
Understanding Surgical Fellowship Pathways: The Big Picture
Surgical fellowship pathways represent the bridge between core surgical training and true subspecialty expertise. For many residents, choosing whether to pursue a surgical fellowship—and which type—is one of the most consequential career decisions they will make.
In today’s landscape, most newly minted general surgeons and many other surgical trainees continue into at least one additional year of specialized training. Whether you are contemplating a surgical oncology fellowship, a minimally invasive fellowship, or a highly focused surgery subspecialty such as hepatopancreatobiliary (HPB) surgery or complex spine, it’s essential to understand:
- How fellowships fit into the broader training pathway
- The major categories of surgical subspecialties
- How accreditation and match processes differ
- Strategic considerations for applications and career planning
This guide walks through the full arc—from the decision to subspecialize, through types of surgical fellowship, to application strategy and long‑term career implications—tailored for residents navigating residency match and applications decisions.
From Residency to Fellowship: How Surgical Training Is Structured
Before diving into individual pathways, it helps to clarify how fellowship fits into the overall surgical training timeline.
Core Surgical Training Pathways
Most surgical fellowship applicants come from one of the following primary residency tracks:
General Surgery (5–7 years)
- Traditional 5-year clinical track
- Some with 1–2 additional research years (often between PGY-2 and PGY-3)
- Leads to American Board of Surgery (ABS) eligibility
Integrated Surgical Programs (e.g., I-6)
- Integrated thoracic surgery (6 years)
- Integrated vascular surgery (5 years)
- Some graduates still complete additional fellowships (e.g., structural heart, advanced aortic)
Other Surgical Specialties (5–7 years)
- Orthopaedic surgery
- Neurosurgery
- Otolaryngology–Head & Neck Surgery
- Urology
- Plastic surgery
- Obstetrics & Gynecology (for Gyn Oncology, FPMRS)
- Ophthalmology (for oculoplastics, retina, glaucoma, etc.)
From these platforms, trainees choose targeted surgical subspecialty training to develop advanced competencies and refine their career niche.
Why Pursue a Surgical Fellowship?
Residents commonly consider a surgical fellowship for the following reasons:
Case complexity and expertise
- Desire to handle high-acuity, referral-level pathology
- Interest in technically demanding procedures (e.g., liver resections, robotic pancreatectomies, complex reconstructive microsurgery)
Career competitiveness and employability
- Expanding demand for subspecialists at academic and large community centers
- In many regions, fellowship training is becoming the “new baseline” for certain jobs (e.g., breast surgery, colorectal, vascular)
Academic and research aspirations
- Fellowship provides structured mentoring and scholarly opportunities
- Necessary for many academic and cancer center positions (e.g., surgical oncology fellowship for NCI-designated cancer centers)
Lifestyle and practice pattern alignment
- Some subspecialties offer more predictable schedules (e.g., breast, endocrine)
- Others emphasize team-based, shift-like ICU or trauma models
The key is not that fellowship is “better” than going straight into practice, but whether it fits your clinical interests, long-term career vision, and personal priorities.
Major Categories of Surgical Fellowship Pathways
Surgical fellowship options are extensive and constantly evolving. Below are the common pathways, organized by core residency and major surgery subspecialty groupings, with a focus on residents in general surgery and closely related fields.
