
Understanding Urology and Why Early Preparation Matters
Urology is a surgical specialty that focuses on the urinary tract of both men and women and the male reproductive system. It combines elements of surgery, medicine, oncology, radiology, and even aspects of women’s health and pediatrics. Because of this breadth, early, focused preparation during your premed years can significantly strengthen your path toward a urology residency and a successful urology match.
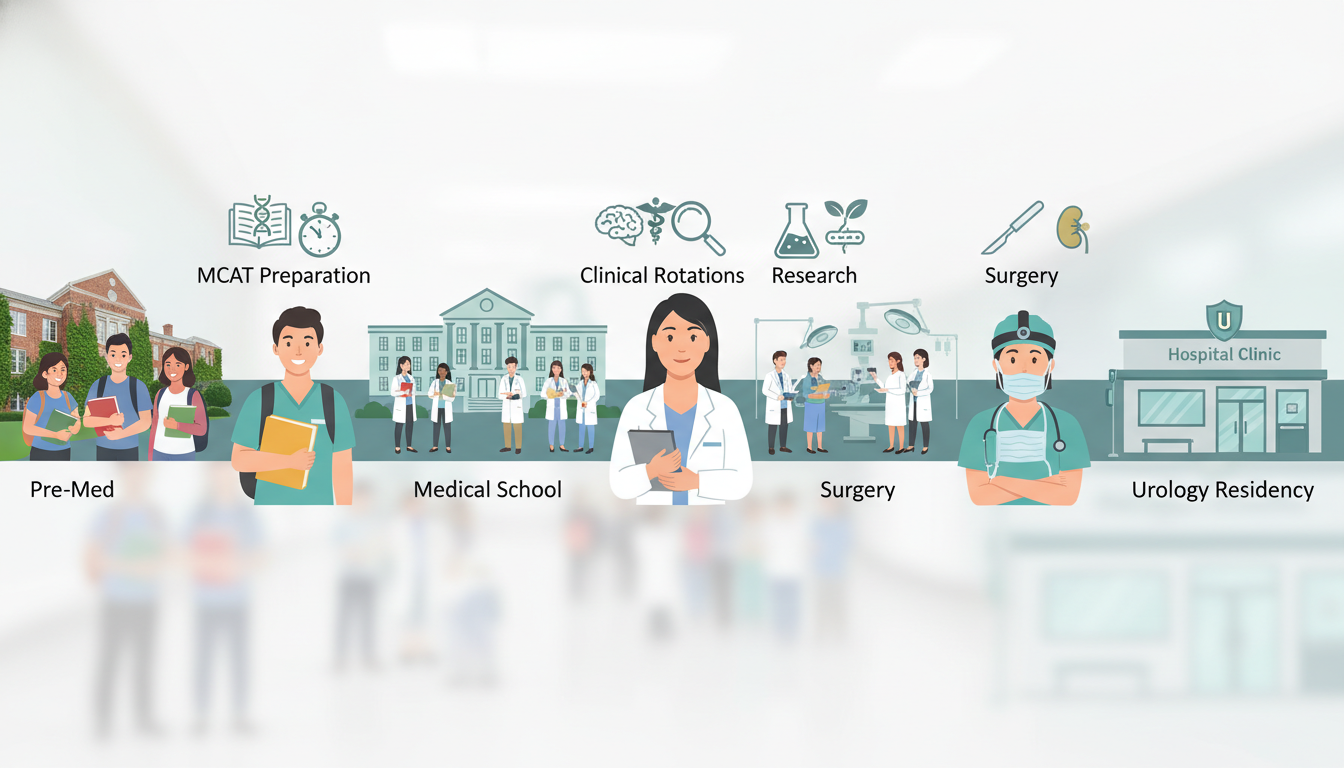
Before you ever submit a residency application, you must complete a long sequence of steps: premed coursework, MCAT, medical school, USMLEs/COMLEX, clinical rotations, and urology-specific experiences. Strategic planning in college—well before medical school—saves time, opens doors, and sets you up for a competitive application.
