
Understanding the Landscape: Is Private Practice in Internal Medicine Still Viable?
Starting a private practice in internal medicine can be one of the most rewarding—yet challenging—career paths after completing your internal medicine residency. In an era of consolidation, large hospital systems, and value-based care, many residents wonder whether opening medical practice is still realistic or if employment is now the only practical option.
The short answer: yes, a private internal medicine practice is still viable, but the pathway, risks, and rewards are very different from what they were 20–30 years ago. As a future internist, you need to think about:
- Your long-term career goals – autonomy, income potential, work–life control
- Your risk tolerance – taking on debt, variable income, business responsibility
- Your local market – competition, payer mix, demographics, health system dominance
- Your personal strengths – clinical excellence, leadership, communication, and willingness to learn business skills
For many residents, the trajectory looks like this:
- Internal medicine residency → IM match completion
- First few years in employed practice (hospital, academic, large group)
- Transition to private practice after gaining experience, mentorship, and capital
Others may join an existing private group straight out of residency and become partners later. Starting a solo practice directly after residency is possible but significantly higher risk and requires strong mentorship and support.
Before diving into logistics, take an honest look at your motivation.
Clarify Your “Why” for Private Practice
Ask yourself:
- Do I want control over how I practice medicine (visit length, workflows, staffing)?
- Am I comfortable being ultimately responsible for payroll, rent, and overhead?
- Does the idea of building something that’s mine energize me or stress me out?
- Am I willing to invest non-clinical time in management, compliance, and strategy?
- Is my priority maximizing autonomy and long-term equity, even if my short-term salary is lower?
Your answers will guide whether you should aim for:
- Solo or small-group traditional fee-for-service practice
- Concierge or direct primary care (DPC) model
- Joining or buying into an existing independent internal medicine group
- Or choosing employment and possibly side ventures instead of practice ownership
Understanding private practice vs employment tradeoffs up front will help you make deliberate decisions as you finish residency and plan your next steps.
Planning Your Path: From Residency to Private Practice
Your preparation for starting a private internal medicine practice ideally begins during residency—even if you won’t open your doors until several years after graduation.
Step 1: Build a Marketable Clinical Profile During Residency
To be successful in private practice, you need both solid general internal medicine skills and some differentiators. During residency:
Aim for broad competence
- Seek strong rotations in ambulatory IM, geriatrics, cardiology, endocrinology, and hospital medicine.
- Learn common outpatient procedures: joint injections, skin biopsies, EKG interpretation, simple dermatologic care, etc.
Develop at least one or two niche interests that can become part of your practice branding:
- Diabetes management / obesity medicine
- Women’s health in medicine
- Geriatric care / complex multimorbidity
- Office-based cardiology or pulmonary follow-up
- Addiction medicine, HIV primary care, or transitions of care
Being the “go-to” internist for something helps build referrals.
Practice efficient documentation and coding
- Shadow billing and coding teams if possible.
- Learn evaluation and management (E/M) coding basics.
- Understand documentation that supports higher-complexity visits without upcoding.
Take electives in practice management if your program offers them:
- Quality improvement, leadership, EMR optimization, or health systems management.
Step 2: Learn the Business of Medicine Early
Most residents get minimal formal training in the business side of private practice. To prepare for opening medical practice later, consider:
Self-education
- Read books on medical practice management, physician finance, and negotiation.
- Follow physician-entrepreneur blogs and podcasts focused on private practice.
- Take inexpensive online courses on healthcare finance and small-business accounting.
Mentorship
- Seek out attendings who are in private practice (not just employed by the hospital).
- Ask for 30-minute informational conversations: How did they start? What would they do differently? What’s their typical week like?
Practical exposure
- Do a community ambulatory rotation in a private internal medicine practice.
- Observe front-desk workflows, billing processes, and patient-flow decisions.
These early experiences give you a realistic sense of what you’re signing up for and build a network you’ll draw on later.
