
Understanding Combined vs Categorical Programs in Medicine-Psychiatry
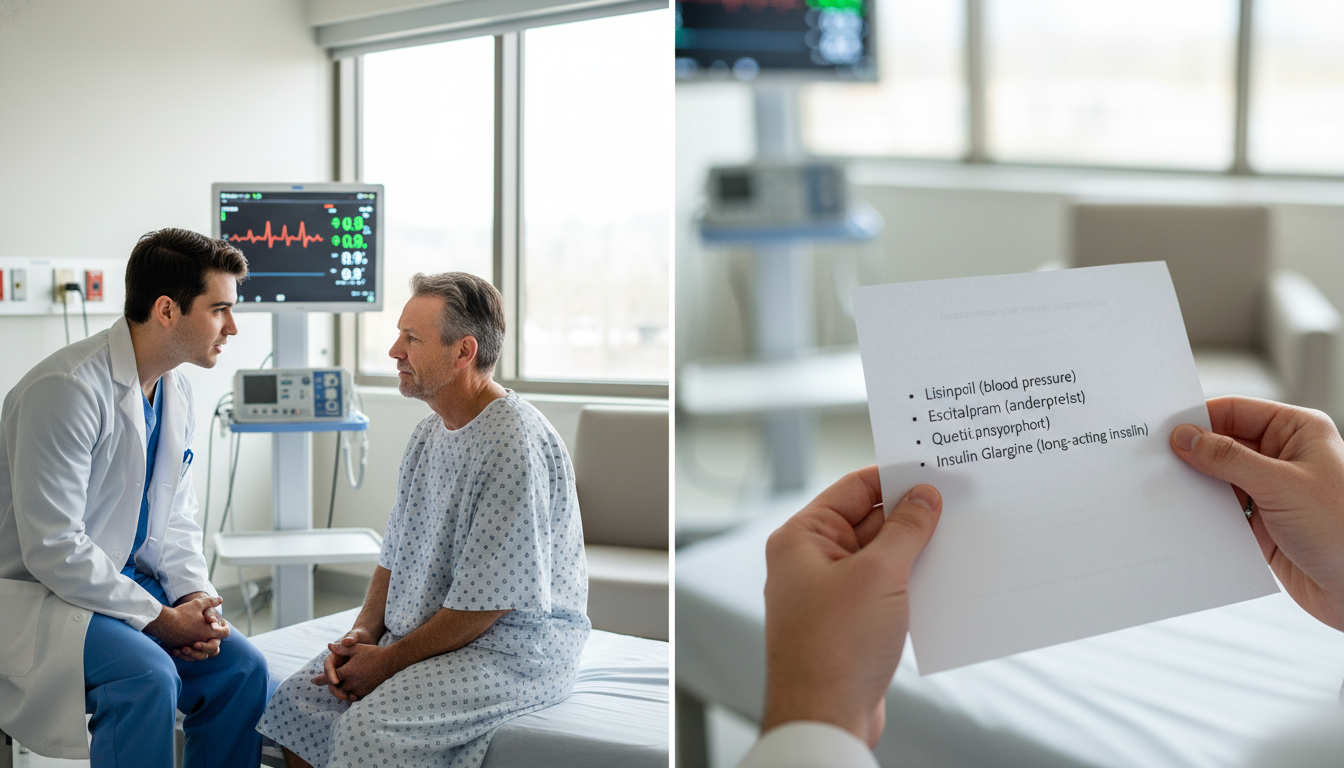
Choosing between combined vs categorical pathways is one of the most strategic decisions for students interested in Medicine-Psychiatry. With the growing emphasis on integrated care and complex comorbidities, it’s essential to understand how a med psych residency (Medicine-Psychiatry combined residency) compares to traditional categorical training.
This guide focuses on:
- How combined Medicine-Psychiatry residencies are structured
- How they differ from categorical Internal Medicine and Psychiatry programs
- Who tends to thrive in each path
- How this choice influences fellowship options, careers, and lifestyle
- Practical tips to decide which path is right for you
Key Definitions: What Do “Categorical” and “Combined” Really Mean?
Before comparing paths, it’s important to clarify terminology that can be confusing during residency applications.
What is a categorical residency?
