Understanding the Role of Addiction Medicine in USMLE Step 1
USMLE Step 1 is increasingly testing integrated, clinically relevant concepts rather than isolated facts—and substance use and addiction topics are prime examples. Even though addiction medicine fellowship training comes years later, your foundation for success in this field is built right now with your basic science knowledge and Step 1 preparation.
Why this matters for you:
- Substance use and related disorders are high-yield for Step 1 across multiple disciplines:
- Neuroanatomy and neurophysiology
- Pharmacology of drugs of abuse
- Behavioral science and psychiatry
- Biostatistics and ethics (screening, public health)
- The shift to Pass/Fail has not reduced the importance of Step 1; it has changed how it matters:
- A solid pass with strong basic science understanding makes Step 2 CK easier.
- Strong addiction-related knowledge signals interest in behavioral health specialties, including a future in addiction medicine.
This guide will walk you through:
- How addiction and substance use topics appear on Step 1
- High-yield addiction-related domains in the exam blueprint
- A practical USMLE Step 1 study plan integrating these topics
- Best Step 1 resources for mastering addiction pharmacology, neurobiology, and behavioral science
- How early attention to these areas lays groundwork for an eventual addiction medicine fellowship
Exam Blueprint: Where Addiction Medicine Shows Up on Step 1
Addiction medicine isn’t labeled as a standalone category on Step 1, but it is woven into multiple content domains tested by the exam.
1. Behavioral Science & Psychiatry
High-yield addiction-related themes:
- Substance use disorders (SUDs) diagnostic features
- Withdrawal vs intoxication syndromes for major classes of substances
- Screening, brief intervention, and referral to treatment (SBIRT) concepts
- Harm reduction principles (needle exchange, naloxone programs)
- Physician impairment, professionalism, and patient safety
Example Step 1-style scenario:
A 38-year-old physician is reported to the hospital committee for frequently missing calls and smelling of alcohol. The best next step:
- A) Immediately report to law enforcement
- B) Ignore the behavior
- C) Refer to the state physician health program
- D) Fire the physician immediately
These questions integrate ethics, professional responsibility, and addiction.
2. Pharmacology: Drugs of Abuse
This is one of the most testable addiction-related areas.
You must know for each major substance:
- Mechanism of action (especially neurotransmitters and receptors)
