
Understanding Urology Residency Work Hours and Why They Matter
Urology is an intellectually demanding, procedure-heavy specialty with substantial time in the operating room, consults, and continuity clinic. For many applicants, the urology residency work hours and how they affect resident work life balance are central to specialty choice.
In the United States, urology residents are typically bound by the ACGME duty hour regulations (even though the urology match is separate and earlier than the NRMP). Most programs adhere to the following core rules:
- 80-hour workweek, averaged over 4 weeks
- 1 day off in 7, free of all clinical duties, averaged over 4 weeks
- In-house call no more frequently than every 3rd night, averaged over 4 weeks
- Maximum shift length: usually 24 hours of in-hospital duties plus 4 hours for transitions and education (no new patients in the last 4 hours)
- Adequate time off between shifts (often 8–10 hours minimum depending on program)
Yet the lived reality is more nuanced. The intensity and structure of urology residency work hours vary across:
- PGY level (junior vs senior)
- Academic vs community programs
- Trauma level and hospital volume
- Call structure (home call vs in-house, night float vs 24-hour call)
Understanding this landscape is step one in learning how to manage your time, energy, and well-being in urology residency.
Why duty hours are especially important in urology
Urology has unique features that make duty hours and fatigue management especially critical:
- High operative volume: Long days in the OR demand sustained concentration and fine motor control.
- Frequent emergencies: Ureteral obstruction, testicular torsion, urosepsis, and trauma can require immediate attention, often overnight.
- Procedural diversity: Endoscopy, robotics, open surgery, minor procedures, and clinic-based interventions require rapid task-switching.
- Early autonomy: Residents may gain hands-on experience early; fatigue can directly affect skill acquisition and performance.
Residents must therefore manage not just time, but cognitive bandwidth and physical stamina. Learning to work efficiently within your duty hours is as important as any clinical skill you’ll acquire.
Typical Urology Residency Schedule: What to Expect by Year
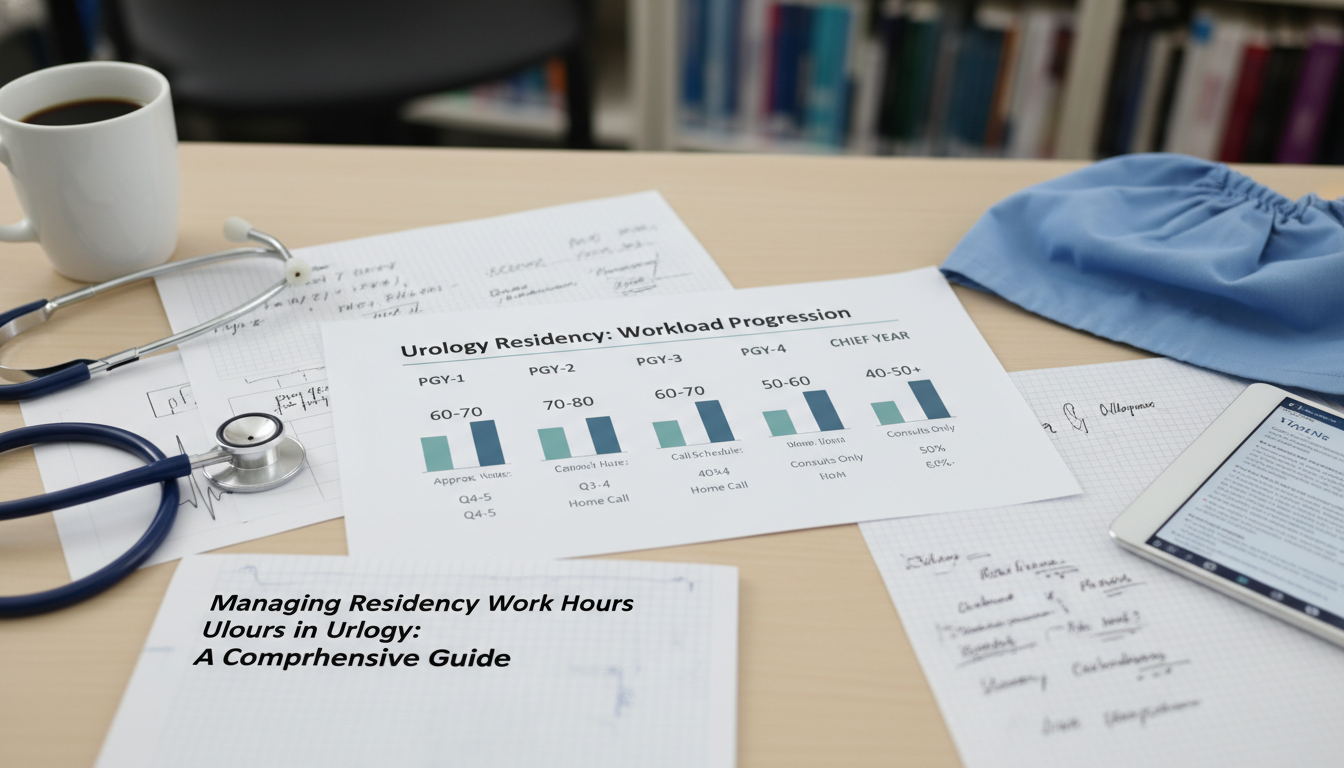
While programs differ, most follow a progression from heavy floor/consult responsibilities early on to more OR time and leadership later.
PGY-1: Foundational surgical year
Many urology residents spend much of PGY-1 on general surgery and surgical subspecialty rotations with a smaller portion on urology itself.
Common features:
- Work hours: Often near the upper range of the 80-hour limit, especially on busy general surgery services.
- Early arrival (5:30–6:00 a.m.) for pre-rounds and sign-out.
- Long operative days, especially on trauma or acute care surgery.
- Night float or q4 call depending on the program.
Your primary goals:
- Learn hospital workflows, order entry, perioperative care, and basic consult management.
- Build stamina while staying attentive to signs of fatigue and burnout.
- Develop core time-management skills you will refine later.
PGY-2 to PGY-3: The heavy urology years
These are often the most intense years in terms of urology residency work hours and cognitive load:
- More time on dedicated urology services
- Large consult volume (ED, floor, ICU)
- Frequent urgent procedures: stent placements, nephrostomy exchanges (with IR), scrotal explorations, emergent decompressions
- In-house or home call with frequent phone calls and returns to the hospital
On a busy service, your schedule may look like:
- Weekdays: 60–70 hours
- Weekends: Call every 2–3 weekends, depending on program
- Typical day: 6:00 a.m.–6:00/7:00 p.m. on non-call days; 24+4 hours on call days, with post-call days often still involving administrative tasks and checkout
These years demand the most intentional strategies for:
- Task triage and efficient rounding
- Managing consults without bottlenecks
- Handing off effectively to preserve your own recovery time
PGY-4 to PGY-5 (or PGY-6): Senior and chief years
As a senior resident, you often experience:
- More time in the operating room and subspecialty rotations (oncology, reconstructive, pediatrics, female pelvic medicine)
- Higher-level planning rather than minute-to-minute paging
- Leadership roles: supervising juniors and advanced practice providers, managing service flow, teaching students
Work hours may feel more predictable, but responsibilities are broader:
- You may have some flexibility in start/stop times when cases allow.
- You’re often involved in program-level decisions about call schedules, coverage, and resident work life balance.
- You must model professional behavior around duty hour compliance and safe cross-coverage.
Key Duty Hour Rules in Practice: Navigating the Gray Zones
Understanding policy is one thing; applying it in real life is another. Here’s how common duty hour principles play out in urology.
80-hour workweek: Averaged reality
The 80-hour cap is averaged over 4 weeks, which means:
- One extremely heavy week can be balanced by a lighter week later, as long as the 4-week average ≤ 80 hours.
- Many residents track this with personal apps or spreadsheets to avoid surprises.
Practical example:
You have three weeks at ~78 hours and one lighter week at ~60 hours.