A categorical residency is a standard, stand-alone residency in a single specialty that leads directly to board eligibility in that field.
For Medicine-Psychiatry applicants, the relevant categorical programs are:
Categorical Internal Medicine
- Length: 3 years
- Outcome: Eligibility for American Board of Internal Medicine (ABIM) certification
- Focus: Diagnosis and management of adult medical illness, inpatient wards, ICU, ambulatory medicine
Categorical Psychiatry
- Length: 4 years
- Outcome: Eligibility for American Board of Psychiatry and Neurology (ABPN) certification in General Psychiatry
- Focus: Diagnosis and management of psychiatric disorders across settings—outpatient, inpatient, consult-liaison, emergency, partial hospitalization, etc.
What is a Medicine-Psychiatry combined residency?
A Medicine-Psychiatry combined residency (often called “Med-Psych”) is an integrated training program that leads to dual board eligibility in both Internal Medicine and Psychiatry.
Key features:
- Length: Typically 5 years
- Outcome: Eligibility for both ABIM and ABPN boards
- Accreditation: Jointly approved by the relevant boards and ACGME
- Curriculum: Alternating or blended blocks of Internal Medicine and Psychiatry with specific requirements in each
These are often referred to as:
- Med Psych residency
- Medicine psychiatry combined residency
- Internal Medicine-Psychiatry combined program
Note: Don’t confuse Med-Psych with Med-Peds (Internal Medicine–Pediatrics), which is a different combined residency focused on dual training in adult and pediatric medicine. Many programs exist in both domains, and applicants sometimes compare med peds program structures to Med-Psych while exploring options.
Training Structure: How Med-Psych Compares to Categorical Paths
Understanding day-to-day and year-to-year structure is crucial when comparing categorical vs combined programs.
Categorical Internal Medicine: Classic 3-Year Track
Length: 3 years
Core experiences:
- Inpatient ward rotations (general medicine, subspecialties)
- ICU/CCU
- Night float
- Ambulatory continuity clinic
- Subspecialty electives (cards, GI, ID, heme/onc, pulm/crit, etc.)
Identity and focus:
- Strong focus on medical complexity, diagnostics, procedures (depending on program), and systems-based practice
- Prepares you for a broad range of fellowships (cards, GI, pulm/crit, ID, rheum, etc.) or hospitalist/primary care careers
Categorical Psychiatry: Classic 4-Year Track
Length: 4 years
Core experiences:
- Inpatient psychiatry (acute, chronic, specialty units)
- Outpatient psychiatry (longitudinal clinics)
- Consultation-liaison psychiatry (psych in medical settings)
- Emergency psychiatry
- Neurology rotations
- Addiction, child & adolescent, geriatric psychiatry exposure
Identity and focus:
- Depth in psychotherapy, psychopharmacology, systems of mental health care, community psychiatry, and subspecialty psych fields
- Prepares for fellowships (CL psychiatry, addiction, forensics, child & adolescent, geriatric, etc.) or general practice
Medicine-Psychiatry Combined Residency: The Integrated 5-Year Path
Length: 5 years (most programs)
Credential outcome:
- Completion of both medicine and psychiatry requirements
- Eligible for dual board certification: ABIM (Internal Medicine) and ABPN (Psychiatry)
Typical rotation mix:
- Roughly 30 months Internal Medicine and 30 months Psychiatry
- Scheduling models vary:
- Some alternate every 3–6 months (e.g., 3 months IM, 3 months Psych)
- Others use yearly themes with both specialties included each year
- Senior years often include integrated or hybrid rotations (e.g., med-psych inpatient units)
Unique Med-Psych elements:
- Integrated rotations caring for patients with complex medical-psychiatric comorbidities
- Consult-liaison experiences where you are uniquely qualified to manage both dimensions
- Longitudinal continuity clinics in both medicine and psychiatry
- Exposure to systems that integrate behavioral health and primary care
- Often strong emphasis on severe mental illness with chronic medical disease, such as:
- Schizophrenia plus diabetes or heart disease
- Bipolar disorder with obesity/metabolic syndrome
- Substance use plus chronic liver or lung disease
Core Differences: Categorical vs Combined in Medicine-Psychiatry
Below are the most practical and impactful differences to consider.