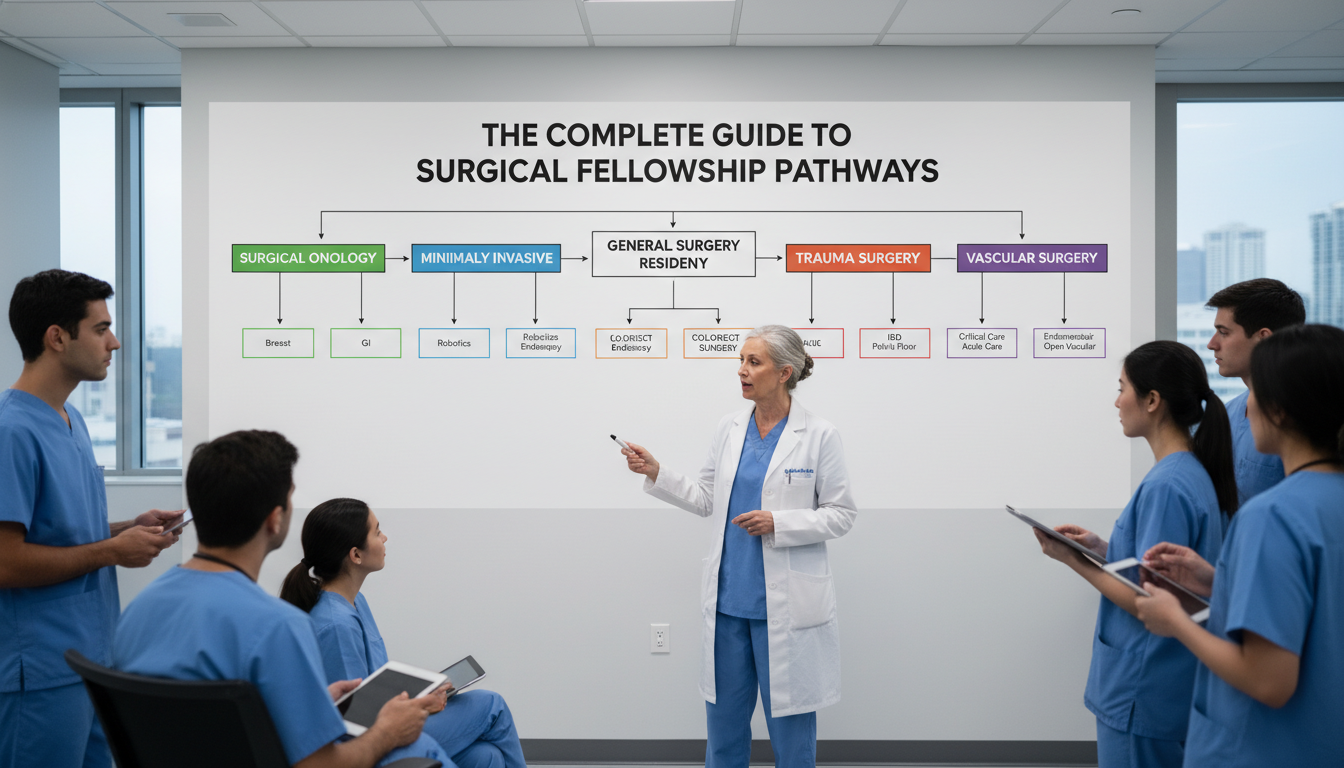
1. General Surgery–Based Fellowships
Most general surgery residents pursuing subspecialty training choose from the following:
Surgical Oncology Fellowship
Focus:
- Multidisciplinary cancer care
- Complex resections (HPB, GI, sarcoma, melanoma)
- Coordination with medical and radiation oncology
Typical Duration: 2–3 years (often includes dedicated research time)
Settings: NCI-designated cancer centers and academic institutions
Career Paths:
- Academic surgical oncologist
- Cancer center leadership roles
- Regional referral surgeon for complex malignancy
Ideal For Residents Who:
- Enjoy tumor boards, longitudinal cancer care, and complex decision-making
- Are interested in research, clinical trials, and guidelines development
- Want a career at a high-volume center
Surgical oncology fellowship training is increasingly valued as cancer care becomes more specialized and protocol-driven, and it is often essential for those targeting academic oncology careers.
