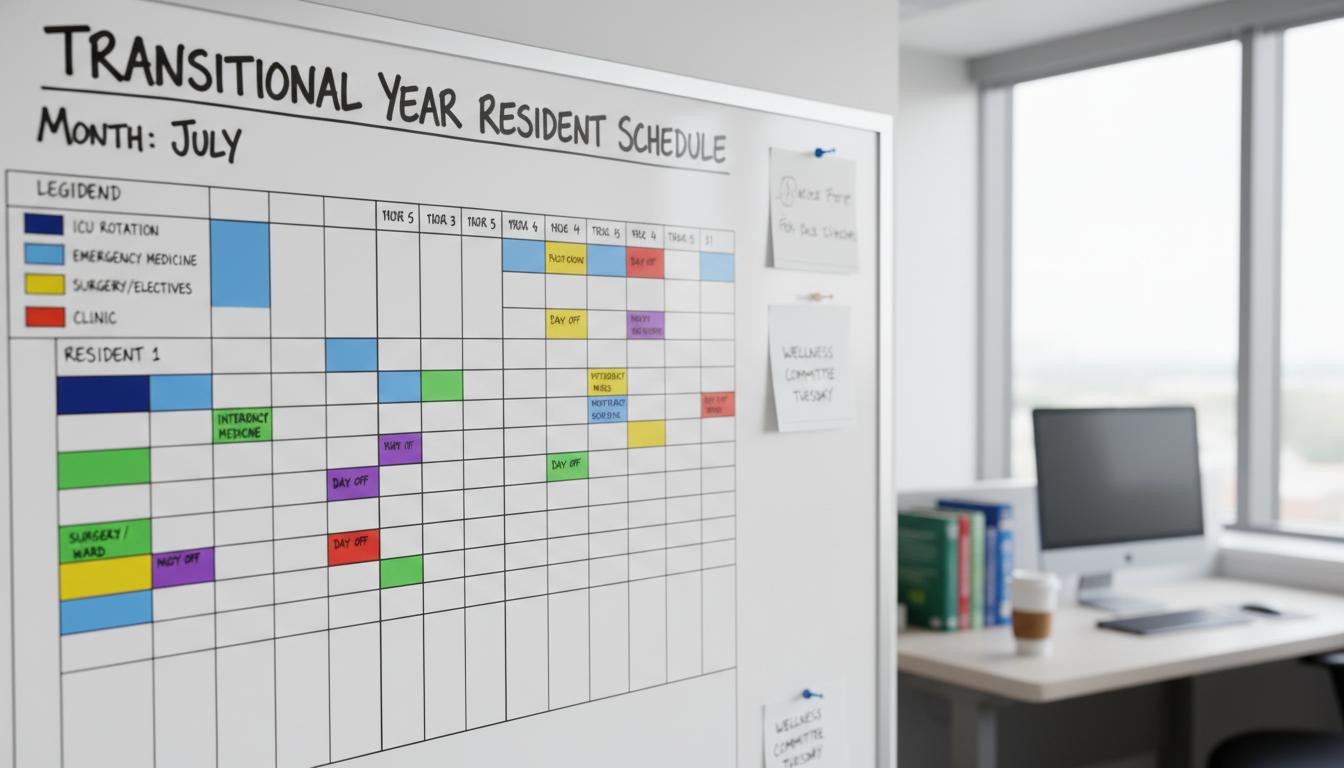
Typical Rotation Mix and Work Hours
While each TY program is different, a representative schedule might look like:
4–6 months of inpatient medicine or subspecialty wards
- Example: General medicine, cardiology, oncology, neurology inpatient
- Hours: 60–80 hours/week, depending on call/night float structure
- Weekends: Often 2–3 weekends per month
1–2 months of ICU or CCU
- Hours: 65–80 hours/week
- Intense shifts, night call, and rapid decision-making
1–2 months of emergency medicine
- Hours: Often 40–55 hours/week
- Mostly shift-based, including nights and weekends
- Fewer “residual” tasks to carry home compared to wards
2–4 months of electives/ambulatory
- Outpatient clinics, subspecialty consults, specialty-specific electives (e.g., radiology, derm, anesthesia, PM&R)
- Hours: 40–55 hours/week
- More predictable schedules and better opportunity to work on research, personal life, and advanced residency preparation
Example Week: Busy Inpatient Month
Monday–Friday (Medicine Wards)
- 6:30 am: Pre-round
- 7:30 am: Team rounds
- 12:00 pm: Noon conference (required)
- 1:00–5:30 pm: Admissions, discharges, cross-coverage, notes
- 6:00–7:30 pm: Wrap-up, sign-out
- Some days: Stay until 9–10 pm for late admissions depending on call system
Weekend
- One full day on call (long day or 24-hour call)
- One day off
Average: 70–80 hours/week.
Example Week: Outpatient / Elective Month
Monday–Friday (Ambulatory Clinic + Elective)
- 8:00 am–5:00 pm: Clinic, consults, or elective activities
- Protected didactics once or twice per week
- Evenings generally off, with rare late notes or reading
Weekend: Often both days off or minimal duties.
