
Understanding Residency Work Hours in Emergency Medicine
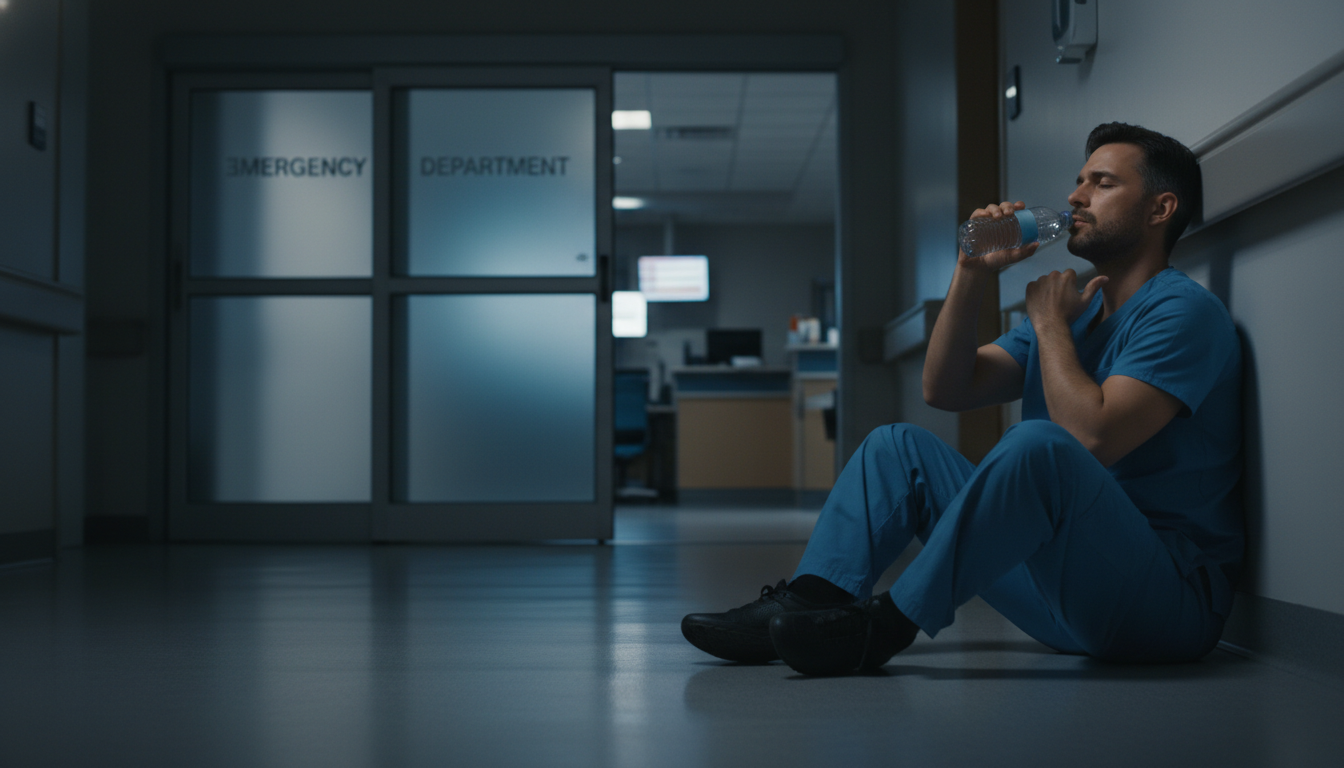
Emergency medicine residency is intense by design: unpredictable patient volumes, high-acuity cases, overnight shifts, and rapid decision-making. Within that intensity, how you manage your residency work hours will shape your training experience, your health, and your long‑term career satisfaction.
Before you can manage your time, you need to understand the framework you’re working within: duty hour regulations, program expectations, and the unique demands of an emergency medicine (EM) schedule.
