
Understanding Physician Salary by Specialty in Neurology
Neurology sits at a fascinating crossroads in medicine: highly cognitive, deeply diagnostic, rapidly evolving with new therapies, and increasingly procedural in some subspecialties. For residency applicants, it’s natural to ask where neurology stands in the broader landscape of doctor salary by specialty—and how your future neuro match and subspecialty decisions might shape your long‑term income.
This guide walks through the key salary concepts, compares neurology with other specialties, explains how neurology subspecialties differ in compensation, and offers practical advice on choosing a path that balances passion, lifestyle, and financial realities.
Note: All salary figures are approximate, rounded, and based on commonly cited U.S. physician compensation surveys through 2024. Individual earnings will vary by region, practice type, and experience.
1. Where Neurology Fits in the Physician Salary Landscape
When applicants talk about “physician salary by specialty,” they usually want to know: Is neurology one of the highest paid specialties? The short answer: neurology is solidly mid‑tier, with specific subspecialties trending higher—especially when procedures or call intensity are involved.
1.1 Neurology vs Other Major Specialties
Approximate average annual U.S. physician salaries (attending level, full‑time):
Primary Care / Cognitive Fields
- Family Medicine: $250k–$280k
- Internal Medicine (general): $260k–$310k
- Pediatrics: $230k–$260k
- Neurology (general): $320k–$380k
- Psychiatry: $280k–$340k
Hospital‑Based, Cognitive + Procedural
- Hospitalist (IM): $290k–$350k
- Critical Care: $380k–$450k
- Emergency Medicine: $380k–$450k
- Neurocritical Care: $380k–$460k
Procedural / Surgical Subspecialties (Highest Paid Specialties)
- Orthopedic Surgery: $600k–$800k+
- Neurosurgery: $700k–900k+
- Cardiology (interventional): $600k–$800k
- Gastroenterology (advanced): $550k–750k
- Dermatology: $450k–650k
- Radiology (diagnostic): $450k–600k
- Anesthesiology: $420k–550k
Placed against this backdrop, neurology:
- Typically earns more than pediatrics, family medicine, general internal medicine, and psychiatry.
- Trails the highest paid specialties that are heavily procedural or surgical.
- Falls into what many surveys label as the upper-mid tier of physician compensation.
1.2 Neurology Salary Trajectory: Resident to Attending
Residency salary is relatively uniform across specialties:
- PGY‑1: $60k–$68k
- PGY‑2: $63k–$72k
- PGY‑3: $66k–$75k
- PGY‑4: $69k–$78k (for programs with a 4th year, as in neurology)
Neurology residents do not earn more than other residents in most institutions; salary is set by training year rather than specialty.
After training, neurology salary growth typically follows:
- Early career (0–3 years out): $270k–$330k (general outpatient neurology, academic settings may be lower)
- Mid‑career (5–10 years): $320k–$400k (with productivity incentives, partnership tracks, or leadership roles)
- Late career (10+ years): $350k–$450k+ (especially in private practice, high‑demand regions, or in neurocritical/stroke leadership roles)
1.3 Academic vs Private Practice Neurology
Compensation varies markedly by setting:
Academic Neurology (university hospitals)
- Base: ~$230k–$320k, with variation by subspecialty and rank (assistant vs associate vs full professor).
- Total compensation may include:
- Teaching stipends
- Admin stipends (e.g., clerkship director)
- Research grants (protected time may reduce clinical productivity)
- Trade‑off: Lower base salary but more academic prestige, research opportunities, and often more predictable hours in some divisions.
Private Practice / Large Multi‑Specialty Groups
- Base: ~$300k–$380k plus productivity incentives (RVU or collections based).
- Potential to reach $400k+ with:
- High volume outpatient clinics
- Procedure‑heavy practices (e.g., Botox, EMG, EEG interpretation, sleep studies)
- Partnership or ownership stakes.