- Clinical features of intoxication and withdrawal
- Management of acute intoxication and withdrawal
- Long-term treatment and medications used in SUD treatment
Commonly tested substances:
- Alcohol
- Opioids (heroin, prescription opioids)
- Benzodiazepines and barbiturates
- Stimulants (cocaine, amphetamines, methamphetamine)
- Nicotine
- Cannabis
- PCP and hallucinogens (LSD, MDMA)
- Inhalants
USMLE loves comparative reasoning: distinguishing alcohol withdrawal from benzodiazepine withdrawal, or opioid intoxication from sedative intoxication.
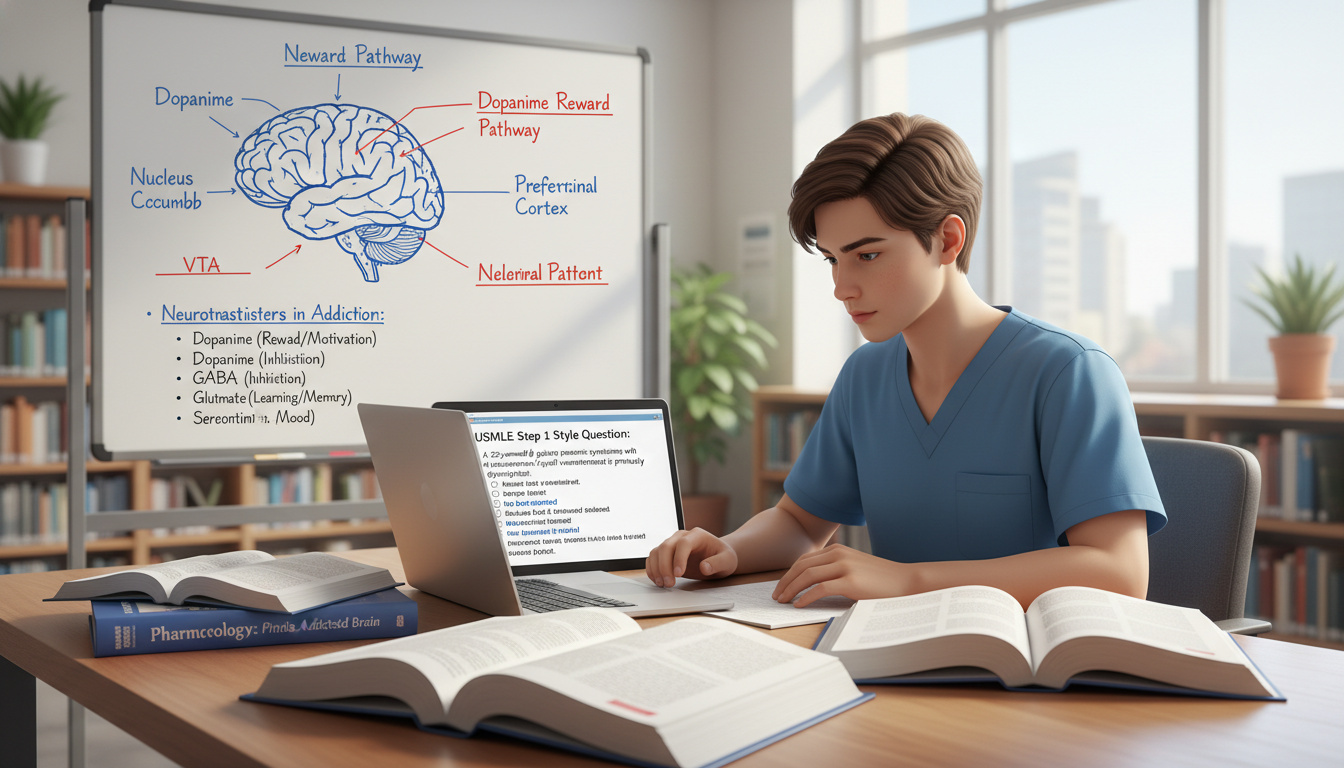
3. Neuroscience & Neuroanatomy: Reward Pathways
Addiction is fundamentally a brain circuit disorder. On Step 1 you may see:
- The mesolimbic dopamine pathway:
- Ventral tegmental area (VTA) → nucleus accumbens
- Role of dopamine in reinforcement and reward
- Prefrontal cortex involvement in impulse control and decision-making
- Neuroadaptations in chronic use (tolerance, dependence)
These concepts may appear as:
- Lesion questions involving nucleus accumbens or VTA
- Neurotransmitter questions involving dopamine in substance use
- Basic science stems translated into clinical addiction scenarios
4. Biostatistics & Public Health
Addiction medicine is highly relevant in population health questions:
- Screening tools (AUDIT, CAGE, SBIRT principles)
- Epidemiology of substance use disorders
- Public health interventions (methadone clinics, syringe programs)
- Evaluating treatment outcomes and relapse rates (sensitivity, specificity, NNT)
Knowing how to analyze screening test performance for substance use is a common testing angle.
Core Knowledge: High-Yield Addiction Topics You Must Master
1. Drugs of Abuse: Mechanisms and Clinical Syndromes
Use a structured framework for each substance:
a. Mechanism of Action
- Opioids: agonists at μ (mu) receptors → increased K⁺ efflux, decreased Ca²⁺ influx → decreased synaptic transmission
- Alcohol: enhances GABA-A, inhibits NMDA → CNS depression
- Benzodiazepines: increase frequency of Cl⁻ channel opening at GABA-A
- Barbiturates: increase duration of Cl⁻ channel opening at GABA-A
- Cocaine: blocks reuptake of NE, dopamine, serotonin
- Amphetamines: increase presynaptic release of catecholamines
- Nicotine: nicotinic ACh receptor agonist
- Cannabis (THC): partial agonist at CB1 receptors in CNS
- PCP: NMDA receptor antagonist
- LSD: complex serotonin receptor agonism (5-HT2A)
Learn these mechanisms alongside standard pharmacology content; they are integral to any good USMLE Step 1 study plan.