This guide is designed for premeds who think they might be interested in urology, students who want strong premed advice regardless of final specialty, and anyone asking “how to become a doctor” with a potential focus in urology. We’ll walk through what to do in college, how to explore urology meaningfully, and how to position yourself for a strong future urology residency application.
Core Premed Foundations: Academics, MCAT, and Requirements
Even if you are already sure you love urology, you still need to clear the same core hurdles as any doctor in training. That means meeting premed requirements, excelling academically, and performing well on the MCAT.
Essential Premed Coursework
Most medical schools don’t require you to major in biology, but they do require a strong foundation in basic science. Typical premed requirements include:
- Biology with lab (1–2 years)
- General chemistry with lab (1 year)
- Organic chemistry with lab (1 year)
- Physics with lab (1 year)
- Biochemistry (1 semester, sometimes more)
- English/writing-intensive courses
- Statistics and/or calculus
- Psychology and sociology (strongly recommended for MCAT)
- Humanities/social sciences (for holistic education and communication skills)
For someone interested in a surgical field like urology, it’s wise to build an even deeper science background:
- Anatomy and physiology – directly relevant to urologic anatomy and pelvic surgery.
- Cell biology and molecular biology – useful if you later participate in urologic oncology research.
- Genetics – increasingly important for hereditary urologic cancers and infertility.
- Immunology or microbiology – helpful for infectious complications, prostatitis, and post-op care.
You can major in anything as long as you complete premed requirements. Some urologists majored in engineering, psychology, or even philosophy. What matters is:
- You meet each school’s science prerequisites.
- You show intellectual curiosity and rigor.
- You maintain a strong GPA (especially in the sciences).
Actionable tip:
Early in college (ideally first year), download the prerequisite charts from 5–10 medical schools you could realistically apply to later. Plan your 4-year schedule so you’re never scrambling to fit requirements at the last minute.
Building a Competitive GPA
Urology residency is considered competitive. Most successful urology applicants were high performers during medical school—and those habits begin in college.
A few GPA strategies:
- Aim for ≥3.7 overall and science GPA if possible. Many strong applicants will be in this range.
- If you struggle with early courses, course-correct quickly:
- Use office hours and tutoring services.
- Adjust your study methods (active recall, spaced repetition).
- Reduce extracurricular overload during heavy science semesters.
- Take advanced courses only when you can realistically excel. An “easier” A often helps more than an “impressive” C.
Think of your GPA as part of a long-term narrative: you want admissions committees—and later residency directors—to see that you can handle rigorous medical content.
MCAT Strategy with a Future Surgical Career in Mind
While the MCAT doesn’t test urology directly, a strong MCAT score helps ensure you get into a good medical school, which then affects your training environment and potential research opportunities.
Key MCAT domains:
- Chemical and Physical Foundations – overlaps with physiology and pharmacology.
- Biological and Biochemical Foundations – core for any physician.
- Psychological, Social, and Biological Foundations – prepares you for the behavioral aspects of patient care (essential when discussing sensitive topics like sexual health or incontinence).
- Critical Analysis and Reasoning Skills (CARS) – vital for clinical reasoning and communication.
Actionable MCAT approach:
- Choose a test date that allows:
- Completion of core prerequisites.
- 3–4 months of dedicated, consistent study.
- Consider structured prep (course, tutoring, or self-study with high-quality resources).
- Build stamina with full-length practice exams every 1–2 weeks as the test approaches.
You don’t need a specific MCAT score to pursue urology; you need a strong enough score to get into medical school where you can thrive. For many allopathic (MD) schools, this may mean aiming for around the 512+ range, but there is wide variability. Always interpret target scores in the context of your GPA and school list.
Exploring Urology as a Premed: Early Clinical and Shadowing Experiences
You can’t commit to a field you’ve never seen. Thoughtful early exposure to urology helps you decide if it’s the right path and builds a story you can carry through your medical school and residency applications.