Average = (78 + 78 + 78 + 60) / 4 = 73.5 hours → compliant.
Actionable tip:
- Keep your own log. When you’re approaching sustained 80+ weeks, speak up early to your chief or program leadership.
24+4 rule and overnight call
In urology, overnight call is common—especially to cover:
- Ureteral stones and urinary retention
- Testicular torsion
- Urologic trauma
- Post-op complications
The 24+4 rule generally works as:
- Up to 24 hours of in-house clinical duty (e.g., 7 a.m.–7 a.m.)
- Up to 4 additional hours for transitions of care, documentation, and education (e.g., sign-out, brief teaching sessions)
- No new patients during the last 4 hours
In practice:
- You might leave anywhere between 9–11 a.m. post-call, depending on workload and program culture.
- You should not be starting another elective case after the 24-hour point.
Actionable tip:
- During call, cluster documentation (e.g., write notes after finishing a block of consults) to avoid staying unnecessarily late in the post-call period.
- Hand off tasks that can safely wait to the day team instead of trying to “clear the list” beyond your legal hours.
Days off and “soft” pressure
You’re entitled to one day in seven free of all clinical responsibilities, averaged over 4 weeks.
Common gray-zone issues:
- Being asked to “just log in briefly” to review labs or imaging on your day off.
- Informal expectations to show up for big operative cases or conferences despite being post-call or on your “off” day.
How to navigate:
- Know your program’s and ACGME’s definitions: a day off is a full, continuous 24-hour period with no required clinical activity.
- Voluntary educational activities (e.g., optional journal clubs) may be permitted, but you should never feel coerced.
Actionable scripts:
- “I’m actually on my day off for duty hour reasons. If it’s urgent and needs immediate attention, can the on-call resident or attending cover it?”
- “I’d love to scrub if I can do so within duty hour limits; can I join for the first part of the case and sign out at [time]?”
Home call vs in-house call
Urology frequently uses home call, especially at senior levels, for programs where urgent cases require quick response but not constant in-house presence.
Key points:
- Time spent in the hospital during home call counts toward the 80-hour limit.
- Time at home but actively engaged in patient care (e.g., extended phone management) often also counts as work; check your program’s policy.
- If home call consistently becomes in-house-level workload, it may need to be reclassified.
Actionable tip:
- Document heavy home call nights (time of pages, time in hospital). If patterns emerge, share them with your chiefs or PD—this can improve scheduling for everyone.
Strategies to Manage Urology Residency Work Hours Day-to-Day
Managing resident work life balance in urology is about more than just leaving on time; it’s about working smart and making the most of your limited time and energy.
1. Master pre-rounding and efficient data gathering
Morning pre-rounds can make or break your day.
Practical workflow for floor patients:
- Batch EHR review: Look at labs, imaging, overnight events, and vitals for all urology inpatients before seeing anyone.
- Prioritize visits: See sickest and soonest-to-OR patients first.
- Standardize notes: Use templates with checklists for urologic issues (e.g., catheter status, drain outputs, imaging follow-up, cultures and sensitivities).
- Pre-empt orders: Place obvious orders (e.g., NPO status, imaging re-checks, voiding trials) during or immediately after rounds to prevent afternoon bottlenecks.
Time-saving example:
Instead of walking back to the workstation after every patient, jot down notes and enter all orders in one focused block, whenever possible.
2. Triage consults with a clear mental framework
Consults are a major source of time pressure in urology.
Use a structured triage approach:
- Emergent: Testicular torsion, obstructed infected kidney (pyelonephritis with obstruction), urosepsis, trauma with active bleeding, acute urinary retention with instability
- Urgent: Obstruction without infection, hematuria with clots and significant anemia, complicated catheter issues
- Routine: Stable urinary retention, uncomplicated hematuria in stable patients, elective pre-op clearance questions
Actionable tips:
- When paged, ask: “What are the vitals, labs, imaging, and main concern?” before running to the bedside—this can save multiple trips.
- For non-emergent consults at odd hours, coordinate with your attending regarding timing: some can safely wait until early morning.