ACGME Duty Hour Basics
Most U.S. EM programs follow Accreditation Council for Graduate Medical Education (ACGME) duty hour requirements. Key elements:
- 80-hour work week, averaged over 4 weeks
- 1 day off in 7, free of clinical and educational responsibilities, averaged over 4 weeks
- Minimum 8–10 hours off between shifts
- In-house call: Typically not the same as other specialties because EM relies heavily on shift work, but off-service rotations may have call
- Night float and night shifts: Must adhere to the 80-hour weekly and day-off requirements
Programs usually track these via an electronic system where you log your shifts, educational activities, and call.
Why EM Work Hours Feel Different
Compared to many other specialties:
- Shift-based schedule: Emergency medicine residency is primarily shift work rather than traditional “call.” You may not stay 28 straight hours, but you might work many intense 8–12 hour shifts in a row.
- Circadian disruption: Rotating between days, evenings, and nights is often more draining than total hours alone.
- Emotional load: High acuity, resuscitations, deaths, and social emergencies can be more exhausting than the clock suggests.
- Off-service rotations: EM residents often rotate through ICU, anesthesia, OB, surgery, etc., where schedules may be more call-heavy and less predictable.
Understanding that “80 hours” in EM is not the same as “80 hours” in some other specialties helps you anticipate stressors and craft strategies to manage them.
Typical Emergency Medicine Residency Schedules and Workload
Not all emergency medicine residency programs manage schedules the same way, but you’ll see common patterns.
Core EM Rotations: Shifts, Not Call
On core ED months, schedules usually include:
- Shift length: Commonly 8–12 hours (e.g., 8s, 9s, 10s, or 12s)
- Shift types:
- Days (e.g., 7a–3p, 8a–4p)
- Evenings (e.g., 3p–11p, 4p–12a)
- Nights (e.g., 11p–7a, 10p–6a)
- Number of shifts per month: Often 18–22 shifts/month depending on shift length, program year, and site expectations
- Weekends and holidays: You will routinely work evenings, nights, weekends, and holidays as part of EM culture
Many programs have “golden weekends” or protected time off built into the schedule, but this varies.
Year-by-Year Workload in EM
While each program is different, typical trends:
PGY-1 (Intern Year):
- Mix of EM and off-service rotations (ICU, medicine, trauma, OB, pediatrics)
- On EM: More supervised, often slightly fewer high-acuity patients but still full schedules
- Off-service: May involve overnight call, 24‑hour shifts, or ICU nights
- Feels physically demanding as you adapt to new systems and expectations
PGY-2:
- More EM months and higher responsibility in the ED
- More resuscitations, trauma leadership, and triage roles
- Often considered one of the most intense years in terms of cognitive and emotional load, even if total hours don’t change dramatically
PGY-3 (and PGY-4 in 4-year programs):
- Increased leadership (pod leader, charge-type roles)
- More autonomy and teaching responsibilities
- Some programs slightly reduce total shifts for seniors; others keep similar hours but adjust responsibilities
- Opportunity to build leadership, efficiency, and wellness routines that will carry into attending life
Residency Work Hours vs. Resident Work Life Balance
In EM, resident work life balance is not simply about counting hours; it’s about how those hours are distributed and how well you recover between them.
Important dimensions:
- Schedule predictability: Some programs schedule a month in advance with minimal last-minute changes; others shift schedules more dynamically.
- Night shift clustering: Some programs group nights (e.g., 4–5 nights in a row) then give several days off, while others sprinkle nights through the month.
- Commuting time: A 20-minute commute feels very different from 90 minutes at the end of a night shift.
- Support services: Scribes, advanced practice providers, and ancillary staff can dramatically affect how draining a shift feels.
Understanding these nuances can help you assess programs during the EM match and later manage your expectations and strategies as a resident.

Strategies to Manage Duty Hours and Prevent Burnout
Your program must follow duty hour rules, but you are responsible for managing your energy, boundaries, and habits within that framework. Below are actionable strategies.
1. Time Management on Shift: Working Smarter
Efficient on-shift habits can reduce the need to stay late and decrease cognitive fatigue.
A. Structured Task Management
- Use a checklist for each patient:
- H&P
- Orders (labs, imaging, medications)
- Reassessment
- Dispo plan
- Documentation
- Keep a pocket card or digital note with standard workups (e.g., chest pain, abdominal pain, sepsis) to speed decision-making.