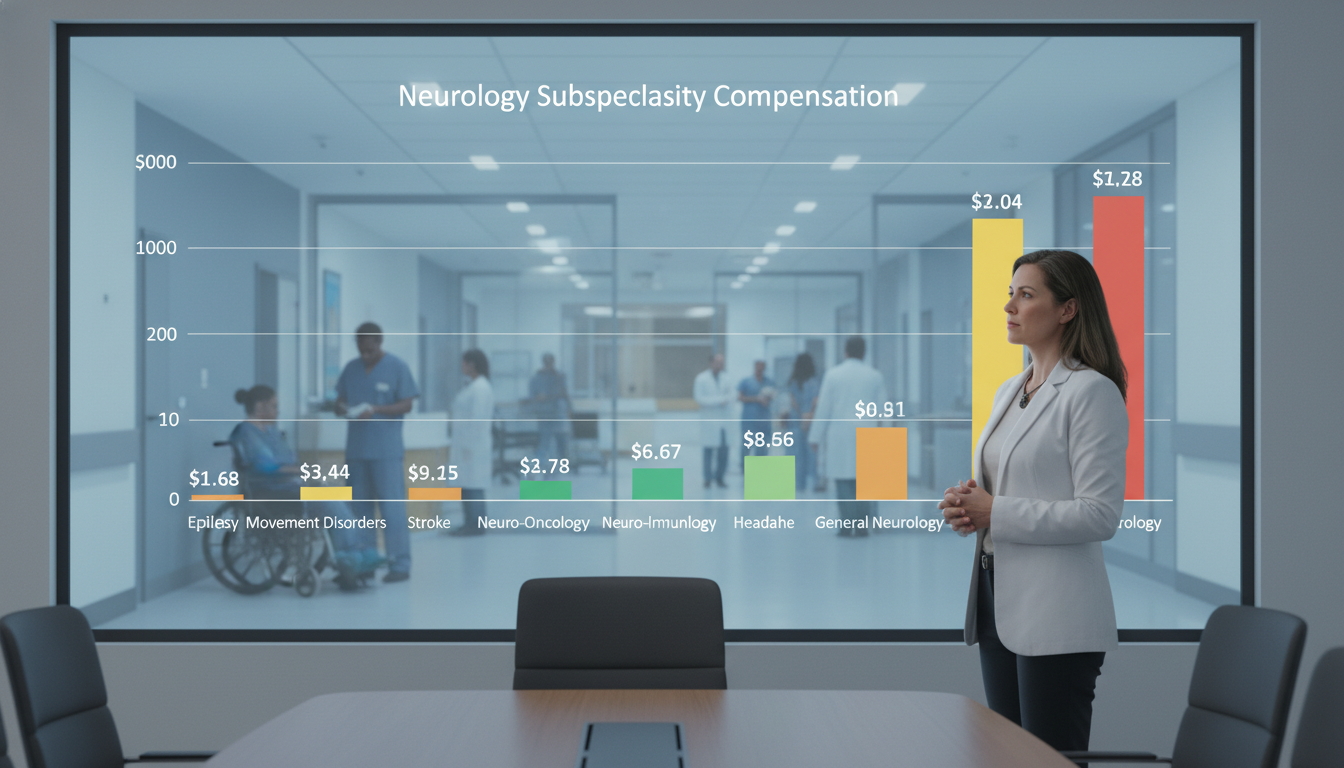
2. Neurology Subspecialties: Salary Breakdown
Within neurology, subspecialization plays a major role in your eventual doctor salary by specialty. Several niches incorporate procedures, call stipends, and ICU work that push compensation higher.
The ranges below are typical attending‑level total compensation (base + incentives) in the U.S.:
2.1 General Adult Neurology
- Approximate range: $300k–$380k
- Practice: Outpatient heavy, common diagnoses (headache, neuropathy, epilepsy, dementia, movement disorders), occasional inpatient consults.
- Key income drivers:
- High clinic volume (15–20+ patients/day)
- Ancillary testing (EMG/NCS, EEG, ultrasound, neuropsych referrals)
- Call coverage pay in some systems
General neurology is a solid benchmark for neurology residency graduates who do not pursue fellowship, or who practice a mix of subspecialty and general neurology.
2.2 Vascular Neurology / Stroke
- Approximate range: $340k–$430k
- Typical training: 1‑year vascular neurology fellowship after neurology residency.
- Practice mix:
- Inpatient stroke service
- Tele‑stroke coverage
- Neuro ICU collaboration
- Some outpatient stroke clinic
- Why higher paid?
- High call burden and urgency (stroke codes)
- Tele‑stroke contracts with multiple hospitals
- Key role in stroke programs and quality metrics
Vascular neurologists often receive additional income from medical directorships for stroke centers and from telemedicine arrangements that pay per shift or per consult.
2.3 Neurocritical Care
- Approximate range: $380k–$460k (sometimes higher with intense schedules)
- Typical training: 2‑year neurocritical care fellowship.