3. Optimize your OR days
OR days are long and cognitively intense but can be more predictable.
Strategies:
- Review the case list the night before; anticipate positioning, equipment, and potential complications.
- Eat and hydrate before long robotic or endourologic cases. Plan micro-breaks (even 60–90 seconds) when safe.
- Use downtime (while scrubbing or waiting) to close small loops: quick note sign-offs, answering non-urgent pages, clarifying plans with nursing.
Protect your post-call and post-OR evenings:
- Avoid the perfectionist trap of “just finishing everything” before leaving. Hand off logically and document what’s pending.
4. Communicate proactively with your team
Many duty hour challenges are solvable with earlier communication.
Examples:
- At noon, tell your chief: “We have 6 new consults and 4 discharges left. I’m post-call tomorrow and may hit my hour limit if I stay past 9 p.m.”
- Coordinate with co-residents: “I’ll handle all ED consults until 4 p.m.; can you cover floor issues, then we swap?”
Good communication ensures that:
- No single resident quietly absorbs an unsustainable workload.
- Attending surgeons understand when a case start time might be unrealistic given overnight volume.
5. Use technology wisely, not compulsively
EHRs, secure messaging apps, and scheduling platforms can either save or steal time.
Productive uses:
- Smart phrases and templates for common consults: stones, retention, hematuria, elevated PSA.
- Task lists in the EHR or on a secure app to track labs, imaging, and follow-ups.
- Calendar reminders for important, but non-urgent items (e.g., check cytology results in 48 hours).
Avoid:
- Constantly checking non-urgent messages on your day off.
- Responding to every notification instantly instead of batching communication.

Protecting Resident Work-Life Balance in a Demanding Specialty
Urology attracts driven, detail-oriented individuals who often overextend themselves. Sustaining performance over 5–6 years requires protecting your physical, mental, and relational health.
Sleep: Your most important “procedure”
Inconsistent, abbreviated sleep is one of the biggest threats to both clinical performance and well-being.
Strategies:
- Anchor sleep: Try to maintain at least one consistent anchor in your schedule—e.g., always sleep from 11 p.m.–4:30 a.m. on non-call days.
- Strategic napping:
- 20–30 minutes before a known long call night.
- 60–90 minutes immediately after call if you must be up for an event later (e.g., conference).
- Sleep hygiene post-call:
- Dark, cool room; consider blackout curtains or eye mask.
- Avoid heavy caffeine within 6–8 hours of planned sleep.
- Use a brief transition routine (shower, light snack) to signal your body it’s time to rest.
Physical health: Minimal investment, maximal return
You do not need an elaborate fitness routine; you need consistency.
Realistic approaches:
- 20–30 minutes of moderate exercise 3–4 times per week: brisk walking, short runs, bodyweight circuits, or resistance bands.
- Micro-workouts: 10 minutes of stretching or light cardio between shifts can reduce musculoskeletal strain from OR postures.
- Plan “easy wins”: keep healthy snacks (nuts, yogurt, fruit, protein bars) available to avoid surviving on vending machine options.
Mental health: Normalize asking for help
Urology residency is emotionally taxing: cancer diagnoses, postoperative complications, emergencies involving children, fertility issues.
Protective practices:
- Debrief major events with a senior resident or trusted attending.
- Use institutional mental health resources or employee assistance programs early.
- Maintain at least one non-medical hobby or interest—even 30 minutes a week can preserve your identity outside the hospital.
Red flags that your work hours and stress are unsustainable:
- Persistent insomnia or nightmares
- Emotional numbness or frequent tearfulness
- Irritability with patients or team members
- Loss of interest in urology or thoughts of leaving medicine entirely
These warrant immediate discussion with a mentor, chief resident, or program leadership.
Relationships and boundaries
Long residency work hours can strain personal relationships. Proactive communication helps:
- Share your typical weekly structure and call schedule with partners, family, and friends.
- Schedule protected time in advance (e.g., monthly dinner, half-day off activities).
- Learn to say no to optional commitments when you are in a heavy call block.