Step 3: Decide on Timing and Model
There’s no single right time after your IM match and residency to start private practice, but common options include:
Immediate transition: start or join a private practice right out of residency
- Pros: early autonomy, less “deprogramming” from institutional habits, faster equity building
- Cons: steep learning curve, financial risk, student loan burden, limited capital
2–5 years of employment, then start or buy-in
- Pros: increased savings, better credentials, relationships with referring physicians, time to study business
- Cons: inertia of a stable job, golden handcuffs of RVU bonuses, family obligations
Join existing private group with a partnership track
- Pros: less startup risk, infrastructure already in place, mentorship from partners
- Cons: less control initially, partnership terms may be restrictive
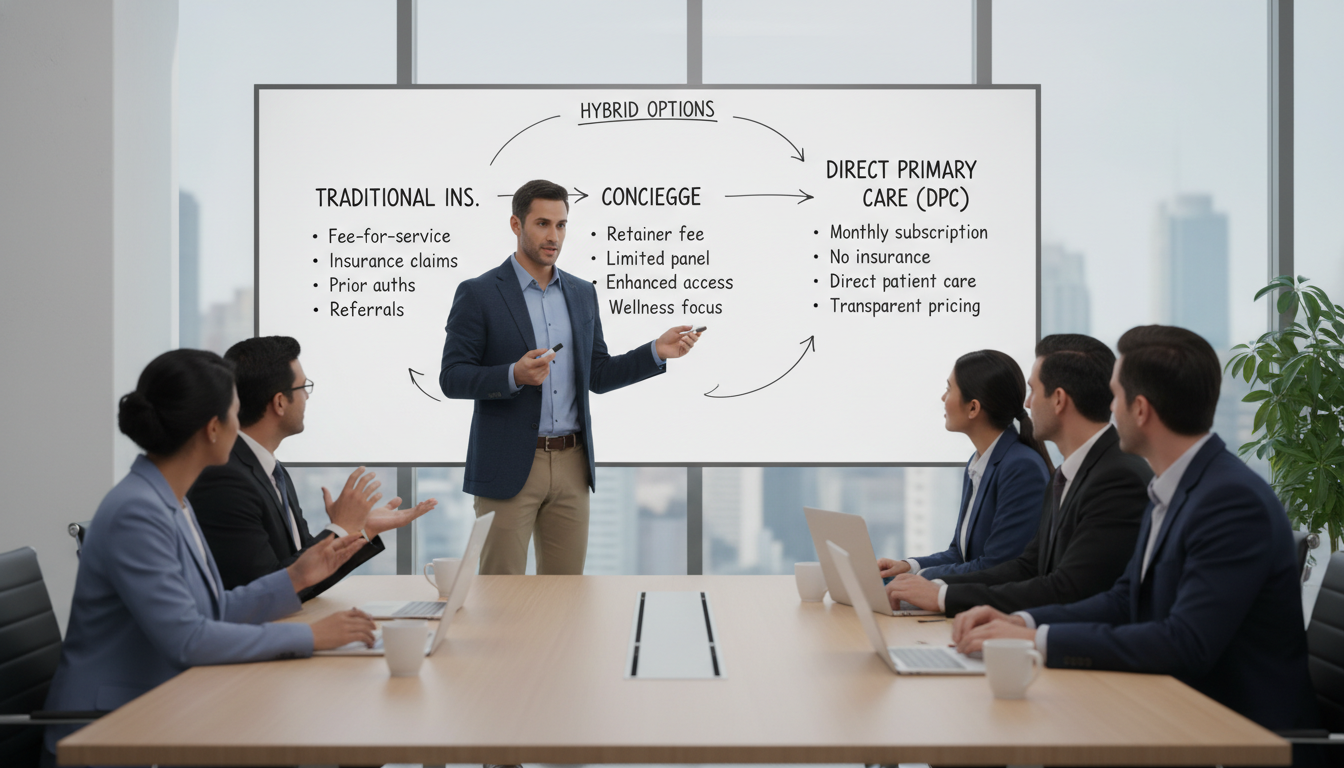
Also decide on your practice model:
- Traditional insurance-based internal medicine clinic
- Concierge / retainer-based practice (annual membership fee; fewer patients, more time per visit)
- Direct primary care (DPC) (monthly fee, transparent pricing, often no insurance billing)
- Hybrid models combining elements of the above
Each has implications for panel size, revenue structure, staffing, and technology.
Designing Your Practice: Strategy, Location, and Structure
Once you’ve clarified your “why” and timing, your next focus is designing a practice that can actually thrive in your local market.
