Navigating the Residency Application Maze: An Expanded Step-by-Step Roadmap
The residency application process can feel like a complex maze—high stakes, many moving parts, and limited room for error. For medical students and international medical graduates, this phase is the gateway from undergraduate medical education into graduate training and ultimately independent practice. The decisions you make now influence not only where you train, but often the trajectory of your long-term career.
This roadmap breaks down the Residency Application and Match Process into clear, manageable steps. You’ll learn what to do, when to do it, and how to optimize each component of your ERAS application, from specialty choice through Match Day. Use it as a practical guide to plan, track, and refine your journey.
Understanding the Residency Application and Match System
Before you start uploading documents and writing personal statements, you need a solid grasp of how the system works. Understanding the structure of ERAS and the NRMP Match will help you make better strategic decisions and avoid preventable mistakes.
How the Match Process Works
In the United States, the National Resident Matching Program (NRMP) administers the Main Residency Match. Here’s the big-picture overview:
- You apply to programs using the Electronic Residency Application Service (ERAS).
- Programs review applications, select candidates to interview, and then submit a confidential Rank Order List (ROL) of applicants.
- You submit your own ROL of residency programs in order of true preference.
- The NRMP algorithm “matches” applicants and programs, prioritizing applicant preferences as much as possible within program constraints.
Key point: The Match algorithm is “applicant-favoring”—you should rank programs in your true preference order, not where you think you’re “most likely to match.”
Core Components of the Residency Application
Understanding each component early will help you build a more cohesive and competitive application.
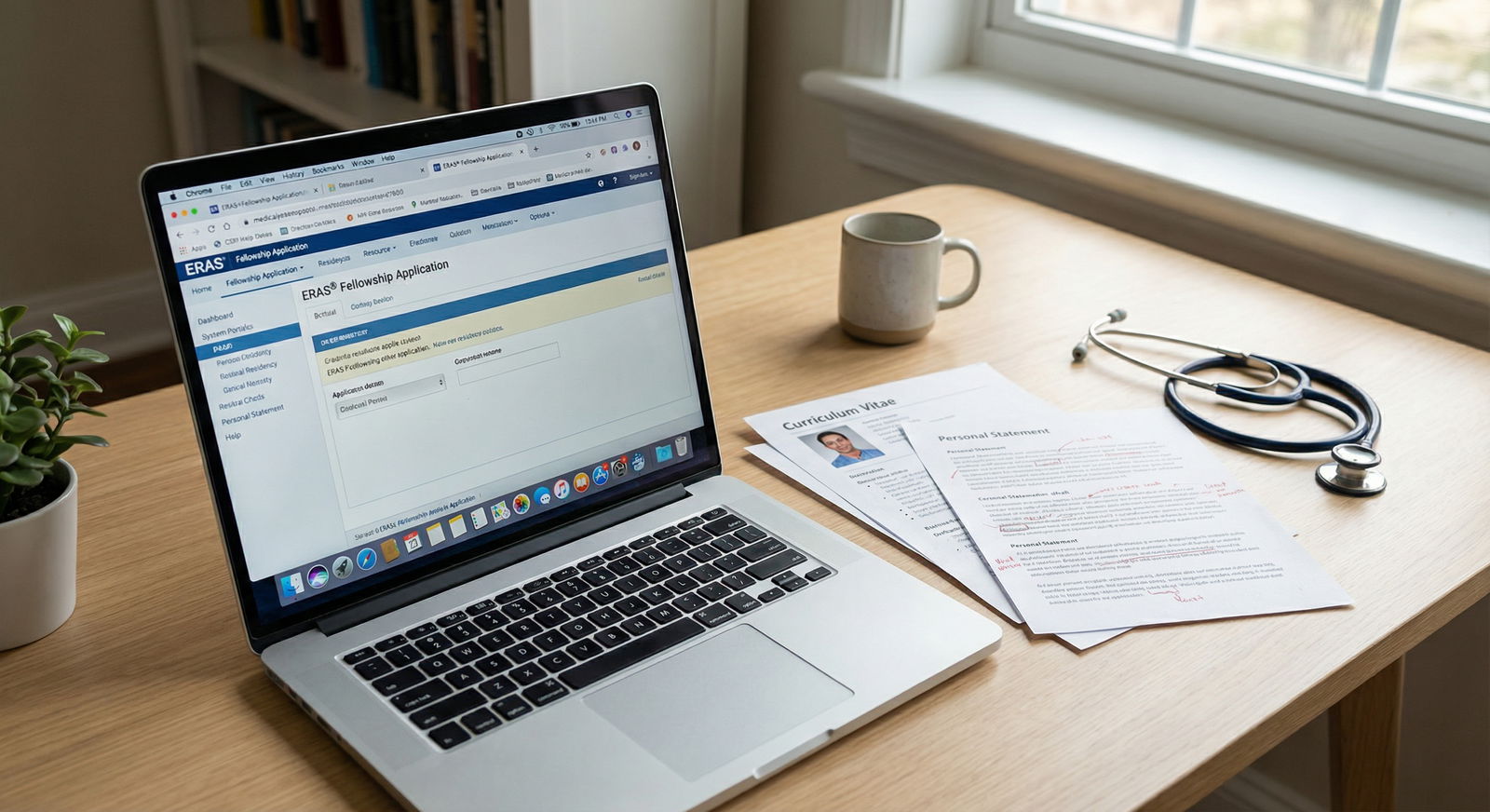
Electronic Residency Application Service (ERAS)
ERAS is the centralized platform where you:- Complete your application profile and experiences
- Upload your personal statement(s), CV (largely auto-generated from entries), and photo
- Designate which documents go to which programs