Example boundary statement:
“These next two weeks I’m on q3 call, so I might be less available. After that, I’d love to commit to [specific plan] on my golden weekend.”
Evaluating Residency Work Hours When Applying to Urology Programs
As an applicant in the urology match, you can and should gather specific information about duty hours and work-life balance at each program.
Questions to ask (and how to interpret answers)
Ask residents—not just faculty—questions like:
“How often do you hit the 80-hour limit?”
- Occasional stretches during heavy rotations are normal.
- Chronic 80+ hours across most rotations is a red flag.
“What is the call structure for juniors and seniors?”
- q3 in-house call for juniors is common at busy centers; ask how they protect post-call time.
- Night float systems may offer more predictability but can be socially isolating.
“How is duty hour compliance monitored, and how does leadership respond to concerns?”
- Look for: openness, encouragement to report honestly, actual changes made in response to past issues.
“How often do you realistically get a full day completely off?”
- A healthy program: most residents get weekly days off, with rare exceptions for unique circumstances.
“What changes have been made in the last 2–3 years to improve resident work life balance?”
- Strong programs can cite concrete examples: additional APP support, revised call systems, improved handoff processes.
Subtle signs of program culture
During interviews and away rotations, observe:
- Do residents appear consistently exhausted or disengaged?
- Do they have time for brief teaching and discussion, or is everything “on the fly”?
- How do attendings talk about residents: as learners and colleagues, or as workforce?
- Are residents able to leave on time post-call, or do they routinely scrub into late cases?
Remember: program culture determines how duty hour rules are applied in real life.
Balancing training intensity and sustainability
You want a program that:
- Challenges you clinically and technically;
- Exposes you to high surgical volume and acuity;
- Still protects your ability to learn safely, maintain health, and grow as a person.
When ranking programs in the urology match, consider:
- Are the work hours acceptable for you for 5–6 years?
- Do you feel you can thrive, not just survive, in that environment?
- Do residents ahead of you seem to be successful and reasonably satisfied?
Frequently Asked Questions About Managing Urology Residency Work Hours
1. Do urology residents really work close to 80 hours every week?
It depends on the program, rotation, and PGY level. On very busy services—especially early urology years and certain general surgery rotations—weeks may approach the 80-hour maximum. Other rotations (e.g., some electives or research blocks) can be significantly lighter, bringing the 4-week average down. When considering programs, ask about specific rotations known to be heavy and what protections are in place for resident rest.
2. How can I prepare during medical school for the work hours in urology residency?
You can’t fully simulate residency hours, but you can build habits that will help:
- Practice efficient pre-rounding and note writing on sub-internships.
- Develop basic personal systems: digital task lists, calendar management, and simple meal-prep strategies.
- Learn your own sleep needs and how to function safely on variable schedules.
- Do at least one sub-I or away rotation in a surgical specialty to experience early mornings and longer days.
3. Is it okay to speak up about duty hour violations, or will it hurt my evaluation?
ACGME and program leadership are obligated to protect residents who report duty hour issues. Most departments want accurate data to make improvements. Approach concerns professionally:
- Start with your chief or rotation director.
- Present specific examples and suggestions.
- Emphasize patient safety and educational value, not just personal comfort.
If local discussions fail, you can escalate via program leadership, GME office, or anonymous surveys—these are taken seriously, especially during accreditation reviews.
4. Can you have a reasonable work-life balance and a family in urology residency?
Yes, many residents successfully have partners, families, and children during urology training. The key is planning and communication:
- Choose a program with a culture supportive of parental leave, flexible scheduling during major life events, and coverage help when needed.
- Coordinate call schedules and childcare with your partner or support network.
- Accept that some periods (e.g., heavy call blocks) will be more challenging, but life can be structured to protect meaningful time with family overall.
Managing residency work hours in urology is a continuous skill—one that evolves as you progress from novice intern to confident chief. By understanding duty hour rules, applying concrete time-management tactics, and evaluating programs thoughtfully during the urology match, you can build a career that is both technically excellent and sustainably lived.






