1. Length of Training and Opportunity Cost
- Categorical Internal Medicine: 3 years
- Categorical Psychiatry: 4 years
- Med-Psych combined residency: 5 years
If you were to complete both categorical residencies sequentially, it would be 7 years (3 + 4). A Medicine-Psychiatry combined residency compresses this into 5 years, integrating training and avoiding redundancy.
Implication:
- You spend 2 fewer years in training vs doing both categorical residencies separately.
- Compared to a single categorical program, you add 1–2 extra years but gain dual board eligibility.
2. Depth vs Breadth
Categorical programs (IM or Psychiatry):
- Deep specialization in one field
- Time to develop a single professional identity
- More elective time dedicated to that specialty’s subspecialties
- Less role confusion and fewer competing demands
Combined Medicine-Psychiatry:
- Broader but still substantial training in both fields
- You sacrifice some depth in subspecialty exposure in exchange for breadth and integration
- The program is carefully structured to meet all board requirements, but the “extra” elective time you might use for advanced subspecialization may be more limited
Rule of thumb: If your dream is high-level subspecialty work in one field (e.g., cardiology research career, or very niche psychotherapy focus), a categorical route plus fellowship may be more optimal. If your dream is to sit at the intersection of both medicine and psychiatry every day, combined may be ideal.
3. Professional Identity and Daily Practice
Categorical Internal Medicine:
- Identity: internist, hospitalist, primary care physician, subspecialist
- Clinical life: primarily medical disease, with frequent psychiatric comorbidity you may refer or co-manage
Categorical Psychiatry:
- Identity: psychiatrist, psychotherapist, consultant
- Clinical life: primarily mental health, with varying comfort in managing general medical issues
Med-Psych combined residency:
- Identity: dual-trained physician—often seen as a “bridge” between medicine and psychiatry
- Clinical life may include:
- Inpatient med-psych units
- Psychiatry consults for medically complex cases
- Primary care for patients with serious mental illness
- Leadership in integrated care teams
Some graduates continue to practice a fairly even mix of both fields; others lean more heavily into one specialty while maintaining strong skills in the other.
4. Career Flexibility and Job Market
With categorical Internal Medicine:
- Clear pathways:
- Fellowship: cardiology, GI, pulmonary/critical care, ID, etc.
- Hospitalist medicine
- Primary care or academic IM
- Psychiatry interest can still be pursued via:
- Strong CL psychiatry collaborations
- Additional formal psychiatry training (less common)
- Behavioral health integration work with psychiatrists and psychologists
With categorical Psychiatry:
- Clear pathways:
- Outpatient or inpatient psychiatry
- CL psychiatry
- Subspecialty fellowships (addiction, child/adolescent, forensics, geriatrics, etc.)
- Can develop strong collaboration with primary care and medical services, but formal authority in medical management is limited to basic medicine comfort and local policies
With Med-Psych combined residency:
You can function as:
- A general internist (hospitalist, primary care)
- A general psychiatrist
- Or a dual-role physician with integrated or specialized practices such as:
- Leading inpatient med-psych units
- Running integrated primary care–behavioral health clinics
- Serving as a consult-liaison psychiatrist with deep comfort in managing complex medical regimens
- Directing programs for populations like:
- People with severe mental illness and high medical burden
- Substance use disorders with significant medical comorbidity
- Homeless or justice-involved populations
Job markets are generally favorable, with many hospitals and health systems seeking physicians who can address both medical and psychiatric needs. However, roles that explicitly recognize both skill sets are still emerging in some regions, so your local market and institutional culture matter.
5. Lifestyle and Rotational Transitions
Categorical residencies tend to have:
- More predictable progression within one specialty
- Fewer shifts in mindset between medicine and psychiatry
- An easier time developing long-term mentorship relationships within a single department
Med-Psych combined residency involves:
- Frequent transitions between medicine and psychiatry services
- Ongoing “mode switching” between highly biomedical and biopsychosocial frameworks
- Learning two sets of departmental cultures, politics, and workflows
- Potential for identity diffusion early on: “Am I a psychiatrist? Am I an internist?” (most trainees grow into their unique dual identity with time)
This can be mentally demanding but also intellectually stimulating and professionally rewarding.

How to Decide: Is a Med-Psych Combined Residency Right for You?