Market Research: Know Your Environment
Before signing a lease or ordering furniture, analyze:
Local demographics
- Age distribution (more Medicare vs commercial insurance)
- Socioeconomic status, employment rates
- Chronic disease prevalence (obesity, diabetes, heart disease)
Competitive landscape
- Number and size of existing internal medicine and family medicine practices
- Presence of large health systems or multispecialty groups
- Availability of subspecialists and hospital partners
Payer mix and reimbursement
- Dominant insurers in the region and typical payment rates
- Medicaid expansion status; Medicaid rates and administrative burden
- Medicare Advantage penetration vs traditional Medicare
Access and convenience factors
- Public transportation and parking
- Underserved neighborhoods or growing suburbs
- Telemedicine friendliness (e.g., state licensing, broadband access)
A short drive around your target area plus online research (state medical board, insurer provider directories, local business registries) can be surprisingly revealing.
Choosing a Location
Your physical site will drive both patient experience and overhead:
Medical office building vs street-level retail
- Medical buildings: built-in referrals, shared imaging/lab, easier compliance
- Retail/office space: higher visibility, better signage, easier parking, may require more build-out
Size and layout
- For solo IM practice: 1–2 exam rooms minimum; 3–4 if you plan to grow or have an NP/PA
- One physician often targets 1,200–2,000 sq ft, depending on number of staff and services
- Functional layout: reception, waiting area, exam rooms, physician office, staff work area, storage, clean/dirty utility, ADA-compliant bathrooms
Lease terms
- Negotiate tenant improvement allowances (TI) for build-out
- Look for options to expand if your panel grows
- Pay attention to: length of lease, escalation clauses, renewal options, and exclusivity clauses
Work with a commercial real estate broker who has experience with medical tenants; they often save more than they cost.
Choosing Your Legal and Business Structure
Most internal medicine private practices choose one of the following:
- Professional Corporation (PC / PA / PLLC) depending on state law
- Partnership or group PC if you are starting with other physicians
- S-corp or LLC structures for tax efficiency, again based on state rules
Consider:
- Liability and asset protection – malpractice is covered by insurance, but you also want to protect personal assets from business creditors.
- Taxation – how income flows to you, ability to retain profits in the business, and retirement plan options.
- Future growth – ease of adding partners or associates.
Engage:
- A healthcare attorney to set up the practice entity and review contracts.
- A CPA with medical practice experience to structure your books and advise on taxes.
Credentialing, Licensing, and Contracts
Before you can see insured patients and get paid, several parallel processes must be completed:
Licensure & IDs
- Valid state medical license
- DEA registration (and any state-specific controlled substance registry)
- NPI (National Provider Identifier)
Payer credentialing
- Medicare enrollment (PECOS)
- Medicaid (if you choose to participate)
- Major commercial insurers in your region
- Medicare Advantage and managed care plans, as appropriate
Credentialing can take 3–6 months or longer; start early. Some physicians use third-party credentialing services to manage forms and follow-up.
- Hospital privileges
- If you plan to follow your patients in the hospital or admit to certain facilities, start the credentialing process early and understand call responsibilities.
Building the Foundation: Finances, Staffing, and Operations
A successful internal medicine residency prepares you for disease management; it does not teach you how to build a functioning business. This section covers the core building blocks of opening medical practice: finances, staffing, systems, and workflows.
Financial Planning and Startup Budget
When starting a private practice, underestimating costs is a common reason for early stress or failure. Major categories:
Startup Costs (one-time)
- Legal and accounting fees
- Entity formation and licensing
- Lease deposits and build-out (construction, renovation, permits)
- Furniture and equipment (exam tables, scales, BP cuffs, ECG, spirometry)
- IT infrastructure (computers, networking, printers, telephones)
- EMR system setup and training fees
- Initial supplies (medical/surgical, office, forms, PPE)
- Marketing and branding (signage, website, logo, print materials)
Operating Expenses (ongoing)
- Rent and utilities
- Staff salaries and benefits
- Malpractice insurance
- EMR subscription and practice management software
- Billing service or in-house billing staff
- Medical and office supplies
- Lab contracts and waste disposal
- Insurance (general liability, property, cyber, workers’ comp)
Develop 12–18 months of projected cash flow including:
- Expected patient volume ramp-up (e.g., 5–8 patients/day initially, rising to 16–20+)
- Average reimbursement per visit (varies by payer mix and complexity)
- Conservative assumptions for no-shows and denials
Funding Options
Most physicians use a combination of:
- Personal savings
- Bank loans or SBA loans (often with a business plan and projections)
- Lines of credit for working capital
- Equipment leases rather than outright purchase
Keep your personal budget lean in the first 1–2 years; it often takes time to build a robust patient panel and stable revenue.