Average: 40–50 hours/week.
Recognizing how your schedule fluctuates allows you to bank rest, relationships, and personal projects during lighter months to offset the heavier rotations.
Practical Strategies to Manage Residency Work Hours
Managing duty hours in a TY program is less about “doing less work” and more about working deliberately, controlling what you can, and building sustainable habits.
1. Be Meticulous About Time Management on Busy Rotations
On wards and ICU, wasting 10–15 minutes repeatedly adds up to hours of extra time in the hospital each week.
Practical tactics:
Structured prerounding:
- Make a checklist: vitals, labs, overnight events, imaging, new consults, active orders
- Use a standardized template for your notes so you can populate them quickly while prerounding
Batch similar tasks:
- Place multiple orders at once instead of piecemeal
- Call all consults in a batch, starting with the most urgent
- Batch phone calls to nurses and case management when possible
Optimize your rounding workflow:
- Pre-identify “quick update” patients vs. “complex discussion” patients
- Anticipate likely plan changes (e.g., “If K < 3.5, I’ll replete; if ready for discharge, I’ll place orders by noon”)
Use micro-deadlines during the day:
- “All progress notes done by 3 pm”
- “All discharge summaries drafted before sign-out”
- This protects your evening and reduces last-minute scrambling
2. Make Documentation Work for You, Not Against You
Documentation is one of the most time-consuming parts of residency. Refining your approach can significantly reduce residency work hours.
Documentation strategies:
Templates and smart phrases:
- Create commonly used dot phrases for HPI structures, assessments, and plans by problem
- Use checklists or bullet points rather than writing full paragraphs where appropriate
Document in real time when possible:
- Start drafting notes while on rounds (if your team culture allows)
- Update assessments immediately after seeing a patient, rather than reconstructing things from memory later
Avoid over-documenting mental clutter:
- Focus on decision-making, assessment, and clear plans, not every possible differential when not relevant
- Be concise but complete—remember, your goal is clarity, not length
Example:
Instead of:
“The patient is a 68-year-old with a history of…” (rewriting the entire history each day)
Use:
“68-year-old with HTN, CAD, HFpEF admitted with decompensated heart failure, now improving (see H&P 12/1 for full details).”
Then focus the day’s note on what changed.
3. Protect Your Resident Work Life Balance Proactively
Your transitional year residency is demanding but finite. How you use this time can determine whether you arrive at your advanced specialty burned out or mentally strong.
Set non-negotiable boundaries:
- Sleep floor: Decide your minimum acceptable sleep (e.g., 6 hours on nights, 7–8 on lighter rotations) and prioritize it relentlessly
- Protected personal time: Identify at least one consistent block each week (e.g., Saturday morning or a weekday evening) that you do not surrender lightly to extra work unless absolutely necessary
- Technology boundaries:
- Turn off non-essential notifications when you’re off duty
- Avoid constantly checking EMR or work email when you are not on call
Use lighter rotations wisely:
- Rebuild your sleep debt in a healthy way
- Re-engage in exercise routines (even simple 20-minute home workouts or walks)
- Reconnect intentionally with friends/family
- Work on long-term professional tasks (research, advanced specialty reading, step exams if applicable) without overwhelming your rest time
4. Manage Nights and Shift Work Strategically
Night shifts and night float are a reality in many TY programs. Poor management can severely disrupt your physical and mental health.
Before night float:
- Gradually adjust your sleep schedule by shifting 1–2 hours later each night in the few days leading up to nights
- Prepare meal options (easy-to-reheat, not too heavy) ahead of time
- Arrange transportation if fatigue might make driving unsafe
During nights:
- Use strategic caffeine, not constant caffeine:
- Small doses early or mid-shift rather than huge amounts late in the night
- Short power naps during permissible breaks can maintain alertness
- Maintain a written checklist to combat “decision fatigue” at 3–5 am
After nights (post-call):
- Avoid driving home if too sleepy—consider carpooling, ride-sharing, or hospital fatigue policies
- Take a short nap (1–3 hours) after your last night, then try to reset to a day schedule
- Use sunglasses on the way home and a dark, cool room to improve sleep quality
Advocating for Yourself When Duty Hours Are a Problem
Even in well-run TY programs, there will be times when residency work hours push the limits of what feels safe or sustainable. Advocacy is both a professional responsibility and an important skill.

Recognizing When Work Hours Are Unsafe or Noncompliant
Red flags that your duty hours may be out of bounds:
- Consistently >80 hours/week over several weeks
- Regularly missing your 1 day off in 7 over multiple 4-week blocks
- Frequently working 28+ hours in a row or without adequate rest
- Feeling unable to safely commute home due to fatigue
- Making or nearly making significant patient care errors directly related to exhaustion
Remember, ACGME duty hours are not “suggestions”—they are requirements designed to protect patient safety and resident well-being.
