
Understanding Surgical Fellowship Pathways in Urology
For many residents, completing a urology residency is only the beginning. As surgical techniques become more sophisticated and patient expectations rise, subspecialty training through a surgical fellowship has become increasingly common—and in some career paths, practically essential.
This guide walks through the major surgical fellowship options after urology residency, how they fit into the broader urology match and career trajectory, and how to decide which pathway aligns with your goals. While the focus is on the U.S. system, much of the logic and strategy also applies internationally.
We will cover:
- Why (and why not) to pursue a fellowship
- Major surgical fellowship options in urology
- How to prepare during residency
- Application strategy and competitiveness
- Career outcomes and long‑term planning
Why Pursue a Surgical Fellowship After Urology Residency?
Urology is already a highly specialized, surgery-heavy field. So why add another 1–3 years of training?
Key Reasons to Pursue a Fellowship
1. Advanced surgical skill development
Many fellowships offer concentrated exposure to complex, high-volume cases:
- Oncology: post-chemotherapy retroperitoneal lymph node dissection (RPLND), IVC thrombectomy, complex nephrectomies
- Robotics/minimally invasive: multi-quadrant robotic procedures, intracorporeal urinary diversions
- Female/reconstructive: urethral reconstruction, complex incontinence and pelvic organ prolapse repairs, fistula repair
- Andrology: penile prostheses, complex Peyronie’s disease surgery, microsurgical varicocele and vasectomy reversal
- Pediatrics: complex hypospadias, pediatric reconstructive work, minimally invasive pediatric oncology
Fellowship training allows you to reach a surgical volume and complexity in a focused area that would be difficult to achieve in a general urology residency alone.
2. Academic and research career preparation
If you aim for an academic career, a fellowship is often de facto required. Benefits include:
- Protected research time (clinical, translational, or basic science)
- Mentorship from established subspecialists
- Early publications, grant exposure, and opportunities to present at national meetings
- Networking within your subspecialty community
In many departments, major academic positions in oncologic urology, female pelvic medicine, reconstruction, pediatrics, and andrology are almost exclusively filled by fellowship-trained surgeons.
3. Differentiation in a competitive job market
In some geographic areas and large group practices, fellowship training is a key differentiator in:
- Securing positions in major health systems
- Becoming the go-to surgeon for a specific niche (e.g., complex urinary reconstruction)
- Negotiating for OR time, equipment (robotic platforms, lasers, microscopes), and institutional support
4. Personal interest and professional satisfaction
Fellowship can allow you to align your day-to-day clinical practice with what you most enjoy:
- Do you love big, technically demanding cases? Oncologic or reconstructive fellowships might fit.
- Do you prefer office-based procedures and longitudinal relationships? Andrology or some FPMRS practices may align better.
- Are you energized by pediatric patients and family-centered care? Pediatric urology may be ideal.
Reasons You Might Not Need a Fellowship
Fellowship is not mandatory for everyone. A general urologist can have an excellent, fulfilling career:
- In many community practices, broad generalist training is valued more than niche specialization.
- If you’re aiming for a smaller community, there may be less demand for an extremely narrow surgery subspecialty.
- Some residents prefer to enter practice earlier for financial, geographic, or family reasons.
Ask yourself:
- What kind of cases do I want to be doing 5–10 years from now?
- Do I want my identity to be “urologist” or “urologic oncologic surgeon,” “reconstructive surgeon,” etc.?
- In the markets I’m considering, do employers favor generalists or subspecialists?
Major Surgical Fellowship Options in Urology
Most urology fellowships fall under a few broad categories. Some are ACGME-accredited; others are non-ACGME, but nationally recognized and often aligned with organizations like SUO or GURS.
Below are the major pathways, their typical structure, and the types of careers they support.

1. Urologic Oncology Fellowship
Focus: Cancer surgery of the kidney, ureter, bladder, prostate, testis, and adrenal gland.
Typical length: 2–3 years (often 1–2 years clinical, 1–2 years research)
Accreditation: Many are Society of Urologic Oncology (SUO)-accredited; some also ACGME-accredited.