Staffing: Build a Lean, High-Functioning Team
Your staff will shape patient experience and your own daily stress. Key roles:
Front-desk / receptionist
- Schedules appointments, verifies insurance, handles check-in/out, manages phone calls
- Needs excellent people skills and attention to detail
Medical assistant (MA) or LPN
- Rooming patients, vitals, injections, EKGs, basic procedures, patient flow support
- Cross-train to help with prior authorizations and refills
Biller / coder (in-house or outsourced)
- Claims submission, payment posting, denial management, prior auth support
- For small practices, outsourcing can be cost-effective initially
Practice manager or office manager (often added later)
- Oversees operations, HR, vendor relationships, financial tracking
In a solo internal medicine practice, you might start with:
- 1 front-desk staff
- 1 MA or LPN
- Outsourced billing
and then scale up as volume grows.
Technology and EMR Choices
Your choice of EMR and practice management software is crucial. Consider:
- Cloud-based vs server-based – most new practices choose cloud-based to avoid large upfront hardware costs.
- Specialty fit – does the EMR support internal medicine templates, chronic disease registries, and population health tools?
- Interoperability – can you easily exchange data with local hospitals and specialists?
- Integrated features – e-prescribing, patient portal, telehealth, secure messaging, e-fax.
- Billing integration – practice management module for claims, eligibility, and reporting.
Evaluate demos from at least 2–3 vendors and talk to existing internal medicine users about real-world pros and cons.
Operational Workflows: Start with “Good Enough,” Then Optimize
Document clear workflows for:
- New patient intake and registration
- Check-in / check-out process
- Prescription refills and prior authorizations
- Lab/imaging orders and result tracking
- Referral management
- Care coordination for high-risk patients
- Telemedicine visits (if offered)
Initially, aim for simple, reliable processes. As your panel grows, you can refine for efficiency and quality—often with staff input and basic quality-improvement cycles (Plan–Do–Study–Act).

Growing and Sustaining Your Internal Medicine Private Practice
Once you’ve opened the doors, the focus shifts to growth, quality, and long-term stability.
Building Your Patient Panel
New-patient volume is the lifeblood of any new internal medicine residency graduate entering private practice. Strategies include:
Referrals from other physicians
- Visit local subspecialists, urgent care centers, and ED physicians.
- Send short, clear consult notes back quickly to build trust.
- Position yourself as a reliable primary care home for complex adults.
Community outreach
- Give talks at community centers, senior centers, or local employers.
- Participate in health fairs or free blood pressure/diabetes screenings.
- Partner with local gyms, churches, or cultural organizations.
Online presence
- Professional website with clear information: services, insurance accepted, patient forms, how to schedule.
- Accurate listings on Google Business, Healthgrades, Zocdoc, and insurer directories.
- Encourage satisfied patients to leave honest online reviews (within ethical and legal limits).
Access and convenience
- Offer early-morning or early-evening slots at least one day a week.
- Same- or next-day acute slots for existing patients.
- Telemedicine appointments for appropriate concerns.
Clinical Quality and Patient Experience
Long-term success depends on delivering excellent care while managing complexity and costs. Focus on:
Evidence-based chronic disease management
- Hypertension, diabetes, CHF, COPD, CKD, and cardiovascular risk management.
- Use registries or EMR tools to identify patients needing outreach.
Preventive care and screenings
- Cancer screenings, vaccinations, lifestyle counseling.
- Use standing orders for nurses/MA to increase efficiency.
Patient communication
- Clear explanations, teach-back method, and written instructions.
- Reasonable response times to portal messages and calls.
Feedback loops
- Short patient satisfaction surveys (paper or electronic).
- Regular staff meetings to discuss pain points and improvement ideas.