- Track which documents have been received by programs
Letters of Recommendation (LoRs)
High-quality letters can significantly strengthen your application. Strong letters:- Are written by physicians who know you well clinically
- Provide specific examples of your performance, character, and growth
- Often come from faculty in your chosen specialty (critical for many fields)
Personal Statement
Your personal statement is your narrative anchor. It should:- Explain why you chose your specialty
- Connect your experiences to your future goals
- Show insight, maturity, and self-awareness
- Complement—not repeat—your CV
Curriculum Vitae (CV)
In ERAS, your “CV” is essentially built from:- Education history
- Clinical and work experiences
- Research, presentations, and publications
- Volunteer and leadership roles
Think of it as your professional snapshot over time.
Transcripts and MSPE (Dean’s Letter)
- Medical school transcript: Documents your courses and grades.
- Medical Student Performance Evaluation (MSPE): Summarizes your performance and provides narrative evaluations. Programs rely heavily on this document.
Board Scores: USMLE/COMLEX
- USMLE Step 1 and Step 2 CK (or COMLEX Level 1/2 for DO students) remain key data points.
- Many programs use score thresholds for initial screening, especially in competitive specialties.
- For IMGs, scores often carry even more weight due to variability in training backgrounds.
Supplemental Application and Program Signaling (if applicable)
In recent cycles, ERAS has offered:- Supplemental applications for certain specialties
- Program signals: Limited “signals” to indicate highest interest in specific programs
These elements can influence interview offers and should be used strategically.
Step 1: Self-Assessment and Thoughtful Specialty Exploration
Before you can build a strong application, you need clarity about where you’re heading. Career planning is the foundation of a successful residency application strategy.
Reflecting on Your Interests and Strengths
Use your clinical rotations and experiences as data points:
Ask yourself:
- Which rotations energized me rather than drained me?
- When did I feel most engaged or “in flow”?
- Do I prefer acute care settings (ED, ICU) or continuity of care (primary care, outpatient clinics)?
- Do I thrive with procedures, complex diagnostics, long-term relationships—or a mix?