Hepatopancreatobiliary (HPB) Surgery
Focus:
- Complex liver, pancreas, and biliary tract surgery
- Management of primary and metastatic liver lesions
- Integration with transplant and oncology teams
Duration: 1–2 years
Overlap: Often linked with surgical oncology or transplant programs
Career Paths:
- Academic HPB surgeon
- High-volume tertiary/quaternary referral centers
Colorectal Surgery
Focus:
- Benign and malignant colorectal disease
- Inflammatory bowel disease, pelvic floor disorders
- Advanced endoscopy and minimally invasive approaches
Duration: 1 year (ACGME-accredited)
Career Paths:
- Academic colorectal surgery
- High-volume community practices
Appeal:
- Strong demand, broad mix of open and minimally invasive cases
- Good balance of procedural diversity and subspecialized focus
Trauma, Acute Care Surgery & Surgical Critical Care
Trauma & Acute Care Surgery (ACS)
- Focus: Trauma resuscitation, emergency general surgery, ICU care
- Duration: Usually 1–2 years; frequently combined with surgical critical care
Surgical Critical Care (SCC)
- Focus: ICU management of surgical and trauma patients
- Duration: 1 year (ACGME-accredited)
Career Paths:
- Academic trauma/ACS surgeon
- Level I/II trauma center practices
Lifestyle & Practice:
- Shift-based models increasingly common
- High-acuity, team-based work; plenty of variety
Minimally Invasive & Bariatric Surgery
- Focus:
- Advanced laparoscopic and robotic surgery
- Foregut, hernia repair, bariatric procedures
- Duration: 1 year
- Career Paths:
- Bariatric/metabolic surgery-focused practices
- Community general surgery with MIS leadership roles
- Key Skills:
- High case volume in laparoscopy, robotics, endoscopy
- Often seen as a broad “value-add” fellowship that enhances general surgery practice
Breast Surgical Oncology
- Focus:
- Comprehensive breast cancer and benign breast disease care
- Oncoplastics, image-guided surgery, multidisciplinary management
- Duration: 1 year
- Career Paths:
- Academic breast surgeon
- Community breast centers and oncology groups
- Considerations:
- Highly multidisciplinary, continuity of care emphasis
- Growing emphasis on genetics, risk stratification, survivorship
Endocrine Surgery
- Focus: Disorders of the thyroid, parathyroid, adrenal, and endocrine pancreas
- Duration: 1–2 years
- Appeal:
- High-volume, highly specialized operations
- Relatively predictable call and lifestyle compared with some other fields
Transplant Surgery
- Focus:
- Liver, kidney, pancreas (and occasionally multivisceral) transplantation
- Duration: 2–3 years
- Career Paths:
- Academic transplant programs, large tertiary centers
- Considerations:
- Intense call, nocturnal work, and emergency cases
- Close long-term patient relationships and complex immunology
2. Plastic, Hand, and Reconstructive Fellowships
While plastics is its own residency, general surgery residents can access some pathways:
Plastic Surgery (Independent Track)
- 3-year independent residency after general surgery
- Highly competitive, reconstructive and aesthetic focus
Hand Surgery Fellowship
- Available to plastic, ortho, and general surgery graduates (in select programs)
- Focus on trauma, nerve, tendon, and complex hand disorders
3. Vascular, Cardiothoracic, and Cardiac Fellowships
Vascular Surgery (Traditional Fellowship)
- Eligible Background: General surgery graduates
- Duration: 2 years
- Focus:
- Open and endovascular management of arterial and venous disease
- Note: Integrated 5-year vascular residencies now complement traditional fellowships.
Thoracic & Cardiothoracic Surgery
Thoracic / Cardiothoracic Fellowships (Traditional)
- 2–3 years after general surgery
- Focus: Complex thoracic, cardiac, aortic operations
Integrated Programs (I-6)
- Some graduates still do additional fellowships (e.g., structural heart, transplant, ECMO)
4. Pediatric Surgery and Subspecialty Peds Fellowships
- Pediatric Surgery Fellowship
- Highly competitive, 2-year fellowship after general surgery
- Focus: Neonatal, pediatric, and adolescent surgical care
- Additional Pediatric Subspecialties (via other cores):
- Pediatric orthopaedics, pediatric neurosurgery, pediatric urology, etc.
Accreditation, Match Systems, and Application Logistics
Not all surgical fellowships follow the same structures for accreditation or match. Understanding this early helps you plan timelines and strategy.

ACGME vs. Non-ACGME Fellowships
ACGME-Accredited Fellowships
- Examples: Colorectal, vascular (traditional), cardiothoracic, surgical critical care, pediatric surgery
- Benefits:
- Standardized curriculum and competencies
- Board eligibility in that subspecialty (when applicable)
- Often required for specific credentialing or hospital privileging
Non-ACGME Fellowships
- Examples: Many HPB, some surgical oncology programs, advanced MIS, certain transplant, specialized robotic or endoscopic fellowships
- Benefits/Limitations:
- Can be highly focused and innovative
- Variable structure and oversight
- May or may not confer additional formal board certification
Both pathways can lead to excellent careers; the key is verifying the program’s track record, case volume, and graduate outcomes.