B. Batch Tasks and Reassessments
- See 2–3 new patients, place all orders, then circle back as results return.
- Reassess several patients in one “round” when possible rather than one at a time in random order.
C. Documentation Efficiency
- Learn (and personalize) smart phrases and templates early.
- Document in real time when possible, particularly key decision points and conversations.
- Use a consistent note structure (e.g., CC → focused HPI → relevant ROS → PMH → PE → Assessment & Plan by problem).
D. Communication and Delegation
- Communicate clear plans to nurses and techs: “This patient needs an EKG and lab draw now; I’ll be back after results in 45 minutes.”
- Ask seniors and attendings to help you prioritize when overwhelmed: “I have three new patients and two with pending discharges; which should I see next?”
2. Before, During, and After Shift: Micro-habits that Matter
Pre-shift:
- Protect the 60 minutes before shift:
- Avoid last-minute studying or major errands.
- Focus on hydration, a light meal, and mental preparation.
- Have a pre-shift ritual: a brief walk, 5 minutes of mindfulness, or reviewing a simple checklist (badge, stethoscope, snacks, water bottle).
During shift:
- Micro-breaks (1–2 minutes):
- Step away from the monitor, stretch, slow breathing.
- When walking between rooms, take 3–5 slow deep breaths.
- Nutrition and hydration:
- Aim for small, frequent snacks vs. one large meal that induces a post-prandial slump.
- Keep a water bottle at the workstation and set a goal (e.g., finish one before mid-shift).
Post-shift:
- Create a short mental sign-off ritual:
- Note what went well.
- Identify 1–2 learning points to review later, then consciously “close the file” in your mind.
- Have a consistent wind-down process (shower, light snack, 15–20 minutes of relaxing non-screen activity) especially before sleep.
3. Protecting Your Time Off: Boundaries and Recovery
Your “1 day off in 7” and post-shift hours are critical. Treat them as non-renewable resources.
A. Say No Strategically (Especially Early)
- It’s fine to defer:
- Extra research projects
- Uncompensated committee work
- Multiple volunteering commitments
- Early PGY years should prioritize:
- Clinical competence
- Sleep and recovery
- Establishing sustainable routines
Later in residency, you can add more extracurriculars once you understand your energy and schedule.
B. Design Real Recovery Days
On true days off, aim for at least one block of 4–6 hours that’s not “productive” in the traditional sense:
- No studying, no email, no administrative tasks.
- Activities that truly recharge you (hiking, brunch, hobbies, time with family/friends, religious or spiritual practices).
C. Guard Sleep Ruthlessly
- Treat sleep as non-negotiable medical equipment, like your stethoscope.
- Avoid routinely cutting 1–2 hours off your sleep to study or socialize; over time this becomes extremely costly to your health and performance.
4. Managing Duty Hour Logs: Accuracy and Advocacy
Duty hour logs are not mere paperwork—they are a safety and wellness tool.
Be accurate:
- Log actual times, including:
- Pre-shift sign-out or chart review
- Post-shift documentation finishing
- Educational conferences and mandatory meetings
- Don’t “round down” to make things look better unless genuinely trivial (e.g., 7:58 vs. 8:00).
Speak up when patterns emerge:
- If you frequently stay >1 hour late after shifts just to finish documentation, discuss:
- Strategies for efficiency
- Potential schedule adjustments
- Whether staffing or expectations need review
- If you approach or exceed 80 hours regularly, your program is required to address it. You won’t be “weak” for reporting it; you are protecting yourself and your patients.
Night Shifts, Circadian Rhythm, and Resident Work Life Balance
Night shifts are a defining feature of emergency medicine residency. Managing them well is essential to maintaining performance and long-term health.
1. Approaches to Night Shifts
Residents (and programs) usually adopt one of three main patterns:
- Clustered nights: Several consecutive nights (e.g., 4–5) followed by several days off.
- Rotating days/evenings/nights within a short period.
- Fixed partial night block for part of the month, then switch back.