Clinical exposure:
- Open and minimally invasive (laparoscopic, robotic) nephrectomies and partial nephrectomies
- Radical and nerve-sparing cystectomies with urinary diversion (ileal conduit, neobladder)
- Advanced prostate cancer surgery (robotic or open radical prostatectomy, salvage surgery)
- RPLND for testicular cancer, including post-chemo cases
- Adrenalectomy for oncologic indications
- Management of complex, oligometastatic, or recurrent disease
Research opportunities:
- Clinical trials (systemic therapies, perioperative approaches)
- Outcomes research, quality of life, big data and registry-based work
- Translational research in tumor biology, immuno-oncology, biomarkers
Career pathways:
- Academic oncologic urologist at tertiary or quaternary centers
- Hybrid community–academic roles, often in NCI-designated centers
- Leadership roles in cancer centers or multidisciplinary tumor boards
Who it’s best for: Residents who enjoy big cases, complex decision-making, and multidisciplinary care. This is a cornerstone surgical oncology fellowship within urology.
2. Endourology and Minimally Invasive / Robotic Surgery Fellowships
Focus: Advanced stone disease, BPH procedures, and minimally invasive approaches (laparoscopic and robotic) for benign and malignant conditions.
Typical length: 1–2 years
Accreditation: Often associated with the Endourological Society; some are ACGME-accredited minimally invasive urology fellowships.
Clinical exposure:
- Complex percutaneous nephrolithotomy (PCNL), including mini-PCNL and endoscopic combined intrarenal surgery (ECIRS)
- Ureteroscopy with laser lithotripsy for complex stone burdens
- Holmium laser enucleation of the prostate (HoLEP) and other laser BPH procedures
- High-volume robotic surgery (prostatectomy, partial nephrectomy, pyeloplasty, sacrocolpopexy, simple and radical nephrectomy)
- Single-port and other advanced robotic techniques in some centers
Research opportunities:
- Technology-driven projects (new lasers, scopes, stone analysis, robotics)
- Perioperative outcomes and quality improvement
- Cost-effectiveness and health services research
Career pathways:
- High-volume robotic surgeon or stone specialist in academic or large group practice
- Director of stone center or minimally invasive program
- Industry collaboration and device development
Who it’s best for: Residents who love technology, robotics, complex stone and BPH management, and who aspire to be technical experts in minimally invasive urologic surgery.
3. Female Pelvic Medicine & Reconstructive Surgery (FPMRS)
Focus: Pelvic organ prolapse, urinary incontinence, voiding dysfunction, and reconstructive pelvic surgery, often shared between urology and gynecology.
Typical length: 2–3 years
Accreditation: ACGME-accredited FPMRS programs (available to both urologists and OB/GYN graduates).
Clinical exposure:
- Surgical management of stress urinary incontinence (sling procedures, urethral bulking)
- Advanced pelvic organ prolapse repair (vaginal, robotic, and abdominal approaches)
- Complex fistula repair (vesicovaginal, urethrovaginal)
- Neurogenic bladder and urinary diversion for benign indications
- Urethral diverticulum, urethral reconstruction in women
- Non-surgical management of pelvic floor dysfunction
Research opportunities:
- Pelvic floor biomechanics and imaging
- Quality of life, patient-reported outcomes, and sexual function
- Comparative effectiveness of surgical vs non-surgical therapies
Career pathways:
- Academic FPMRS urologist or urogynecologist
- Multidisciplinary pelvic floor center roles
- Community practices specializing in incontinence and prolapse
Who it’s best for: Those interested in functional outcomes, complex pelvic anatomy, and a mix of OR and clinic. Often attractive to residents who enjoy continuity of care and a strong quality-of-life focus.
4. Genitourinary Reconstructive Surgery (GURS)
Focus: Complex urethral stricture disease, urinary diversion, trauma, and gender-affirming surgery (in some programs).