Consider your working style:
- Are you comfortable with irregular hours and high-acuity settings (e.g., surgery, EM, critical care)?
- Do you prefer team-based decision-making or more autonomy?
- How do you handle stress, uncertainty, and time pressure?
Personality and values fit:
- Lifestyle goals (call schedule, flexibility, geographic preferences)
- Long-term career plans (fellowship, academic medicine, community practice, global health)
- Need for work–life integration vs willingness to tolerate intense training for a period
Writing these reflections down can help clarify patterns and guide discussion with advisors.
Exploring Specialty Options Strategically
Once you’ve reflected on your preferences:
Research specialty characteristics:
- Competitiveness and average applicant profiles
- Length of training and typical fellowship pathways
- Lifestyle considerations (call, nights, weekends)
- Patient populations and typical clinical scenarios
Use targeted resources:
- Articles on the most competitive medical specialties (e.g., dermatology, plastic surgery, orthopedic surgery)
- Analyses of less competitive specialties or “parallel plans” (e.g., internal medicine, family medicine, psychiatry)
- AAMC Careers in Medicine, specialty societies, and program websites
Talk to people in the field:
- Residents and fellows in programs where you’ve rotated
- Faculty mentors in your home institution
- Alumni from your school who matched into your field of interest
Align your specialty choice with both your passions and a realistic reading of your academic profile (board scores, grades, clinical evaluations, research).
Step 2: Building a Strong, Cohesive Application Profile
Once you have a clearer sense of specialty direction, you can start assembling and polishing the core elements of your ERAS application.
Create a Detailed Residency Application Timeline
Backward-plan from Match Day and ERAS deadlines. A typical structure:
12–18 months before applications open (late MS2–early MS3 / early in clinical years):
- Begin specialty exploration and mentorship
- Plan core rotations and, if possible, away rotations in your target field
6–9 months before ERAS opens:
- Identify letter writers and start building relationships
- Map out any remaining board exams (e.g., Step 2 CK)
- Start drafting your CV and tracking experiences
3–5 months before ERAS submission (spring–early summer):
- Draft and revise personal statement(s)
- Confirm transcript and MSPE timelines with your school
- Decide on a preliminary program list and application strategy
1–2 months before ERAS deadline:
- Finalize and proofread ERAS entries
- Ensure LoRs, photo, transcripts, and scores are uploaded or in process
- Double-check any supplemental application requirements
Having a written timeline—ideally in a calendar or project management tool—helps you stay organized and reduces last-minute stress.
Crafting a Compelling Personal Statement
Your personal statement should function as a coherent story, not a disjointed list of achievements. Practical tips:
Start with a specific, honest moment, not a generic quote or cliché.
- Example: A formative patient encounter, a turning point rotation, or a challenge that shaped your perspective.
Show, don’t just tell.
- Instead of “I am compassionate,” describe what you did in a situation that demonstrates compassion and reflection.
Connect your experiences to the specialty.
- Explain why this specialty fits your skills, values, and long-term goals.
- Highlight clinical, research, volunteer, or leadership experiences that demonstrate alignment.
Address red flags strategically (if needed).
- Briefly and maturely discuss issues like a failed exam or leave of absence.
- Take responsibility, explain context, and focus on growth and what’s changed.
Tailor for different specialties if applying to more than one.
- Do not use a generic “one-size-fits-all” statement.
- Each version should clearly speak to that field and its culture.
Have multiple people review your statement: a trusted mentor in your specialty, someone strong in writing, and ideally an advisor who knows the Match Process.
Step 3: Securing Strong Letters of Recommendation
Letters of Recommendation are among the most influential parts of your Residency Application. They provide evidence from supervisors who have seen you in action.
Choosing the Right Recommenders
Aim for 3–4 strong letters for most specialties. Consider:
Specialty-specific letters:
- Many programs prefer or require a certain number of letters from within the specialty (e.g., 2–3 for internal medicine, 3 for surgery).