- Practice:
- Neuro‑ICU attending (24/7 coverage model)
- Management of severe stroke, traumatic brain injury, status epilepticus, post‑op neurosurgical cases.
- Compensation drivers:
- Shift work and nights
- ICU billing complexity
- High‑acuity care
- Medical director roles for neuro‑ICUs
Neurocritical care is often among the best‑compensated neurology subspecialties, reflecting intensity, burnout risk, and 24/7 coverage expectations.
2.4 Epilepsy / Clinical Neurophysiology
- Approximate range: $330k–$420k
- Typical training: 1‑year epilepsy or clinical neurophysiology fellowship.
- Practice:
- EEG reading, video EEG monitoring
- Seizure management, pre‑surgical evaluation
- In academic centers, participation in epilepsy surgery programs
- Income opportunities:
- High volume EEG interpretation
- EMG/NCS if trained in neuromuscular as well
- Intraoperative neurophysiologic monitoring (IONM) in some settings
Those who build a practice around neurophysiology services (EEG, EMG, IONM) can significantly augment income beyond standard clinic visits.
2.5 Movement Disorders
- Approximate range: $320k–$400k
- Typical training: 1‑ or 2‑year movement disorders fellowship.
- Practice:
- Parkinson’s disease, dystonia, tremor, ataxia, Huntington’s disease
- Deep brain stimulation (DBS) programming
- Botulinum toxin injections for dystonia, spasticity
- Why potentially lucrative?
- Procedural revenue from DBS programming, Botox
- Long‑term, high‑complexity patients (higher RVU visits)
Movement disorders can be quite rewarding financially if the practice incorporates procedures; a purely cognitive clinic without procedures may align closer to general neurology compensation.
2.6 Neuromuscular Medicine
- Approximate range: $330k–$420k
- Typical training: 1‑year neuromuscular fellowship, often with heavy EMG focus.
- Practice:
- EMG/NCS studies (major revenue component)
- Myasthenia gravis, ALS, neuropathies, myopathies
- Multidisciplinary ALS or neuromuscular clinics
- Income drivers:
- High EMG volume
- Ability to contract with community hospitals for EMG services
- Procedural focus
Because EMG/NCS generates significant RVUs, neuromuscular neurologists in busy practices often out‑earn general neurologists.
2.7 Headache Medicine
- Approximate range: $310k–$390k
- Typical training: 1‑year headache fellowship.
- Practice:
- Chronic migraine, tension‑type headache, trigeminal autonomic cephalalgias
- Botox for chronic migraine
- Nerve blocks, trigger point injections
- Income factors:
- High patient volumes
- Procedural interventions (Botox, nerve blocks)
- Infusion center services for refractory cases in some systems
Headache medicine has seen growth alongside new CGRP therapies and devices, with opportunities in infusion centers and specialized headache clinics.
2.8 Sleep Medicine (for Neurologists)
- Approximate range: $320k–$410k
- Typical training: 1‑year sleep medicine fellowship (often open to pulmonology, psychiatry, ENT, pediatrics as well).
- Practice:
- Sleep clinic (OSA, narcolepsy, insomnia)
- Polysomnography interpretation
- Management of CPAP/BiPAP titration
- Compensation drivers:
- Sleep study interpretation volume
- Multiple practice sites (sleep labs, outpatient clinics)
- Growing demand in community settings
Sleep can be especially lucrative when you read a large number of studies or serve as medical director of sleep labs in multiple hospitals.
3. What Really Influences Neurology Salary?
While subspecialty is important, several cross‑cutting factors often influence your final doctor salary by specialty even more—especially in neurology.
3.1 Practice Setting and Ownership
- Hospital‑employed neurology
- Stable base salary, robust benefits
- Quality‑based bonuses, RVU incentives
- Less direct financial risk; minimal overhead responsibilities
- Private practice / group practice
- Potentially higher ceiling via:
- Partnership
- Profit‑sharing from ancillary services (EEG, EMG, imaging, infusion)
- More administrative responsibility and financial risk
- Potentially higher ceiling via:
- Hybrid models
- Large multi‑specialty groups aligned with hospitals
- Combining academic appointments with community practice
Ownership in an imaging center, EMG lab, or infusion center can significantly boost income for established neurologists, especially in the community.