1. Clarify Your True Interest in Medicine vs Psychiatry
Ask yourself:
When I picture my future week, what am I doing most of the time?
- Managing blood pressures, heart failures, COPD exacerbations?
- Working with patients on trauma, mood, psychosis, addiction?
- Or explicitly navigating both at once in complex, integrated settings?
Do I feel energized by:
- Complex differential diagnoses and medical physiology?
- Deep longitudinal psychotherapeutic relationships and psychopharmacology?
- Both, to the point that I don’t want to give either up?
Actionable step:
During clinical rotations:
- Keep a simple log for 4–6 weeks: after each day, write which aspects of the day were most meaningful and why.
- Look for patterns: is one domain consistently giving you more satisfaction?
2. Consider Your Tolerance for Longer Training
A combined residency adds:
- +1 year compared with Psychiatry alone
- +2 years compared with Internal Medicine alone
Reflect on:
- Financial considerations (debt, family responsibilities, partner’s situation)
- Burnout risk: Are you energized by training, or eager to move quickly into attending life?
- Career return on investment: Will dual training realistically help you do what you uniquely want to do?
3. Think About Future Fellowship and Subspecialization
For each path, consider your long-term options:
Categorical Internal Medicine:
- Most straightforward path to IM subspecialty fellowships
- You can still work closely with psychiatry and integrated care teams
Categorical Psychiatry:
- Streamlined path to popular psych fellowships
- Depth in psychotherapy or a particular psychiatric subspecialty
Medicine-Psychiatry combined residency:
- Often eligible for fellowships in either Internal Medicine or Psychiatry, though:
- Competitiveness and expectations can vary
- Some subspecialty programs may be less familiar with Med-Psych backgrounds and may need clarification about your training
- Particularly synergistic fellowships:
- Consultation-Liaison Psychiatry
- Addiction Psychiatry or Addiction Medicine
- Geriatric Psychiatry (for medically complex older adults)
- Primary care or population health tracks
- Often eligible for fellowships in either Internal Medicine or Psychiatry, though:
If you already know you want something like interventional cardiology, a categorical Internal Medicine plus fellowship is more targeted than a 5-year Med-Psych track.
4. Understand the Nature of Positions You Want After Training
Best-suited for Med-Psych combined residency:
- Running or working on:
- Inpatient med-psych units
- Integrated primary care–behavioral health clinics for persons with serious mental illness
- Specialty clinics (e.g., HIV + serious mental illness, transplant psychiatry with heavy medical management responsibilities)
- Serving in roles where dual expertise is explicitly valued:
- Medical director of programs for complex comorbidity populations
- Leadership in quality improvement at the medicine–psychiatry interface
- Systems-level work in population health that integrates behavioral health
If your dream job is largely:
- Outpatient psychotherapy, or
- Highly procedural cardiology, or
- ICU-based critical care
…the combined pathway may not offer enough additional benefit relative to its length.
5. Evaluate Program Availability and Location Flexibility
There are far fewer Medicine-Psychiatry combined programs than categorical IM or Psychiatry. This has several impacts:
- You may need to move farther or to fewer geographic regions to pursue Med-Psych
- Competition can be significant due to small program sizes (often 2–4 residents per year)
- If you need to be in a particular city/region for family or personal reasons, categorical programs may offer more options
Practical tip:
Start early:
- Identify all Med-Psych programs via FREIDA and program websites
- Map them against your geographic preferences
- Decide if your commitment to dual training is strong enough to prioritize these limited locations
Application Strategy: Approaching the Match for Combined vs Categorical
If you are interested in Medicine-Psychiatry combined training, your application strategy should be deliberate.