- A strong letter from your sub-internship or away rotation can carry significant weight.
Clinical supervisors over “big names” who barely know you:
- A detailed letter from a mid-level faculty who worked closely with you is more valuable than a generic letter from a famous chair who barely remembers you.
Diversity of perspective:
- Mix of inpatient, outpatient, research (if applicable), and leadership/mentorship experiences.
- For physician–scientist paths, at least one strong research letter is essential.
Preparing Your Letter Writers for Success
Make it as easy as possible for your recommenders to write you an excellent, specific letter:
Provide them with:
- Your updated CV
- A draft of your personal statement
- A summary of your work with them, including:
- Rotation dates
- Specific patients or projects you worked on together
- Any particular strengths or themes you hope they might highlight
- Clear deadlines and how to upload via ERAS
- Your ERAS AAMC ID and relevant instructions
Ask them explicitly if they feel they can write a “strong, supportive letter” for your residency application. This gives them a graceful way to decline if they cannot be enthusiastic.
Step 4: Completing and Submitting a High-Quality ERAS Application
Once your content pieces are in progress, turn to the technical and organizational aspects of your ERAS application.
Organizing and Entering Your Information Thoughtfully
Pay attention to detail—programs notice sloppiness. Key sections:
Personal and Biographical Information
- Double-check your contact information and demographic data.
- Ensure your photo is professional: neutral background, business attire, clear lighting.
Education and Training
- Enter all institutions, degrees, and dates accurately.
- Report any leaves of absence or unique circumstances truthfully (your MSPE will reflect these as well).
Experience Entries (Work, Research, Volunteer)
- Be concise but specific in your descriptions.
- Focus on impact and responsibilities, not just titles.
- Use active verbs and quantify when appropriate (e.g., “Led a team of 5 volunteers…”).
Publications, Presentations, and Posters
- Use consistent citation format.
- Clearly distinguish between published, accepted, in press, and submitted work.
- Do not exaggerate your role or contributions.
Honors and Awards
- Include academic awards, leadership recognitions, scholarships, and notable distinctions.
- Briefly explain lesser-known awards if their importance might not be obvious.
Quality Control Before Submission
Before you certify and submit:
- Read through your entire application out loud—you’ll catch errors you missed silently.
- Ask one or two trusted people to review for:
- Typos and grammar
- Clarity and consistency
- Redundant or weak entries that could be tightened
Remember: Once you certify your ERAS application, you cannot edit most sections. Take the time to get it right.
Step 5: Strategically Researching, Selecting, and Ranking Programs
The Match Process is not just about getting a spot—it’s about finding a good fit. Thoughtful program selection and ranking is a core part of smart career planning.
Researching Residency Programs Effectively
Go beyond name recognition. Consider:
Program culture and environment
- Read resident testimonials and program mission statements.
- Look for signs of support, wellness initiatives, mentorship, and DEI efforts.
- Talk to current or recent residents if possible.
Clinical training and case mix
- Volume and diversity of patients
- Balance of community vs tertiary/quaternary care
- Exposure to subspecialties and procedural opportunities
Academic and career development
- Research infrastructure, protected time, and mentorship (especially for academic careers)
- Fellowship match outcomes and faculty connections
- Opportunities for teaching medical students
Location and lifestyle
- Cost of living, commute, support systems, and personal priorities
- Availability of partner employment or family support if relevant
Create a spreadsheet or tracking tool to compare programs on factors important to you.
Building and Ranking Your Program List
Right-sizing your application volume:
- Number of programs varies by specialty and competitiveness of your application.
- Competitive fields may require broad applications; less competitive fields allow more selectivity.
- Use data from NRMP (Charting Outcomes in the Match) and guidance from advisors.
Constructing your Rank Order List (ROL):
- Rank programs based on your true preference, not where you “think” you’ll match.
- Include a reasonable safety range, especially if your application has risk factors (lower scores, visa needs, career breaks).