Typical length: 1–2 years
Accreditation: Non-ACGME, with many programs associated with the Society of Genitourinary Reconstructive Surgeons (GURS).
Clinical exposure:
- Anterior and posterior urethral reconstruction (anastomotic, substitution, buccal grafts)
- Management of radiation and iatrogenic urethral strictures
- Revision of urinary diversion and stoma complications
- Management of incontinence in men, including artificial urinary sphincter placement
- Penile and genital reconstruction after trauma or cancer
- Gender-affirming genital surgery in select programs
Research opportunities:
- Outcomes research in urethral reconstruction and incontinence
- Quality of life, sexual function, and patient satisfaction
- Surgical technique innovation and flap/graft development
Career pathways:
- Academic reconstructive urologist
- Reconstructive referral center within large practice networks
- Trauma-focused or veterans’ health system roles
Who it’s best for: Residents who are technically oriented and enjoy meticulous, tissue-based surgery with major functional implications for patients.
5. Andrology and Men’s Health
Focus: Male infertility, sexual medicine, and men’s health across the lifespan.
Typical length: 1–2 years
Accreditation: Typically non-ACGME; recognized by the Sexual Medicine Society of North America (SMSNA) and the Society for the Study of Male Reproduction.
Clinical exposure:
- Microsurgical varicocelectomy
- Micro-TESE and other advanced sperm retrieval techniques
- Vasectomy reversals and complex redo reversals
- Penile prosthesis and complex Peyronie’s disease surgery
- Penile and testicular trauma management
- Hormonal evaluation and management, low testosterone, and metabolic men’s health
Research opportunities:
- Outcomes of fertility interventions and microsurgery
- Novel treatments for erectile dysfunction and Peyronie’s disease
- Hormonal and metabolic aspects of men’s health
Career pathways:
- Academic andrology and male infertility specialist
- Men’s health center director
- Hybrid practice combining andrology with general urology or oncology
Who it’s best for: Residents drawn to microsurgery, longitudinal patient relationships, and a mix of office- and OR-based practice.
6. Pediatric Urology
Focus: Surgical and non-surgical management of genitourinary conditions in infants, children, and adolescents.
Typical length: 2 years (ACGME-accredited)
Accreditation: ACGME Pediatric Urology fellowships.
Clinical exposure:
- Hypospadias repair (primary and reoperative)
- Vesicoureteral reflux management (endoscopic and surgical)
- Reconstruction for congenital urologic anomalies (e.g., bladder exstrophy, cloacal anomalies)
- Pediatric oncology cases (Wilms tumor, neuroblastoma with GU involvement)
- Pediatric stone disease and minimally invasive approaches
- Disorders of sex development and multidisciplinary care
Research opportunities:
- Congenital anomaly outcomes and long-term follow-up
- Pediatric quality of life and psychosocial outcomes
- Surgical innovation in minimally invasive pediatric urology
Career pathways:
- Academic pediatric urologist at children’s hospitals
- Regional pediatric urology referral centers
- Leadership roles in multidisciplinary pediatric subspecialty clinics
Who it’s best for: Residents who enjoy working with children and families, complex congenital anatomy, and longitudinal care from infancy through adolescence.