How to Approach Concerns Professionally
Collect data for 2–4 weeks:
- Record your start/end times, call shifts, and days off
- Note any particularly unsafe situations (e.g., near-miss errors from fatigue)
Start locally:
- Discuss with your senior resident or chief resident
- Ask if your experience is typical and whether adjustments are possible (e.g., redistributing admissions, help with discharges)
Escalate thoughtfully if needed:
- If systemic issues persist, schedule a calm, factual meeting with your program director or associate PD
- Emphasize safety and learning rather than only personal inconvenience
Example framing:
“Over the last 4 weeks I’ve averaged around 85–88 hours per week, and have only had 2 full days off. I’m concerned about my ability to learn effectively and care for patients safely when I’m this fatigued. I’ve kept a log of my hours and wanted to discuss possible solutions.”
- Know your institutional resources:
- GME office or resident well-being committees
- Anonymous reporting mechanisms
- ACGME resident survey (taken annually; your honest feedback matters)
Professional advocacy is not “complaining”; it’s participating in quality improvement for your training environment.
Using Your Transitional Year to Build Long-Term Work-Hour Habits
The transitional year residency offers a rare opportunity: you are learning intense inpatient medicine but not yet locked into a single specialty’s long-term culture. This is the ideal time to build healthy patterns.
1. Clarify Your Long-Term Priorities
Ask yourself:
- What kind of physician lifestyle do I want in 5–10 years?
- How important is schedule predictability, clinic vs. hospital work, or academic vs. private practice?
- What boundaries must I maintain to stay emotionally healthy and engaged?
Use your TY experiences—both good and bad—to refine what kind of professional life you’re aiming for.
2. Learn From Different Rotations and Attendings
Each rotation exposes you to attendings and seniors who manage similar duty hours very differently.
- Identify attendings who seem efficient yet kind and organized yet flexible
- Ask directly:
- “How do you structure your day so that you can leave on time most days?”
- “What documentation habits save you the most time?”
- “What do you wish you had done differently as an intern to protect your time?”
Adopt and adapt their strategies. TY is perfect for experimentation.
3. Build Systems You Can Transfer to Your Advanced Specialty
Whether you’re heading into dermatology, radiology, anesthesia, PM&R, or another field, some skills are universally transferable:
- Task capture system (notebook, digital app, EMR to-do lists) so nothing falls through the cracks
- Prioritization framework:
- Emergent (must do now), urgent (by today), important (by tomorrow), optional (when time allows)
- Weekly review ritual:
- 20–30 minutes once a week to review upcoming shifts, academic deadlines, personal obligations, and rest needs
If you learn to manage unpredictable hours in your TY year, later training phases—often more specialized but still demanding—will feel more manageable.
FAQs: Managing Residency Work Hours in a Transitional Year
1. Are transitional year residency programs really better for work life balance?
TY programs often have more elective and outpatient time and may feel lighter than categorical internal medicine or surgery internships. However:
- Inpatient and ICU months can still hit 70–80 hours/week
- Call systems vary widely by program
- Some TY programs affiliated with big academic centers can be just as intense as categorical programs
When researching programs, ask specifically about duty hours, call structure, and percentage of elective time.
2. How can I compare residency work hours between different TY programs during the application process?
Use these strategies:
- Ask residents during interviews:
- “What is a typical week like on medicine wards? On ICU? On electives?”
- “How often do people hit close to 80 hours?”
- “How many weekends off do you get per month on average?”
- Check if programs advertise:
- Night float vs 24-hour call
- Frequency of ICU months
- Percentage of elective months
- Look at resident wellness initiatives and attrition; high burnout or frequent transfers are warning signs
3. Is it okay to moonlight during my transitional year?
Moonlighting policies vary by institution and state, and some programs do not allow TY residents to moonlight at all. If allowed:
- All moonlighting hours count toward the 80-hour ACGME duty hour limit
- Patient safety and your own rest must come first
- Moonlighting should never interfere with your primary residency responsibilities
Discuss with your program director, and get formal approval before starting any moonlighting.
4. How do I maintain any sense of personal life on 70–80 hour weeks?
It’s possible but requires intentional choices:
- Simplify basics: meal prepping, scheduled laundry days, autopay for bills
- Protect small rituals: a weekly coffee with a friend, video call with family, a short workout or walk
- Avoid perfectionism: your apartment won’t always be tidy, and hobbies may shrink temporarily; that’s normal for this phase
- Use your lighter rotations to more fully re-engage socially and personally
The goal is not perfect balance every week but a sustainable pattern over months, where periods of intensity are followed by periods of real recovery.
Managing residency work hours in a transitional year is less about “having an easy year” and more about learning how to train sustainably. By understanding duty hour rules, planning around rotation-specific demands, setting realistic boundaries, and advocating when needed, you can finish your TY program not only competent and confident, but also ready—physically and mentally—for the next stage of your training.






