What Urologists Actually Do
Urology spans multiple patient populations and clinical scenarios:
- Men’s health and sexual medicine – erectile dysfunction, infertility, low testosterone.
- Oncology – prostate, bladder, kidney, testicular cancers.
- Stone disease – kidney and ureteral stones, often treated endoscopically.
- Reconstructive urology – urethral stricture disease, trauma, congenital anomalies.
- Female pelvic medicine – incontinence, pelvic organ prolapse (often overlapping with urogynecology).
- Pediatrics – congenital urinary tract abnormalities, undescended testes, vesicoureteral reflux.
- Minimally invasive and robotic surgery – laparoscopic or robotic nephrectomies, prostatectomies, and more.
This blend of clinic and OR time, long-term patient relationships, and life-altering interventions makes urology appealing to many.
Shadowing Urologists as a Premed
Shadowing is one of the most accessible ways for premeds to explore urology.
How to find urology shadowing opportunities:
- Ask your university’s pre-health advising office for physician contacts.
- Reach out to academic medical centers or large hospital systems in your city.
- Ask family doctors or other specialists you know if they can connect you with a urologist.
- If there’s a urology residency program nearby, check the department website for medical student or premed outreach contacts.
How to frame your request (brief email example):
Dear Dr. [Name],
I am a pre-med student at [University], interested in exploring surgical specialties and particularly curious about urology. I am hoping to learn more about the day-to-day work, patient care, and training path in your field. Would you be open to allowing me to shadow you in clinic or the operating room for a short period, if permitted by hospital policy?
Thank you for your time and consideration.
Sincerely,
[Your Name]
What to pay attention to while shadowing:
- How the urologist talks about sensitive topics (sexual function, urinary incontinence).
- The balance between clinic visits vs. procedural and OR time.
- The emotional aspects: delivering cancer diagnoses, discussing fertility, managing chronic pain.
- The team structure: residents, physician assistants, nurses, anesthesiologists.
Afterward, reflect in writing—what energized you? What surprised you? These reflections later become powerful material for personal statements and interview answers.
Clinical Volunteering that Aligns with Urologic Interests
Not all your clinical exposure must be in urology, and it often cannot be at the premed stage. However, you can choose experiences that relate well to urologic themes:
- Hospital volunteering on surgical floors or in perioperative areas.
- Nursing home or long-term care volunteering, where you’ll often see urinary issues, catheters, and incontinence.
- Men’s health or primary care clinics, where prostate issues, ED, or urinary symptoms are common.
- Cancer centers, especially if they see genitourinary (GU) malignancies.
Actionable advice:
Aim for consistent clinical exposure over a long period (e.g., 3–4 hours per week over a year) rather than a short, intense block. Consistency shows commitment and helps you build meaningful patient-centered stories.

Building a Urology-Relevant Extracurricular Profile as a Premed
You do not need to “brand” yourself as a urologist at age 19. However, you can choose activities that build transferable skills and show a budding interest in surgery and patient-centered care.
Research: Is Urology-Specific Research Necessary in College?
Urology-specific research is rarely required at the premed stage, but research experience in any rigorous biomedical or clinical area can be helpful, especially if:
- You enjoy asking scientific questions.
- You’re considering academic medicine or future fellowship training.
- You want to be comfortable in research environments during medical school.
Types of research that fit well with a future in urology:
- Oncology research (e.g., cancer biology, immunotherapy).
- Health services or outcomes research (e.g., disparities in surgical care access).
- Biomechanics or biomedical engineering (e.g., device development, imaging).
- Basic science in cell biology, regenerative medicine, or genetics.
If you’re lucky enough to be near a urology department that accepts undergraduates, urology-focused projects can be ideal, but they’re not mandatory.
How to get started:
- Check your university’s research portal or “undergraduate research” office.
- Read faculty profiles in departments like:
- Urology
- Surgery
- Oncology
- Biomedical engineering
- Email potential mentors with:
- A short introduction and your academic background.
- Why you’re interested in their work.
- Your availability and willingness to learn.