3.2 Geographic Region and Local Market
Location can alter physician salary by specialty more than 20–30%:
- Higher pay, often with lower cost of living:
- Rural or semi‑rural Midwest, South, some Mountain states
- Underserved regions with strong recruitment incentives
- Moderate pay, moderate to high cost of living:
- Suburban settings, mid‑sized cities
- Lower relative pay, very high cost of living:
- Coastal metros (San Francisco, NYC, Boston, Seattle, LA)
- Academic‑heavy cities with high physician density
A neurology attending in a midwestern town might earn $400k+ with a low mortgage and short commute, while a peer in a coastal academic center may earn $275k–$320k but gain academic prestige and research opportunities.
3.3 Workload, Call, and Schedule Design
- Clinic volume: More patients and more complex visits generate more RVUs.
- Procedures: EMG, EEG, DBS programming, Botox, nerve blocks, sleep studies, and IONM add substantial revenue.
- Call coverage:
- Inpatient call stipends (overnight pager, stroke call)
- Tele‑stroke consults (per‑shift or per‑consult payment)
- Shift work: Neurocritical care and teleneurology may pay more per hour but concentrate work into intense blocks, with burnout considerations.
Physicians seeking the highest paid specialties within neurology often accept more call, ICU work, or tele‑stroke coverage in exchange for higher compensation.
3.4 Academic Rank and Leadership Roles
In academic neurology, salaries typically scale with:
- Rank: Assistant < Associate < Full Professor.
- Division / program leadership:
- Stroke director
- Program director (residency or fellowship)
- Department vice chair or chair
- Protected time vs. clinical productivity:
- More protected research or administration time usually means lower RVU‑based bonuses but may increase long‑term career sustainability and grant‑based income.

4. Planning Your Career: Matching into Neurology with Salary in Mind
If you’re at the neurology residency application or early training stage, it’s wise to understand salary trends—but not let compensation be the only factor.
4.1 During the Neuro Match: What to Look For
When ranking programs in the neurology residency match, consider how each program sets you up for both clinical competence and career flexibility:
Subspecialty exposure:
- Do you have robust rotations in stroke, epilepsy, neurocritical care, movement, neuromuscular, sleep, and headache?
- Are there fellows in these subspecialties, and do they enhance or limit your hands‑on experience?
Procedure opportunities:
- EMG/EEG exposure
- Lumbar punctures
- Botulinum toxin injections
- DBS programming
- Sleep studies
Research and mentorship:
- Are there mentors doing clinical trials or health services research in high‑impact areas (stroke, epilepsy, neurodegeneration)?
- Can you build a CV strong enough for competitive fellowships?
Program outcomes:
- Where do graduates go?
- Do alumni match into strong fellowships or secure desirable private practice positions?
Programs that emphasize broad skill development and subspecialty options give you more levers to pull later when it comes to optimizing your income and lifestyle.
4.2 Choosing a Fellowship with Financial and Lifestyle Awareness
Subspecialty choice affects both your quality of life and your place in the physician salary by specialty hierarchy. Some frameworks to consider:
Intensity vs income:
- Higher intensity & call: neurocritical care, vascular neurology with heavy telestroke.
- Moderate intensity, procedural: epilepsy (EEG), neuromuscular (EMG), movement disorders (DBS/Botox), sleep.
- Lower intensity (variable): some headache or predominantly outpatient subspecialty practices with minimal call.
Location flexibility:
- Subspecialties like stroke, epilepsy, and sleep are in demand in both academic and community settings nationwide.
- Highly niche subspecialties may cluster in academic centers, where salaries can be modest.
Burnout and sustainability:
- Consider whether you can maintain high‑intensity neuro‑ICU or 24/7 stroke coverage long term.
- Some neurologists transition over time from high‑call roles (neuro‑ICU) to more clinic‑based roles (headache, movement, general).
4.3 Negotiating Your First Neurology Contract
When you complete training, understanding the drivers of neurology compensation will help you evaluate offers:
Key elements to review:
Base salary vs RVU target:
- Is the base realistic for a new graduate?
- What’s the expected timeline to reach bonus thresholds?
Call schedule and compensation:
- Is call mandatory?
- Are there separate stipends or built‑in RVUs for call and telestroke work?
Sign‑on bonuses and loan repayment:
- Common in rural or underserved areas; can make a large impact early in your career.
Partnership track (private practice):
- Timeline (2–4 years is common)
- Buy‑in terms
- Access to ancillary revenue streams (EMG lab, EEG services, infusion suite, imaging)
Non‑compete clauses:
- Can strongly affect your flexibility if you want to switch jobs within a region.
Having mentors (especially recent graduates) review your contract can protect you from common pitfalls and help you maximize both compensation and job satisfaction.