Each has pros and cons.
Clustered nights:
- Pros: Fewer circadian transitions; you can partially adjust to a night schedule.
- Cons: More intense fatigue in the middle of the block; days off can be “wasted” just recovering.
Intermittent nights:
- Pros: You never fully flip your schedule.
- Cons: You’re always somewhat out of sync; sleep can become fragmented.
2. Practical Sleep Strategies for Nights
Before a first night:
- Take a 90-minute to 2-hour nap in the late afternoon or early evening.
- Avoid a full long “daytime sleep” before your first overnight, or you may struggle to sleep the next day.
During nights:
- Use caffeine strategically, front-loading in the first half of shift and tapering by ~4–5 hours before intended sleep.
- If allowed, brief 10–20 minute “power breaks” during lulls can help; set an alarm and discuss the culture with your team.
After nights:
- Immediately after a night shift, wind down quickly:
- Light snack, shower, eye mask, and blackout curtains.
- White noise or fan to mask daytime sounds.
- Aim for 4–6 hours of core sleep post-shift, plus maybe a short nap later.
- Limit screens and bright light exposure after work; consider blue-light-blocking glasses during your commute home if it’s bright.
Flipping back to days:
- On your last night, consider sleeping a shorter period (e.g., 3–4 hours), then staying awake until an early bedtime that evening to “reset.”
- Plan light, low-stakes activities the day after your last night so your schedule nudges back toward normal.
3. Nutrition, Hydration, and Physical Health on Unusual Hours
- Meal timing: Try to anchor at least one consistent “main meal” around the same time daily (e.g., post-shift breakfast/lunch).
- Avoid heavy, greasy foods during the night that can worsen fatigue and GI discomfort.
- Have healthy, portable snacks available:
- Nuts, yogurt, fruit, string cheese, cut veggies, hummus, protein bars
- Aim for short, regular physical activity, even 10–15 minutes:
- A brief walk before or after shift
- Bodyweight exercises at home
- Don’t expect a perfect fitness routine on nights; aim for consistency, not intensity.
Integrating Learning, Career Development, and Personal Life Within EM Work Hours
Residency is more than clocking in and out; you must also grow clinically, pass boards, build a CV, and maintain a personal life. Doing all of that within duty hour limits requires deliberate planning.
1. Fitting Studying into a Busy EM Schedule
Principles:
- Study little and often rather than marathon sessions.
- Align studying with your current rotations and recent cases.
Practical tactics:
- 20–30 minutes before or after shifts (not both) on most days.
- Use commute time (if you’re not driving) to review flashcards or listen to EM podcasts.
- Keep a running list of “learning points from last shift” and review 1–2 items the next day.
Example weekly plan in a busy EM month:
- 3–4 days/week: 30 minutes of focused reading or question bank
- 1 day/week: 60–90 minutes of deeper dive (e.g., complicated topics, procedure videos)
- Pre-board period: Increase intensity for a limited time with a clear end date
Avoid trading away sleep for study on a regular basis—it erodes both learning and performance.
2. Research and CV Building Without Overload
If you aim for fellowship or an academic career, you’ll want research or scholarly activity. Balance is critical.
- Start with one primary project at a time.
- Clarify expectations: “How many hours/month will this realistically require?”
- Advocate for realistic timelines that respect EM residency work hours.
- Combine duties when possible:
- Use a QI project related to ED flow or documentation as both a scholarly project and a way to improve your own workflow.
- Turn interesting cases into case reports or teaching sessions.
3. Relationships, Family, and Life Outside the ED
Emergency medicine residency can be hard on relationships, but planning helps.
A. Shared calendar and communication
- Use a shared digital calendar with your partner/family that includes:
- All shifts (color-coded by day/evening/night)
- Call or off-service rotations
- Conferences, exams, and major deadlines
- Schedule protected time together in advance (e.g., date nights, family events, small trips) and treat them as hard commitments when possible.
B. Social life in residency
- Accept that your schedule will be “off cycle” from many friends.
- Lean on co-residents, who understand the schedule and can socialize at odd hours.