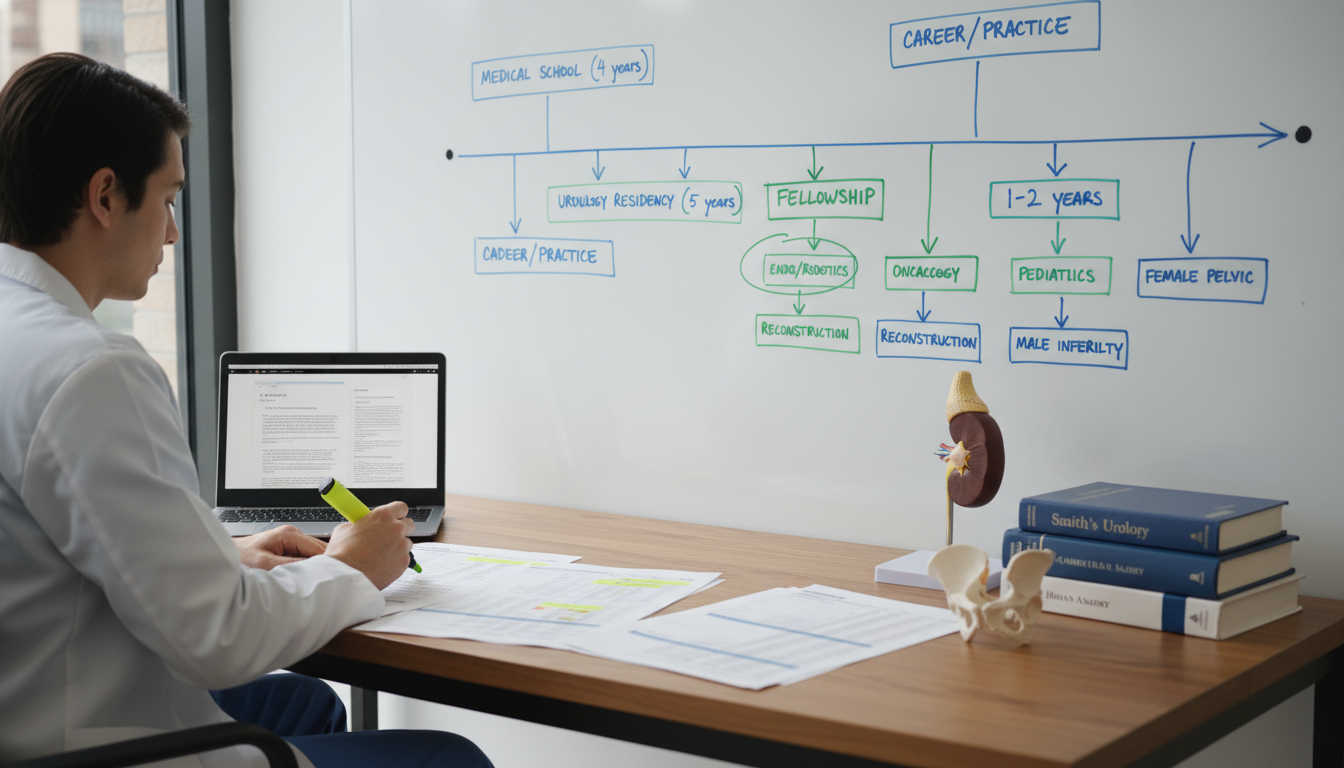
Timeline: From Urology Match to Fellowship Application
Understanding the training sequence helps you plan early.
Training Sequence Overview
Medical school → Urology residency match
- Most U.S. urology programs participate in a separate urology match (early NRMP match).
- Residency usually lasts 5–6 years (including preliminary surgical year).
Urology residency (PGY-1 to PGY-5/6)
- First 1–2 years: general surgery rotations + basic urology
- Middle years: increasing operative responsibility
- Senior years: chief responsibilities, complex cases, and elective time
Fellowship application window
- Many residents apply in PGY-4 (occasionally early PGY-5 for longer residencies).
- Timelines vary by subspecialty and by whether a centralized match exists.
Surgical fellowship (1–3 years)
- Highly focused clinical and/or research training.
Post-fellowship career
- Academic, hybrid, or community roles depending on subspecialty and personal goals.
Key Milestones During Residency
PGY-1 to Early PGY-2: Exploration
- Focus on solidifying your performance in the urology residency.
- Rotate broadly: stones, oncology, pediatrics, FPMRS, reconstruction.
- Keep an open mind about different surgery subspecialty options.
- Start informal conversations with faculty about their careers and fellowships.
PGY-2 to PGY-3: Direction and Early Preparation
- Identify what cases and clinical scenarios you find most satisfying.
- Seek mentors in areas you might consider for fellowship.
- Begin small research projects or case series with relevant faculty.
- Attend at least one national meeting (AUA, subspecialty meetings if possible).