Match Systems: ERAS, NRMP, SF Match, and Direct Application
Fellowships may use:
ERAS + NRMP Match
- Common for many ACGME-accredited fellowships
- Standardized application, LoRs, personal statement, centralized ranking and matching
SF Match
- Used by several surgical subspecialties (e.g., some hand, microsurgery)
- Similar centralized process but through a different platform
Program-Specific or Consortium Matches
- Some surgical oncology and HPB fellowships use discipline-specific portals (e.g., SSO for surgical oncology)
- Others use specialty society-run match systems
Direct Application (Outside a Formal Match)
- CV + letters + personal contact with PDs
- Offers may be made on a rolling basis, often earlier than match-based specialties
Timing: When to Apply
The application timeline has been trending earlier:
- Most Surgical Fellowships:
- Applications are often submitted in PGY-3 or early PGY-4
- Interviews occur PGY-4; match or offer typically before PGY-5
- Highly Competitive Fields (e.g., pediatric surgery, some surgical oncology):
- Preparation may begin as early as PGY-2 for research alignment and mentorship
Key actions:
- Check your specialty society website (e.g., SSO, EAST, AAST, ASCRS, ACS) by early PGY-3 for your target fellowship.
- Map deadlines, match dates, and any program-specific requirements well in advance.
Building a Competitive Fellowship Application
To earn a position in a strong surgical fellowship—especially in sought-after areas like surgical oncology fellowship programs, HPB, pediatric surgery, or transplant—you’ll need deliberate preparation starting early in residency.
1. Clinical Excellence and Evaluations
Fellowship directors want evidence that you are:
- Technically competent and safe
- Reliable, professional, and team-oriented
- Capable of independent judgment by the end of residency
Practical steps:
- Seek progressive responsibility on services aligned with your target field.
- Ask for formative feedback early (PGY-2/3) and act on it.
- Strive for strong ABSITE scores, especially for fields where cognitive load is high (e.g., surgical oncology, transplant).
2. Research and Scholarly Productivity
Most competitive surgery subspecialty fellowships expect at least some scholarly output:
- Types of Activity That Help:
- Retrospective chart reviews, clinical series, QI projects
- Case reports/series in niche areas relevant to your desired fellowship
- Prospective trials, translational research, database analyses (if available)
- Outputs to Aim For by PGY-4:
- 1–3 peer-reviewed publications
- Abstracts or posters at national specialty meetings
- Presentations at institutional research days
Align research with your field:
- If targeting a surgical oncology fellowship, aim for projects involving GI cancers, melanoma, sarcoma, or HPB.
- For MIS, focus on hernia, foregut, bariatric outcomes, or robotic surgery research.
3. Mentorship and Networking
Strategic mentorship is often decisive:
- Identify one primary career mentor in your desired field by early PGY-3.
- Seek letters of recommendation from recognized subspecialty surgeons who can speak to your clinical and scholarly strengths.
- Attend national meetings (e.g., SSO, AHPBA, ASCRS, SAGES, EAST, AAST) and introduce yourself to leaders and program directors.
Effective tactics:
- Ask to help with your mentor’s talks, posters, or manuscripts.
- Request a practice run of your fellowship interview with senior faculty.
- Get targeted feedback on your CV and personal statement from mentors in that subspecialty.
4. Personal Statement and Application Strategy
Your personal statement should:
- Clearly articulate why that subspecialty (e.g., why surgical oncology vs. HPB vs. MIS)
- Convey long-term goals (academic vs. community; research-intensive vs. clinically focused)
- Reflect insight into the field’s challenges (e.g., palliative dimensions in oncology, chronic disease in transplant)
Application strategy:
- Apply broadly for competitive fields, especially if your metrics (ABSITE, publications) are moderate.
- Tailor your CV and experiences section to highlight relevant rotations, electives, and research.
Strategic Career Planning: Choosing the Right Surgical Fellowship Path
The “right” surgical fellowship is not just the most prestigious or competitive option; it’s the one that best aligns with your skills, values, and vision for your life 10–20 years from now.
Clarify Your Clinical Interests and Strengths
Reflect on:
- Which cases make time fly in the OR?