Financial Health and Metrics
Monitor key performance indicators (KPIs):
Volume metrics
- New patients per month, total visits per day/week
- No-show and cancellation rates
Revenue metrics
- Collections per visit and per provider
- Days in accounts receivable (AR)
- Denial rates and reasons
Cost metrics
- Overhead percentage (often 50–65% in traditional IM practices)
- Staff costs as a proportion of total expenses
Use these data to adjust scheduling templates, staffing, payer contracting, and service offerings.
Considering Concierge or DPC Transitions
Some internists move toward concierge medicine or direct primary care as a way to:
- Reduce panel size (e.g., from 2,000+ to 400–800 patients)
- Increase visit length and accessibility
- Stabilize revenue via membership fees
This can be attractive if you’re feeling squeezed by high volumes and administrative burden, but:
- Check state and federal laws, including Medicare regulations.
- Carefully communicate changes to patients to avoid backlash.
- Run detailed financial scenarios; transitions often involve short-term revenue dips.
Private Practice vs Employment: Making the Right Long-Term Choice
As you move from residency and IM match into attending life, you’ll inevitably compare private practice vs employment options.
Key Differences
Autonomy
- Private practice: High. Control over scheduling, clinical protocols (within standards), staffing, and strategic direction.
- Employment: Variable. Often subject to institutional policies, scheduling templates, and productivity metrics.
Financial Risk and Reward
- Private practice: Higher risk (overhead, variable income, business liability); higher upside if well-managed and eventually sold or passed on.
- Employment: Lower risk; stable salary with potential RVU or quality bonuses; no equity.
Administrative Burden
- Private practice: You ultimately own the problems—HR, leases, payer negotiations—but can delegate over time.
- Employment: Administrative infrastructure provided, but you may have limited influence over systems and policies.
Lifestyle Flexibility
- Private practice: Ability to design your schedule, add or reduce hours over time, and pivot models (e.g., concierge).
- Employment: Often more vacation and benefits early on; changing FTE or leaving may be more constrained.
Hybrid and Transitional Models
You don’t have to pick one for life:
- Join a large group now with a path to partial ownership.
- Start in employment and later:
- Buy into a practice
- Co-found a new group with trusted colleagues
- Launch a side DPC or telemedicine practice (check contracts for non-competes)
Revisit your career goals every 3–5 years. What fit at PGY-3 may not fit at age 40 with different financial and family circumstances.
FAQs: Starting a Private Practice in Internal Medicine
1. How long after residency should I wait before starting my own internal medicine private practice?
Many internists benefit from 2–5 years of employed experience before opening medical practice. This allows you to:
- Hone clinical skills and efficiency
- Build a local reputation and referral network
- Accumulate savings and reduce debt
- Learn from how others run (or mismanage) practices
However, if you have strong mentorship and a clear plan, starting sooner is possible—especially if you join an existing group.
2. How much money do I need to start a solo internal medicine practice?
Numbers vary widely by region, but a typical range for startup plus initial working capital is often in the low- to mid-six figures. A realistic rough ballpark:
- $100,000–$250,000 in startup costs (build-out, equipment, IT)
- Several months of operating expenses (rent, salaries, insurance)
Work with a CPA to build detailed projections; overestimate costs and underestimate early revenue.
3. Is a concierge or direct primary care model better for internal medicine?
Both can work well for internists:
- Concierge: Often retains insurance billing plus an annual membership fee; higher-touch service, smaller panel.
- Direct Primary Care (DPC): Typically no insurance billing; monthly membership covers most primary care services; simpler billing and potentially stronger patient relationships.
Your choice depends on local demographics, your risk tolerance, and how much you want to decouple from insurer constraints.
4. What’s the biggest mistake new internal medicine private practice owners make?
Common pitfalls include:
- Underestimating how long it takes to build a patient panel and cash flow
- Choosing the wrong location or signing an unfavorable lease
- Skimping on billing expertise, leading to poor collections
- Not tracking financial and quality metrics from the start
Proactive planning, mentorship from experienced private practitioners, and working with a healthcare-savvy attorney and CPA can prevent many of these issues.
Starting a private practice in internal medicine demands courage, preparation, and a willingness to learn skills far beyond what’s taught in residency. With careful planning, honest self-assessment, and the right advisors, it can offer a uniquely satisfying blend of clinical autonomy, long-term financial potential, and the opportunity to shape the patient experience on your own terms.






