PGY-3 to early PGY-4: Commitment and Application Prep
- Narrow down 1–2 fellowship areas of interest.
- Increase your involvement in subspecialty clinics and OR blocks.
- Work toward abstracts/posters related to your chosen area.
- Update your CV, draft a personal statement, and confirm letters of recommendation.
PGY-4: Application and Interviews
- Apply according to the subspecialty timeline (SUO match, SF Match, or direct application).
- Attend interviews (often clustered in the fall/winter).
- Rank programs if a match is used; otherwise, respond promptly to offers.
PGY-5 and Beyond: Finalizing Skills and Transition
- If matched, shape your elective time to strengthen skills for your chosen fellowship.
- Wrap up research projects and publications.
- Work with your mentor on long-term career planning and positioning for academic or private practice roles post-fellowship.
Competitiveness, Program Selection, and Application Strategy
With more residents pursuing advanced training, fellowship spots in certain areas—especially urologic oncology and pediatric urology—can be competitive. Strategy matters.
Factors That Influence Fellowship Competitiveness
1. Clinical performance and evaluations
Strong operative skills, mature intraoperative judgment, and reliability are essential. Fellowship directors often contact your program leadership informally to ask:
- Are you safe in the OR?
- Are you a team player?
- Will you represent our program well academically and professionally?
2. Research profile
Not every fellowship requires a heavy research background, but it helps:
- Highly academic fellowships (urologic oncology, pediatric urology at top centers) often expect:
- Multiple first- or co-author publications
- National meeting presentations
- Evidence of sustained academic interest
- More clinically focused fellowships (some endourology, andrology, GURS) may weigh clinical skills and fit more heavily, but scholarly work is still a plus.
3. Letters of recommendation
Target:
- 1–2 letters from subspecialists in your intended field
- 1 from your program director or chair
- Possibly an additional letter from a research mentor if separate
Specificity matters more than prestige. Programs value letters that detail your operative skills, integrity, growth trajectory, and collegiality.
4. Fit with program strengths
Each fellowship has a “personality” and emphasis:
- High-volume, technically focused vs research-intense
- Robotic-heavy vs open/reconstructive
- Benign vs oncologic case mix
Your application should clearly state why their particular structure aligns with your goals.
Choosing the Right Fellowship Program
When comparing programs, consider:
- Case volume and complexity: Do fellows get meaningful primary surgeon experience?
- Fellow autonomy: Are you operating independently under supervision, or mostly assisting?
- Research infrastructure: Is there real support—data managers, statisticians, lab resources—or just lip service?
- Mentorship and track record: Where have prior fellows gone (academia vs private practice)? Do graduates succeed in the type of career you envision?
- Culture and support: How are fellows treated by faculty and staff? How is work–life balance?
- Location and personal considerations: Proximity to partner/family, cost of living, schools, and support systems.
Application Tips and Common Pitfalls
Do:
- Start early: at least 6–9 months before the application deadline.
- Tailor your personal statement to your chosen subspecialty.
- Be honest about your goals: academic vs community, research vs primarily clinical.
- Practice subspecialty-specific interview questions (e.g., controversies in BPH surgery, emerging bladder cancer therapies, ethics in pediatric GU surgery).
Avoid:
- Applying to a highly research-focused surgical oncology fellowship if you have little interest in research.
- Overemphasizing operative volume without demonstrating reflection, critical thinking, or interest in outcomes.
- Applying reflexively because “everyone else is doing a fellowship”—lack of clear motivation can show.
Career Outcomes: Life After a Urology Surgical Fellowship
Your choice of fellowship has long-term implications for your professional life, but there is also flexibility. Many fellowship-trained urologists blend subspecialty and general practice.
Academic vs Community vs Hybrid Practice
Academic practice:
- Common for urologic oncology, pediatric, FPMRS, and GURS fellowship graduates.
- Expect:
- Higher research and teaching obligations
- Subspecialized referral practice with complex cases
- Opportunities for leadership, grants, and national committee work
- Trade-offs often include lower early earning potential than busy private practice, but higher institutional support and prestige.