b. Intoxication Features
Know hallmark features that distinguish each substance:
Opioid intoxication:
- CNS and respiratory depression
- Miosis (pinpoint pupils)
- Decreased bowel sounds
- Hypotension, bradycardia
- Reversal: naloxone, naltrexone
Alcohol intoxication:
- Disinhibition, emotional lability
- Ataxia, slurred speech, nystagmus
- Coma at high levels
- Risk of respiratory depression with other sedatives
Cocaine intoxication:
- Euphoria, increased energy
- Tachycardia, hypertension
- Mydriasis (dilated pupils)
- Chest pain, arrhythmias, MI, stroke
- Risk of sudden cardiac death
Being able to rapidly identify which substance is involved from a short vignette is a classic Step 1 skill.
c. Withdrawal Syndromes
This is heavily tested because it is clinically crucial:
Alcohol withdrawal:
- 6–24 hours: tremors, anxiety, GI upset, insomnia
- 12–48 hours: seizures, hallucinations
- 48–96 hours: delirium tremens (confusion, autonomic instability, risk of death)
- Treatment: benzodiazepines (e.g., lorazepam, diazepam), thiamine
Opioid withdrawal:
- Lacrimation, rhinorrhea
- Yawning, piloerection (goosebumps)
- Diarrhea, abdominal cramps
- Mydriasis
- Body aches, restlessness
- Distressing but not typically life-threatening
Benzodiazepine/barbiturate withdrawal:
- Anxiety, tremors, insomnia
- Seizures
- Can be life-threatening
Nicotine withdrawal:
- Irritability, anxiety, increased appetite, difficulty concentrating
For Step 1, associate “life-threatening withdrawal” with alcohol and sedative-hypnotics, not opioids.
d. Treatment & Long-term Management
Even though detailed addiction therapeutics are more Step 2 CK–oriented, Step 1 expects recognition of key medication strategies:
- Alcohol use disorder:
- Naltrexone (opioid antagonist, reduces craving)
- Acamprosate (modulates glutamate/GABA)
- Disulfiram (aldehyde dehydrogenase inhibitor; aversive therapy)
- Opioid use disorder:
- Methadone (full agonist, long-acting)
- Buprenorphine (partial agonist often with naloxone)
- Naltrexone (long-acting antagonist for relapse prevention)
- Nicotine dependence:
- Nicotine replacement (patch, gum)
- Varenicline (partial agonist at nicotinic receptors)
- Bupropion (NDRI antidepressant, helps reduce craving)
These details are foundational if you later pursue an addiction medicine fellowship, but they also appear directly in test questions.
2. Neurobiology of Addiction
Step 1 will not ask you to design a treatment program, but it will test core neurobiologic mechanisms.
Key concepts:
- Reward pathway:
- Origin: Ventral tegmental area (VTA)
- Target: Nucleus accumbens (ventral striatum)
- Neurotransmitter: Dopamine
- Tolerance and dependence:
- Receptor downregulation/upregulation
- Changes in neurotransmitter release
- Conditioning and cues:
- Classical conditioning: environmental cues trigger craving via learned associations
- Operant conditioning: drug use reinforced by euphoria or relief of withdrawal
Example Step 1-style question:
A researcher lesions a brain structure in rodents that abolishes the reinforcing effects of cocaine. Which structure was most likely damaged?
Correct answer: nucleus accumbens.
Understanding these pathways also helps connect pharmacology (dopamine, GABA, glutamate) to clinical behavior, which is increasingly emphasized on Step 1.
3. Behavioral Science and Diagnostic Criteria
You do not need DSM-5 memorization for Step 1, but you must understand:
- Substance use disorder as a pattern of:
- Impaired control
- Social impairment
- Risky use
- Pharmacologic criteria (tolerance, withdrawal)
Common question themes:
- Distinguishing use, misuse, dependence, and withdrawal
- Recognizing motivational interviewing and nonjudgmental communication
- Management of patient denial or ambivalence about substance use
You may see a vignette where the “correct answer” reflects an empathic, non-confrontational statement, or one that prioritizes patient safety (e.g., assessing for withdrawal risk).
4. Public Health, Screening, and Ethics
High-yield areas:
- Screening tools:
- CAGE questions (Cut down, Annoyed, Guilty, Eye-opener)
- Understanding that positive screening requires further assessment
- Physician impairment:
- Duty to report unsafe practice to appropriate bodies (e.g., physician health programs)
- Providing help while protecting patients
- Harm reduction:
- Needle/syringe exchange programs reduce HIV/HCV transmission
- Overdose education and naloxone distribution
- Medication-assisted treatment improves outcomes
These topics are not only testable; they also mirror the real-world framework of modern addiction medicine practice.