- Don’t rank a program where you would truly be unhappy training for several years; if matched there, you are obligated to go.
Seeking guidance:
- Meet with your dean’s office or advising office.
- Ask specialty mentors to review your list for realism and balance.
- Discuss any need for a “parallel plan” (applying to more than one specialty).
Step 6: Preparing for Residency Interviews
Interviews are your chance to transform a 2D file into a 3D impression. Whether virtual or in person, preparation can significantly influence how programs perceive you.
Interview Preparation and Practice
Know your application cold.
- Anything you listed—research, experiences, hobbies—may be fair game in questions.
- Be ready to discuss your contributions, challenges, and what you learned.
Common interview topics:
- “Tell me about yourself.”
- “Why this specialty?”
- “Why this program?”
- Difficult patient encounters or ethical dilemmas
- Strengths, weaknesses, and areas for growth
- Career goals and possible fellowships
Mock interviews:
- Practice with advisors, faculty, or peers.
- Record yourself (video) to assess body language, pace, and clarity.
- Get specific feedback and refine answers, but avoid sounding rehearsed or robotic.
Professionalism, Presence, and Follow-Up
Dress and setting (for virtual interviews):
- Professional attire, neutral background, good lighting, and reliable internet.
- Test audio and video ahead of time; have a backup plan if possible.
During the interview:
- Be punctual, attentive, and engaged.
- Prepare thoughtful questions about curriculum, mentorship, culture, and resident life.
- Be honest—programs can tell when answers are overly scripted.
After the interview:
- Take notes right away about your impressions and details (resident camaraderie, faculty vibe, call schedule).
- Send concise, genuine thank-you emails if appropriate and if not discouraged by the program.
- Use your notes when creating your Rank Order List.
Step 7: Staying Engaged and Growing During the Application Season
The residency application window can be long and anxiety-provoking. Use this time to continue building your clinical skills and professional identity.
Continue Specialty-Relevant Engagement
Clinical activities:
- Electives or sub-internships in your chosen field
- Additional exposure to patient populations you care about (e.g., underserved, global health)
Research and scholarly work:
- Complete pending projects and submit abstracts or manuscripts if feasible.
- Be ready to discuss these projects during interviews.
Service and leadership:
- Ongoing involvement in student organizations, community outreach, or advocacy.
- These experiences can reinforce your commitment to your field and to patient care.
Maintain and Expand Your Knowledge Base
Read:
- Specialty journals and guidelines
- Landmark trials and practice-changing studies
- Core textbooks or review resources relevant to your target field
This preparation:
- Helps you speak more confidently during interviews
- Smooths your transition into residency
- Signals genuine interest and initiative

Step 8: Awaiting Results, Match Day, and Post-Match Decisions
As deadlines pass and interviews wrap up, you move into the final—and often most stressful—phase of the Match Process.
Finalizing Your Rank List and Preparing for Match Week
Double-check your ROL before certification:
- Ensure every program is in your true order of preference.
- Confirm there are no accidental omissions or misordered choices.
Understand Match Week:
- Monday: You learn whether you matched (but not where).
- Monday–Thursday (if unmatched or partially matched): Participation in the Supplemental Offer and Acceptance Program (SOAP).
- Friday (Match Day): You receive your final Match result.
If you match:
- Take time to celebrate—this is a major milestone.
- Reach out to your future program as directed.
- Start planning logistics (housing, move, licensure, onboarding requirements).
If you do not match or only partially match:
- Work closely with your school’s advisors immediately.
- Understand SOAP options and timeline.
- If you remain unmatched after SOAP, begin planning a gap year strategy (research, prelim year, additional clinical experience) and reapplication approach.
Making Informed Decisions About Offers
For those with choices (e.g., multiple specialty possibilities, couples match, or post-SOAP options):
- Consider:
- Training quality and support
- Geographic and family factors
- Alignment with long-term career goals
- Your overall well-being and sustainability during training
Discuss your options with mentors who understand your values and aspirations. The “best” program on paper isn’t always the best fit for you personally.