- Aim for quality, not volume of social interactions—short, meaningful touchpoints can matter more than long events you can’t sustain.
C. Protecting mental health
- Normalize therapy and counseling as part of your support system.
- Watch for warning signs: persistent sleep disturbance, irritability, emotional numbness, increased substance use, or loss of interest in previously enjoyable activities.
- Know your institution’s confidential resources and your program’s culture regarding mental health; ask senior residents how they’ve accessed help if needed.
Choosing Programs with Sustainable Work Hours: EM Match Considerations
If you’re still in the EM match or exploring programs, you can and should evaluate how programs handle residency work hours and resident work life balance.
Questions to Ask During Interviews and Second Looks
Ask residents (not only faculty):
- “On a typical EM month in PGY-2, how many shifts do you work and what are the usual shift lengths?”
- “How often do you stay late after a shift, and why?”
- “How are nights scheduled—clustered, spread out, or fixed blocks?”
- “What systems help your productivity—scribes, advanced practice providers, strong nursing support?”
- “How often do you hit the 80-hour limit, especially on off-service rotations?”
- “How does the program respond if residents are consistently close to duty hour caps?”
Ask about schedule flexibility:
- “How far in advance do you get your schedule?”
- “Can you switch shifts easily for important life events?”
- “How does the program handle parental leave, illness, or emergencies?”
Red Flags Related to Duty Hours and Wellness
Be cautious if you consistently hear:
- “We all work more than 80 hours but we just don’t log it.”
- “Everyone stays 2–3 hours late to finish charts—it’s just part of the culture.”
- “If you can’t handle this, you’re not cut out for EM.”
- “We don’t really pay much attention to duty hour logging; it’s just for the ACGME.”
Good programs foster a culture where residents feel safe being honest about their workload.
Frequently Asked Questions
How many hours do emergency medicine residents usually work?
Most emergency medicine residents work 60–80 hours per week, depending on the program, rotation, and year of training. On core EM rotations, your schedule is mostly determined by the number and length of your shifts. Off-service rotations (e.g., ICU, surgery, OB) may push you closer to the upper limit of duty hours at times, but averaged over four weeks, you must remain at or below 80 hours/week.
Is emergency medicine residency better for work life balance than other specialties?
Emergency medicine residency can offer better-defined boundaries because of its shift-based nature—when your shift ends, you usually sign out and go home. However, the rotating schedule (nights, evenings, weekends, holidays) and intensity of shifts can be challenging. Resident work life balance depends on:
- How your program distributes shifts
- Support staff and ED flow
- How well you manage sleep, stress, and expectations
- Your personal responsibilities outside the hospital
Many residents find that once they develop strong routines, EM can provide a reasonable balance, especially compared to some call-heavy specialties.
How do I avoid burnout with long residency work hours and night shifts?
Key steps:
- Prioritize sleep as non-negotiable.
- Develop pre-/post-shift routines and micro-breaks during shifts.
- Guard true off days and avoid overcommitting to extra projects early.
- Maintain connection with supportive people (co-residents, friends, family).
- Seek help early if you notice sustained mood changes, exhaustion, or loss of interest in things you normally enjoy.
- Use institutional resources (wellness programs, counseling, peer support).
Should I worry if I’m close to the 80-hour limit during residency?
Being near the 80-hour limit during certain rotations—especially ICU or heavy inpatient months—is not unusual. However:
- If you consistently hit or exceed 80 hours/week averaged over 4 weeks, discuss it with your chief residents or program leadership.
- Use accurate duty hour logging; it’s designed to protect you.
- Look for systemic issues (inefficient workflows, poor staffing, unrealistic expectations) that might be driving chronic overwork.
Your safety, learning, and long-term career health are just as important as meeting service demands.
Managing residency work hours in emergency medicine is not about perfection—it’s about deliberate, sustainable strategies that let you learn deeply, care for patients safely, and preserve your own health. With realistic expectations, strong habits, and open communication with your program, you can navigate the EM residency years and build a career you can thrive in for decades.






