5. Neurology in the Context of the Highest Paid Specialties
For applicants who track “highest paid specialties” lists and wonder whether neurology is “worth it” financially, it helps to place neurology in context.
5.1 Neurology vs Procedural Giants
Compared to orthopedic surgery, neurosurgery, interventional cardiology, and GI, neurology:
- Requires similar or shorter total training time (4 years neurology residency + 1–2 years fellowship vs 7+ years including surgical residencies).
- Has lower malpractice premiums on average compared to high‑risk surgical specialties.
- Offers greater flexibility in late career (e.g., tele‑neurology, outpatient‑only practice, partial retirement).
However, neurology:
- Is primarily cognitive, so RVU generation per encounter is often lower than for procedures.
- Has fewer high‑reimbursement procedures than surgical fields.
5.2 Neurology vs Other Cognitive Specialties
Within cognitive and internal medicine–based specialties, neurology is relatively favorable:
- Generally higher pay than general internal medicine, family medicine, and pediatrics.
- Often comparable or higher than psychiatry, depending on region and subspecialty.
- Approaches or exceeds many hospitalist roles, depending on subspecialty and practice type.
This makes neurology attractive for applicants who prefer complex diagnostics over procedures but still want above‑average income among non‑surgical specialties.
5.3 Long‑Term Financial Strategy for Neurologists
Even if neurology is not at the very top of the doctor salary by specialty rankings, neurologists can build strong long‑term financial security by:
- Choosing a practice environment with favorable cost‑of‑living vs salary ratio.
- Developing a niche (e.g., EMG, EEG, DBS, headache procedures, tele‑stroke).
- Negotiating smartly on call pay, admin roles, and productivity incentives.
- Managing lifestyle inflation early in practice to pay down loans and build savings.
- Using flexible work models (tele‑neurology, part‑time outpatient) later in career to sustain income while reducing burnout.
6. Key Takeaways for Neurology Residency Applicants
- Neurology sits in the upper‑mid range of U.S. physician salaries—higher than many primary care fields, lower than the highest paid procedural and surgical specialties.
- Subspecialty choice significantly shapes income:
- Neurocritical care, tele‑stroke–heavy vascular neurology, and neurophysiology‑based practices (EMG/EEG) are often at the top of the neurology earnings spectrum.
- Practice setting, geographic region, call burden, and procedural mix may ultimately matter more than the name of your subspecialty alone.
- During the neuro match, prioritize programs that offer:
- Strong subspecialty exposure
- Robust procedural training
- Mentorship and clear fellowships outcomes
- Think of income as one factor among many. The best careers in neurology balance:
- Intellectual fit and passion for the patient population
- Sustainable workload and call expectations
- Fair compensation within your chosen setting
Neurology offers a compelling combination of cognitive challenge, impactful patient care, and solid earning potential—especially when you make strategic choices throughout training and early practice.
FAQ: Physician Salary by Specialty in Neurology
1. Is neurology considered a high‑paying specialty?
Neurology is generally mid to upper‑mid in the physician salary spectrum. It usually pays more than primary care fields (internal medicine, pediatrics, family medicine) and is competitive with or higher than psychiatry, but it typically pays less than highly procedural or surgical specialties like orthopedics, neurosurgery, interventional cardiology, and gastroenterology.
2. Which neurology subspecialties tend to earn the most?
Among neurology fields, neurocritical care and vascular neurology with substantial telestroke or ICU work are often at the top, followed by subspecialties with heavy procedure or study interpretation volume (epilepsy/clinical neurophysiology, neuromuscular/EMG, sleep medicine). Movement disorders and headache can also be well compensated when they incorporate procedures such as DBS programming, Botox, and nerve blocks.
3. Does doing a fellowship always increase neurology salary?
Not always, but often. Fellowships that add marketable procedural or ICU skills (neuro‑ICU, stroke, EMG/EEG, sleep) tend to increase your value in both academic and community settings. However, some fellowships may steer you toward academic roles with lower base salaries but more research time. The impact on salary depends on how you use your subspecialty skills and where you practice.
4. How much does location affect neurology compensation?
Location can change neurology income by 20–30% or more. Neurologists in rural or underserved areas, often in the Midwest or South, may earn significantly higher salaries (plus bonuses and loan repayment) compared with peers in coastal academic cities. When evaluating offers, consider both the absolute salary and the cost of living to understand your real purchasing power.






