Conclusion: Turning the Maze into a Manageable Map
The Residency Application and Match Process is inherently complex, but it becomes far less overwhelming when broken into clear, actionable steps:
- Understand the systems and timelines (ERAS, NRMP, specialty requirements).
- Engage in honest self-assessment and informed specialty exploration.
- Build a cohesive, accurate, and polished application—from personal statement to LoRs.
- Research and rank programs that align with your goals, values, and preferred training environment.
- Prepare thoroughly for interviews and continue to grow clinically and professionally.
- Approach Match Week and beyond with a plan, support, and flexibility.
This phase of your professional journey is demanding, but it’s also an opportunity to clarify your identity as a physician and intentionally shape your career path. The skills you develop in planning, self-reflection, and resilience will serve you well far beyond Match Day.
For deeper dives, explore related guides on crafting an irresistible personal statement and avoiding common mistakes in residency applications to complement this roadmap.
Residency Application FAQs
1. What is the typical timeline for the residency application and Match Process?
Most U.S. medical students follow this general timeline:
- Spring–Summer (before 4th year):
- Finalize specialty choice, identify letter writers, schedule Step 2 CK (if needed).
- September:
- ERAS opens for program review; many applicants submit early–mid September.
- October–January:
- Interview season (dates may vary by specialty and program).
- February:
- Rank Order List (ROL) certification deadline with NRMP.
- March:
- Match Week, SOAP (if applicable), and Match Day.
Exact dates vary each year—always confirm current deadlines on ERAS and NRMP websites.
2. How many Letters of Recommendation do I need, and from whom?
Most residency programs require 3–4 Letters of Recommendation:
- At least 1–2 letters from your chosen specialty (more for some competitive fields like surgery or radiology).
- Additional letters can come from:
- Sub-internship supervisors
- Research mentors (especially for academic careers)
- Core clinical clerkship directors who know you well
Always review individual program requirements; some specify the exact number and type of letters they prefer.
3. Can I apply to more than one specialty, and how should I handle that in my application?
Yes, you can apply to multiple specialties, but you should do so strategically:
- Use separate personal statements for each specialty.
- Ensure your LoRs and experiences support each specialty you apply to.
- Avoid obvious conflicts (e.g., using a very specialty-specific letter for an unrelated specialty).
- Discuss this approach with an advisor; you may need a “primary” specialty and a well-considered “parallel” option, especially if your first choice is very competitive.
Programs understand that some applicants pursue more than one pathway, but they still expect sincere, specialty-specific interest.
4. What role does the personal statement really play in my residency application?
Your personal statement won’t usually overcome major objective deficits on its own, but it can:
- Differentiate you from applicants with similar metrics
- Provide context for your journey (e.g., nontraditional background, career switch, adversity)
- Demonstrate insight, maturity, and professionalism
- Help programs assess your fit with their culture and values
Strong personal statements are focused, specific, and reflective—they add depth to your application rather than repeating your CV.
5. How can I make my residency application more competitive overall?
You can strengthen your application by:
- Maximizing clinical performance:
- Strong evaluations, honors in key rotations, meaningful sub-internships.
- Improving objective metrics where possible:
- Solid Step 2 CK/COMLEX Level 2 performance is especially important given Step 1’s pass/fail status.
- Securing strong, specific Letters of Recommendation from supervisors who know you well.
- Engaging in meaningful research or scholarly activity, particularly in competitive specialties or academic career tracks.
- Demonstrating sustained commitment to your specialty through electives, volunteer work, leadership, or advocacy.
- Presenting a polished application:
- No typos, organized experiences, coherent narrative across personal statement and CV.
By combining thoughtful planning with consistent execution, you’ll greatly improve your chances of matching into a residency program that fits both your professional goals and your personal values.






