1. Decide Whether to Apply to Combined Only, or Combined + Categorical
Common strategies:
Med-Psych only
- For highly committed applicants who are geographically flexible
- Risk: fewer total programs = higher match risk if not also applying categorical
Med-Psych + Categorical Psychiatry
- For applicants who know psychiatry will be their primary long-term identity if Med-Psych doesn’t work out
- Your narrative still needs to make sense: emphasize why psychiatry is a clear independent passion, and combined is an enriched variant
Med-Psych + Categorical Internal Medicine
- For applicants leaning more toward IM as their base identity
- Emphasize your interest in psychosocial aspects of medicine and complex comorbidity
Med-Psych + both categorical IM and Psych
- For applicants who want maximum flexibility but need a coherent narrative
- You’ll need to tailor personal statements and interviews carefully to avoid seeming unfocused
2. Tailor Your Personal Statement and Experiences
For Med-Psych programs, focus on:
- Concrete experiences where you managed or observed complex medical + psychiatric comorbidity
- Reflection on how you think across both domains (e.g., understanding how depression affects diabetes management)
- Demonstrated commitment:
- Research or QI at the medicine–psychiatry interface
- Involvement with integrated care clinics, CL psychiatry, addiction medicine, etc.
- Longitudinal work with populations with serious mental illness and medical burden
For categorical programs, avoid sounding like they are merely a “backup.” Instead:
- For Psychiatry: highlight why psychiatry alone is meaningful to you
- For Internal Medicine: highlight your interest in the humanistic and behavioral side of care while showing respect for pure IM paths
3. Prepare for Interview Questions Specific to Combined vs Categorical
Expect questions like:
- “Why Medicine-Psychiatry instead of just Internal Medicine or Psychiatry?”
- “If you had to pick one specialty, which would it be and why?”
- “How do you see yourself using dual training 5–10 years out?”
- “Tell us about a patient who convinced you that combined training was right for you.”
Have clear, honest answers prepared. Programs want to see that you’ve thought deeply about the extra year of training and the dual identity.
Frequently Asked Questions (FAQ)
1. Can I do a Med-Psych combined residency and still subspecialize later?
Yes, many Medicine-Psychiatry combined graduates pursue fellowships in either Internal Medicine or Psychiatry, such as:
- Consultation-Liaison Psychiatry
- Addiction Psychiatry or Addiction Medicine
- Geriatric Psychiatry
- Certain Internal Medicine subspecialties (depending on program and competitiveness)
However, if you’re aiming for a highly competitive IM fellowship (e.g., cardiology at a top academic center), some program leaders may be less familiar with Med-Psych training; you’ll need to clearly articulate your preparation and goals. It’s wise to ask Med-Psych program leadership about alumni fellowship placements.
2. If I’m unsure between Med-Psych and categorical Psychiatry, what should I prioritize?
If you are truly split, consider:
- How strongly you value medical complexity and internal medicine identity
- Your tolerance for an extra year of training and more frequent rotations shifts
- Whether your long-term job vision requires or strongly benefits from dual training
If your core passion is working as a psychiatrist (with medical comfort but not necessarily independent medical management responsibility), categorical Psychiatry may be sufficient, perhaps with a strong focus on CL psychiatry or collaborative care. If you want to independently manage both realms daily, Med-Psych is more aligned.
3. Do Med-Psych combined residents get paid more than categorical residents?
During residency, salary is generally determined by PGY level, not by specialty. Since Med-Psych is a 5-year program, you’ll reach PGY-5 and be paid at that level, similar to other 5-year programs (like some surgical or combined tracks). After training, your income depends on the jobs you choose—hospitalist, psychiatrist, academic faculty, leadership roles, etc.—rather than the fact of combined training alone.
4. Is it possible to switch from a Med-Psych combined residency to a categorical program (or vice versa)?
In some cases, yes, but it depends on:
- Your program’s structure and policies
- ACGME and board requirements for minimum time in each specialty
- Availability of categorical positions at your institution
Switching from Med-Psych to categorical Internal Medicine or Psychiatry is more common than going the other direction, and typically requires careful planning to ensure you meet specific board requirements. If you’re worried you might want to switch, discuss this candidly with mentors and program directors before and during training.
Choosing between combined vs categorical paths in Medicine-Psychiatry is ultimately a personal decision about how you want to practice, where you find meaning, and how you’re willing to invest your training years. If your passion lies squarely at the interface of physical and mental health, a Medicine-Psychiatry combined residency can be a powerful and efficient way to build a career that fully integrates both. If your interest is more focused within a single specialty, a categorical path—augmented by targeted experiences at the interface—may serve you better.
Use your rotations, mentors, and self-reflection to clarify what kind of physician you want to be, then select the pathway that most directly supports that vision.






