Service, Leadership, and Communication Skills
Urologists must discuss intimate and sometimes embarrassing topics with empathy and clarity. Experiences that build communication skills and comfort with sensitive issues are invaluable:
- Peer counseling or health education roles.
- Sexual health education programs on campus.
- Leadership positions in premed clubs or community organizations.
- Tutoring or teaching assistant roles, which strengthen your ability to explain complex ideas clearly.
These activities also strengthen your medical school application generally and prepare you for the patient-centered aspects of urology.
Technical Skills and Hands-On Exposure
No one expects you to be surgically skilled before medical school. However, certain hobbies and experiences can signal or build comfort with the hands-on, technical nature of urology:
- Working with your hands: art, music, crafts, robotics, or electronics.
- Basic clinical skills classes or EMT certification.
- Shadowing in OR-based specialties beyond urology (general surgery, orthopedics).
These activities are not premed requirements, but they can help you confirm you enjoy procedural work—a central part of urology.
Premed Planning with the Urology Match in Mind
Even though the urology match is years away during your premed phase, understanding its contours helps you make informed decisions about medical school selection and your long-term preparation.
Brief Overview: The Urology Residency Pathway
The typical training sequence:
- 4 years of college (premed phase, your current stage).
- 4 years of medical school (MD or DO).
- Urology residency:
- Usually 5–6 years total, depending on the program.
- Includes 1 year of general surgery or surgical internship, followed by dedicated urology years.
- Optional fellowship (1–2 years) in:
- Urologic oncology
- Pediatric urology
- Female pelvic medicine and reconstructive surgery
- Endourology / minimally invasive surgery
- Male infertility/andrology
- Others
The urology match is separate from the main NRMP match and has its own timeline (run by the AUA/SAU). It is competitive, with fewer spots than many other specialties.
Choosing a Medical School with a Future in Urology in Mind
When you think about how to become a doctor with the goal of entering urology residency later, your choice of medical school can matter.
Factors to consider:
- Presence of a urology department and residency program
- Offers early exposure, mentorship, and research options.
- Strength of surgical training
- OR exposure, surgical skills curriculum, simulation centers.
- Research infrastructure
- Availability of urology or oncology research for medical students.
- Student performance indicators
- Match lists: Do students match into surgical fields and urology?
- Support for competitive specialties (advising, mock interviews).
You don’t have to attend a “top 10” institution to match into urology, but you should aim for a school where motivated students regularly match into competitive specialties and have access to strong mentors.
Developing a Long-Range Timeline from Premed to Urology Match
Premed years (college):
- Complete premed requirements with strong GPA.
- Prepare for and take the MCAT.
- Gain meaningful clinical experience and basic exposure to urology.
- Participate in some research or scholarly activity if possible.
- Apply to a range of medical schools where surgical specialties are supported.
Medical school years:
- M1–M2: Academic excellence, early urology interest groups, maybe urology research.
- M3: Excel in core clinical clerkships, especially surgery; complete urology elective(s).
- M3–M4: Sub-internships (sub-Is) or away rotations in urology, Step/COMLEX performance, letters of recommendation.
- M4: Apply to urology residency through the AUA match, interview, then match.
Understanding this pathway now helps you reverse engineer your choices today: preparing strong academic habits and time management skills in college will pay dividends when the stakes are higher.
Practical Step-by-Step Plan: From Freshman Year to Medical School Matriculation
To bring this all together, here is a structured plan you can adapt to your own situation.
First Year (Freshman)
Goals:
- Confirm interest in medicine generally.
- Lay academic foundations.
- Begin light clinical exposure.
Action items:
- Meet with a premed advisor to map out premed requirements.
- Enroll in foundational courses: general chemistry, biology, or another appropriate starting point depending on placement.
- Join a premed organization and attend events featuring physicians or surgeons.
- Start volunteering 2–4 hours per week in a clinical setting (hospital, clinic, or nursing home).
- Shadow any physician you can (family doctor, internist) just to confirm you enjoy clinical environments.