- Do you prefer high-acuity emergencies or scheduled oncologic resections?
- Are you drawn to continuity of care (breast, endocrine, oncology) or episodic, high-intensity encounters (trauma, transplant)?
Use electives and away rotations to “test-drive” fields. If possible:
- Spend a full month on subspecialty services (e.g., HPB, breast, vascular)
- Ask attendings about real-world practice patterns and how their fellowship training shaped their jobs.
Consider Lifestyle and Practice Environment
Key factors:
Call structure and intensity:
- Trauma, transplant, and some vascular jobs can be demanding but rewarding.
- Breast, endocrine, and some MIS-focused practices may offer more predictability.
Academic vs. Community:
- Academic positions often expect research, teaching, and committee roles in addition to clinical work.
- Community practices may be more clinically intensive but with clearer work–life boundaries.
Geographic Goals:
- Some regions have strong demand for certain subspecialties (e.g., colorectal, MIS) but saturated markets for others (e.g., breast in urban centers).
- Talk to alumni and mentors about job market realities.
Single vs. Multiple Fellowships
In some cases, surgeons pursue sequential fellowships (for example, surgical oncology fellowship followed by HPB; trauma + SCC; MIS + bariatric). Consider:
Pros:
- Highly specialized niche and unique skillset
- Strong academic credibility in complex cross-disciplinary fields
Cons:
- Longer training (delayed earning potential)
- Risk of over-specialization limiting job flexibility in certain markets
Weigh these decisions carefully with input from trusted mentors and recent graduates.
Frequently Asked Questions About Surgical Fellowship Pathways
1. Do I need a surgical fellowship to get a good job after general surgery residency?
No—not universally. In some regions and practice settings, a well-trained general surgeon can still secure excellent positions immediately after residency. However:
- In urban and competitive markets, fellowship training is increasingly expected or strongly preferred.
- For specific fields (e.g., surgical oncology fellowship graduates at NCI centers, colorectal surgery at academic hubs), fellowship is essentially required.
- A “broad-based” fellowship like MIS or trauma/ACS can enhance job options even for those planning a primarily general surgery practice.
The decision should be based on your target geography, practice type, and subspecialty interest rather than a blanket assumption that fellowship is mandatory.
2. How early should I decide on a surgical subspecialty?
You don’t need to lock in during intern year, but by early PGY-3 you should:
- Narrow down to 1–2 serious options
- Establish relationships with mentors in those fields
- Start or join at least one subspecialty-aligned research project
Highly competitive fields (e.g., pediatric surgery, some surgical oncology fellowships) may require earlier planning, especially if you’ll do dedicated research years.
3. Can I switch subspecialties after completing a fellowship?
Switching is possible but can be challenging and may require:
- Additional fellowship training in the new area
- Demonstrated experience (e.g., case logs, CME, proctorships)
- Institutional willingness to support your transition
Examples:
- An MIS-trained surgeon may later complete a surgical oncology fellowship to refocus on cancer care.
- A general surgeon who practiced broadly for several years might later pursue breast or endocrine fellowships.
However, such shifts carry opportunity cost and time; it’s better to invest heavily in choosing your initial path thoughtfully.
4. How important is research for getting into a top surgical fellowship?
Research expectations vary:
- Critical for: Pediatric surgery, many surgical oncology and transplant programs, highly academic HPB centers.
- Helpful but not always mandatory for: MIS, trauma/ACS, colorectal, breast, endocrine, depending on program type.
In general:
- Having some research shows initiative, academic curiosity, and ability to complete projects.
- High-volume publications strengthen applications to research-heavy, academic fellowships.
- If your interest is primarily community practice, strong clinical performance and fit can outweigh limited research, especially in clinically oriented programs.
A surgical fellowship can profoundly shape your clinical practice, career trajectory, and daily life. Understanding the spectrum of surgical subspecialty options—from surgical oncology fellowship pathways to trauma, MIS, vascular, and beyond—allows you to plan proactively, cultivate the right mentorship, and build an application that authentically reflects your goals. As you move through residency match and applications decisions, keep revisiting your clinical interests, lifestyle priorities, and long-term vision, and use your mentors and specialty societies as guides along the way.






