Building Your Step 1 Study Plan with Addiction Medicine in Mind
1. Integrate, Don’t Isolate
Avoid studying addiction-related content as a detached “extra” chapter. Instead, weave it into your USMLE Step 1 preparation:
- When you study pharmacology of CNS drugs, include:
- Alcohol, benzodiazepines, barbiturates, opioids, stimulants
- Treatment of intoxication and withdrawal
- When you study neuroanatomy:
- Add diagrams of the mesolimbic dopamine pathway
- When you study behavioral science/psychiatry:
- Pair mood and anxiety disorders with substance-induced disorders
- Review SUD diagnostic principles and screening tools
This integration mirrors how the exam now tests content and will help you recall information more flexibly.
2. A Sample 4-Week Micro-Plan for Addiction Topics
Assume you already have a global Step 1 plan; here’s how to plug addiction-focused review into it:
Week 1: Foundations
- 1–2 hours: Read addiction-related sections in your main review book (e.g., First Aid)
- 1 hour: Watch a high-yield video set on:
- Drugs of abuse (pharm)
- Reward pathways (neuro)
- 50–75 Qbank questions focusing on:
- Alcohol and opioid intoxication/withdrawal
- Sedative-hypnotic pharmacology
Week 2: Deepen Pharmacology
- Build comparative tables:
- Alcohol vs benzodiazepine vs barbiturate withdrawal
- Cocaine vs amphetamine vs PCP vs LSD intoxication
- Another 75–100 Qbank questions:
- Mixed pharmacology sets filtered for substance-related content
- Flashcard creation or review for:
- Mechanism, intoxication, withdrawal, treatments for each major substance
Week 3: Neurobiology and Behavioral Science
- 1–2 hours: Review reward pathways, conditioning, and related neurophysiology
- 1 hour: Behavioral science/psychiatry videos on SUD and screening tools
- Qbank:
- 50–75 questions on psychiatric/behavioral topics including SUD
- Practice short-answer: “Explain the mechanism underlying tolerance in chronic opioid use” (helps conceptual understanding, not just memorization).
Week 4: Integration and Rapid Review
- Mixed Qbank blocks under test-like conditions (40-question timed blocks)
- After each block, tag and review:
- Any addiction-related misses
- Any question you got right by guessing
- Rapid review of your drugs-of-abuse charts and flashcards
- Final pass through Step 1 resources sections on:
- Substance use
- Neurobiology of reward
- Withdrawal/intoxication charts
By the end of this month, addiction-related material should feel like familiar territory, not a fringe subject.
Best Step 1 Resources for Addiction-Related Content
Different resources excel at different aspects of substance abuse training for Step 1. Combine them strategically.
1. Core Review Books
First Aid for the USMLE Step 1
- Compact, exam-oriented summary
- High-yield tables of intoxication/withdrawal
- Use as your “checklist” for what you must know
Board-style comprehensive texts (e.g., Step-Up, BRS Physiology/Behavioral Science)
- Helpful if your foundation is weaker in neuro/behavioral science
- Use selectively; don’t get lost in low-yield details
2. Video Lectures
Pharmacology courses (e.g., Sketchy Pharm, Boards & Beyond, Osmosis-type platforms)
- Sketches/mnemonics are extremely useful for memorizing:
- Drug classes
- Mechanisms
- Side effects
- Use spaced repetition: revisit addiction pharmacology videos multiple times
- Sketches/mnemonics are extremely useful for memorizing:
Psychiatry/Behavioral Science modules
- Good for concepts like SUD categories, screening, and ethics
- Reinforces clinical reasoning underlying case vignettes
3. Question Banks
Your USMLE Step 1 study is incomplete without intensive Qbank work.
- UWorld (gold standard)
- Prioritize:
- Psychiatry
- Neurology
- Pharmacology (especially CNS)
- Carefully read explanations for:
- Why other options were wrong
- Integrated neuroanatomy and pharmacology concepts
- Prioritize:
- NBME practice exams
- Provide the most exam-predictive addiction-related questions
- Review every SUD-related question and make notes/tables
Strategy tip:
Create an “Addiction Medicine” tag or notebook section where you collect:
- Screenshots or notes on any addiction-related question
- Patterns you repeatedly miss (e.g., confusing opioid vs sedative withdrawal)
This builds a mini-addiction medicine curriculum within your overall Qbank work.