If possible, start exploring what urology is—read about it, watch educational videos, or attend any local specialty talks.
Second Year (Sophomore)
Goals:
- Solidify your medical career decision.
- Begin targeted exploration of urology.
- Prepare for research and MCAT planning.
Action items:
- Continue core science sequence (organic chemistry, biology, physics as appropriate).
- Upgrade your study strategies to maintain or raise your GPA.
- Seek research opportunities—they don’t have to be in urology yet.
- Try to arrange at least one shadowing experience with a urologist to see real-world practice.
- Draft a rough timeline for MCAT (usually late sophomore or junior year).
Use this year to ask yourself: Do I feel drawn toward surgery and procedural work? If yes, urology remains a strong possible fit.
Third Year (Junior)
Goals:
- Cement your overall medical school application strength.
- Deepen clinical experience.
- Take the MCAT.
Action items:
- Complete any remaining premed requirements.
- Dedicate focused time (3–4 months) for MCAT preparation and testing.
- Increase responsibility in research or clinical roles if possible (e.g., independent project, leadership).
- If you enjoyed prior urology exposure, try to expand it:
- More shadowing with the same or additional urologists.
- Consider a short-term project or quality improvement initiative if your mentor is open to it.
- Keep detailed notes on meaningful patient and physician interactions for future essays.
By the end of this year, you should feel confident in your choice to apply to medical school and have at least some concrete exposure to surgical or urologic practice.
Fourth Year (Senior)
Goals:
- Finish strong academically.
- Apply and commit to a medical school.
- Reflect on your evolving interest in urology.
Action items:
- Complete any leftover coursework, especially upper-level sciences that interest you.
- Use your application materials (personal statement, secondary essays) to show:
- Genuine interest in medicine and patient care.
- Curiosity about specialties like urology without seeming prematurely committed.
- Once accepted, research if your future medical school has a urology interest group or robust surgical mentorship programs.
- Continue clinical or service work until you transition to medical school; avoid “checking out” academically after acceptances.
By matriculation, you won’t be a urologist (or even a medical student urologist), but you’ll have a solid academic record, meaningful clinical experiences, and an informed curiosity about urology—exactly where you need to be.
Frequently Asked Questions (FAQ)
1. Do I need to decide on urology during college to match into a urology residency later?
No. Many future urologists decide during medical school, often after core surgical rotations. However, early awareness helps you maximize relevant experiences and ensure you attend a medical school with good surgical and urology exposure. The most important premed priorities remain: strong academics, MCAT, and genuine clinical engagement.
2. Is urology too competitive to consider if my GPA or MCAT isn’t perfect?
Urology is competitive, but applicants are evaluated holistically. You can compensate for slightly lower numbers with outstanding clinical performance, strong letters, research, and evidence of dedication to the field. At the premed level, focus on improvement and trend—if your early grades were lower but you show sustained upward momentum, admissions committees and future residency directors often view that favorably.
3. Do I have to do urology research specifically as a premed to go into urology?
No. Urology-specific research is not required during college. Any solid research experience (oncology, surgical outcomes, biomedical engineering, etc.) teaches you critical thinking and scientific reasoning. You’ll have more targeted opportunities for urology research in medical school, especially at institutions with active urology departments.
4. As a premed, how do I talk about urology in my medical school application without sounding too narrow?
You can say that you are interested in surgical or procedure-based specialties and that experiences like shadowing a urologist helped you appreciate the combination of surgery, long-term relationships, and sensitive patient communication. Emphasize that you are open to exploring all fields in medical school, but that these experiences gave you insight into the diversity of medical careers. This shows maturity and curiosity rather than rigidity.
By approaching your premed years with intention—balancing strong academics, meaningful clinical time, and thoughtful exploration of fields like urology—you not only prepare yourself for medical school, but also position yourself for a potential future in one of the most dynamic, innovative surgical specialties. Your path to a urology residency begins now with each course you take, each patient you encounter, and each question you ask about what kind of physician you want to become.






