Community or private practice:
- Very feasible for endourology, andrology, and many GURS and FPMRS graduates.
- You might:
- Serve as the regional specialist in stones, robotics, reconstruction, or men’s health
- Combine subspecialty referrals with a base of general urology
- Have more control over schedule and potentially higher earnings, depending on the market
Hybrid roles:
- Many large health systems offer positions where you:
- Have academic titles and teaching responsibilities
- Practice within a “community-academic” environment
- Run subspecialty clinics while sharing general call and bread-and-butter urology
Flexibility and Evolving Interests
Your fellowship choice does not permanently lock you into a single niche, but it strongly nudges your trajectory. For example:
- A urologic oncologist can still do benign robotic surgery and some endourology.
- An andrologist may maintain a general urology practice while building a niche men’s health program.
- A reconstructive urologist can overlap with FPMRS, trauma, or oncology reconstruction.
Look for programs where graduates demonstrate a range of satisfying careers; that’s evidence the training equips you for multiple paths.
Putting It All Together: Actionable Steps for Residents
Early residency (PGY-1–2):
- Rotate broadly and reflect on which cases energize you.
- Start a simple research project with an interested mentor.
Mid-residency (PGY-2–3):
- Narrow to 1–2 potential surgery subspecialty interests.
- Attend national or regional meetings and talk to fellows and faculty informally.
- Build your CV with at least a few presentations or publications.
Later residency (PGY-3–4):
- Choose a primary subspecialty target and a backup that you would genuinely enjoy.
- Identify 3–4 letter writers and give them plenty of notice.
- Apply strategically to programs whose strengths match your goals.
During interviews:
- Ask detailed questions about case logs, autonomy, research support, and graduate outcomes.
- Assess program culture and whether you can see yourself thriving there.
Before fellowship starts:
- Use your final residency year to fill experience gaps you’ll need for fellowship success (e.g., more open cases before an oncologic fellowship, or more endoscopic work before endourology).
Frequently Asked Questions (FAQ)
1. Do I have to decide on a surgical fellowship during medical school when I apply for urology residency?
No. When entering the urology match, you do not need to have your fellowship plans fixed. Most residents solidify their interest in a particular surgical fellowship during PGY-2 or PGY-3, after adequate exposure. Programs may ask about your interests, but they also know interests can evolve.
2. Can I have a successful community urology career without a fellowship?
Yes. Many urologists practice broad-based general urology without fellowship and have excellent careers. In smaller or more rural communities, generalists are indispensable. Fellowship becomes more advantageous if you:
- Want an academic or tertiary-care role
- Aspire to be a high-volume surgeon in a particular niche
- Plan to practice in competitive urban markets where subspecialty training differentiates you
3. Is it possible to change subspecialties after fellowship (for example, do oncology after an endourology fellowship)?
You can adjust your practice mix over time, but formal re-specialization is limited. A fellowship in one area equips you best for that core domain, but you may still perform general urology and related subspecialty work. For instance, an endourologist who loves robotics may handle benign robotic oncology cases. However, becoming a recognized tertiary-quaternary urologic oncologist after a non-oncology fellowship is challenging without additional structured training.
4. How important is research for getting into a competitive urology surgical fellowship?
Research is important, particularly for academically oriented fellowships (urologic oncology, pediatric urology at major centers, research-heavy FPMRS or GURS). Programs look for:
- Evidence of curiosity and follow-through (projects that reach presentation or publication)
- Comfort interpreting literature and designing studies
- Alignment between your academic interests and their program strengths
For more clinically focused fellowships, a modest research portfolio plus strong operative and interpersonal skills may be sufficient. However, having no scholarly activity at all can significantly limit your options.
Surgical fellowship pathways in urology offer powerful ways to deepen your expertise, shape your surgical identity, and align your career with what you enjoy most. By understanding the major options, planning ahead during residency, and applying strategically, you can position yourself for a rewarding role within the evolving landscape of urologic surgery.






