4. Flashcards / Spaced Repetition Tools
- Use Anki decks (pre-made or custom) focused on:
- Drugs of abuse
- Reward pathways
- Withdrawal/intoxication patterns
- Aim for short, concept-focused cards:
- “Mechanism of action: methadone”
- “Classic triad of opioid intoxication”
- “Structure receiving VTA dopaminergic projections involved in reward”
Spaced repetition ensures these facts are retrievable months later, when you sit for Step 1 and when you start clinical rotations.
How Strong Step 1 Addiction Knowledge Supports a Future in Addiction Medicine
If you’re already thinking about an addiction medicine fellowship, your approach to Step 1 can set you up for a coherent long-term path.
1. Building a Strong Clinical Foundation
- Many clinical scenarios in addiction medicine hinge on:
- Pharmacology (drug interactions, withdrawal management)
- Neurobiology (understanding cognitive and behavioral changes)
- Solid Step 1 mastery makes:
- Third-year psychiatry, internal medicine, and family medicine rotations easier
- Sub-internships in addiction medicine or consult-liaison psychiatry more intuitive
2. Signaling Interest to Programs
While Step 1 is now Pass/Fail, programs still care that:
- You learned the material deeply
- You can apply it clinically (reflected later in Step 2 CK, clerkship grades, and letters)
Down the line, you can build on this interest by:
- Doing addiction-focused research (e.g., projects on withdrawal management protocols)
- Seeking electives in addiction medicine or related fields
- Presenting posters on substance-related topics at student or specialty conferences
Your early addiction-focused Step 1 preparation is the first layer of that story.
3. Avoiding Burnout and Moral Distress
Addiction cases can be emotionally complex. Understanding:
- That addiction is a chronic brain disease, not a moral failing
- The biologic basis of craving, relapse, and tolerance
helps you maintain empathy and reduces frustration as a trainee. That mindset starts now with evidence-based learning rather than stereotypes or stigma.
Frequently Asked Questions (FAQ)
1. How much addiction-related content should I expect on Step 1?
There is no fixed percentage, but in most full-length exams and Qbanks you can expect multiple questions per block period involving:
- Drugs of abuse (intoxication/withdrawal, mechanisms)
- SUD-related behavioral science scenarios
- Neurobiology of reward and reinforcement
While addiction medicine isn’t the majority of the test, it’s clearly high-yield relative to its page count in review books.
2. Are there any dedicated “addiction medicine” Step 1 resources I should buy?
You usually don’t need specialty-specific books at this stage. The standard Step 1 resources—First Aid, a high-quality Qbank, and a robust video series—cover everything you need. If you want to go a bit deeper out of interest, consider:
- Short clinical review articles on SUD neurobiology
- Brief guideline summaries on alcohol and opioid use disorders
But keep these as supplements, not the core of your Step 1 plan.
3. How can I quickly distinguish intoxication from withdrawal on exam questions?
Use this rapid framework:
- CNS depressants (alcohol, benzos, barbiturates):
- Intoxication: sedation, ataxia, respiratory depression
- Withdrawal: agitation, tremors, hallucinations, seizures
- Opioids:
- Intoxication: miosis, respiratory depression, constipation
- Withdrawal: mydriasis, lacrimation, diarrhea, piloerection
- Stimulants (cocaine, amphetamines):
- Intoxication: agitation, tachycardia, hypertension, mydriasis
- Withdrawal: depression, fatigue, increased appetite
Practice using mixed Qbank sets and create a single-page comparison chart you review repeatedly.
4. If Step 1 is Pass/Fail, is it still worth putting extra effort into addiction topics?
Yes, for several reasons:
- Addiction questions help you secure a confident pass and build momentum for Step 2 CK.
- The content is clinically central—you will use this knowledge on nearly every rotation.
- If you’re considering an addiction medicine fellowship, early mastery:
- Makes you more effective on clinical teams
- Strengthens your understanding of later advanced concepts
Think of addiction-related Step 1 content as both exam preparation and early specialty training.
By approaching addiction medicine as a core system in your USMLE Step 1 study—rather than an afterthought—you not only improve your chances of passing comfortably, but also lay a solid foundation for a career that may eventually include an addiction medicine fellowship.






















