Why USMLE Step 1 Preparation Matters for Aspiring Ophthalmologists
If you are targeting an ophthalmology residency, your USMLE Step 1 preparation is strategically important—even in the pass/fail era. While Step 1 no longer reports a three‑digit score, program directors in competitive fields like ophthalmology still use it as a filter and as a proxy for your ability to master large volumes of foundational science.
For the ophtho match, Step 1 is often viewed alongside:
- Medical school transcript (pre-clinical performance)
- Step 2 CK score
- Research productivity (especially in ophthalmology)
- Letters of recommendation from ophthalmologists
- Ophthalmology‑specific experiences and performance in away/audition rotations
Strong USMLE Step 1 study habits build the knowledge base you’ll rely on during:
- Ophthalmology shelf exams and rotations
- USMLE Step 2 CK and, later, boards
- Clinical reasoning for neuro‑ophthalmology, retina, glaucoma, and systemic disease with ocular manifestations
This guide will walk you through:
- How Step 1 content intersects with ophthalmology
- A high‑yield, ophthalmology‑oriented Step 1 study strategy
- How to integrate Step 1 resources efficiently
- Concrete examples of eye‑related Step 1 questions and how to think through them
- A timeline and practical tips tailored to future ophthalmologists
Understanding USMLE Step 1 Through an Ophthalmology Lens
The role of Step 1 in the ophtho match
Although Step 1 is now pass/fail, in a highly competitive specialty such as ophthalmology residency, failing Step 1 can be severely detrimental and often requires a compelling remediation story plus outstanding performance in other domains.
Programs may:
- Use a pass on first attempt as a basic screening criterion.
- Look more carefully at your preclinical grades and Step 2 CK score to distinguish candidates.
- Expect robust research and ophthalmology engagement to complement your exam performance.
Result: Treat USMLE Step 1 preparation as a serious, long‑term project, not a “minimum effort to pass” test.
How much ophthalmology is actually on Step 1?
The exam will not test tiny details like rare lens implant types or specific surgical techniques; that’s far beyond its scope. However, ophthalmic content on Step 1 covers:
- Neuroanatomy of the visual pathways
- Optic nerve, chiasm, tract, LGN, optic radiations, visual cortex
- Visual field defects and localizing lesions
- Cranial nerves affecting the eye
- CN II, III, IV, VI and their lesions
- Pupillary reflexes and eye movements
- Autonomic pharmacology of the eye
- Parasympathomimetics, sympathomimetics, and their side effects
- Glaucoma drugs and systemic ocular side effects
- Microbiology and immunology
- Common organisms causing conjunctivitis, keratitis, endophthalmitis
- Viral infections with ocular manifestations (HSV, VZV, CMV)
- Opportunistic infections in immunocompromised patients
- Pathology and systemic disease
- Diabetic and hypertensive retinopathy
- Autoimmune diseases with ocular findings (e.g., Sjögren, sarcoidosis, GPA)
- Nutritional deficiencies (vitamin A deficiency, B12, etc.)
- Embryology and development
- Neural crest derivatives, eye development defects (aniridia, coloboma)
- Pharmacology side effects
- Steroid‑induced cataracts and glaucoma
- Ethambutol optic neuropathy, PDE5 inhibitors and visual changes, isotretinoin and pseudotumor cerebri
You won’t see an “ophthalmology” section on the exam blueprint; eye content is integrated into systems-based questions, particularly neuro, pharm, path, and micro. Thinking in these cross‑disciplinary terms is crucial for high‑yield USMLE Step 1 study.
Building a High‑Yield Step 1 Study Strategy as a Future Ophthalmologist
Step 1 preparation principles that matter for ophtho
Regardless of specialty, effective USMLE Step 1 study is built on:
- Active learning (questions, flashcards, teaching others)
- Spaced repetition (Anki or equivalent)
- Integration (linking basic science to clinical vignettes)
- Continuous assessment and adjustment (NBMEs, self‑assessments)
As an aspiring ophthalmologist, refine these principles with a focus on:
- Neuro‑ophthalmology connections (visual pathways, cranial nerves, neuroanatomy)
- Pharmacology that affects the eye
- Systemic diseases with key ocular manifestations
This alignment helps your Step 1 preparation serve as an early foundation for residency‑relevant knowledge.
Pre‑dedicated vs dedicated: when to emphasize ophthalmology
Pre‑dedicated period (during preclinical years):
- Goal: Build strong basic science, not memorize every rare ocular condition.
- Integrate ophthalmology where it naturally appears in:
- Neuroanatomy (visual fields, cranial nerves)
- Pharmacology (adrenergic and cholinergic drugs, glaucoma meds)
- Microbiology (ocular infections)
- Use USMLE Step 1 resources early, such as:
- First Aid or similar summary books
- Anki (Zanki/Anking or own cards) for visual pathways, CN lesions, and ocular pharm
- Early question bank exposure with organ systems that include eye‑related vignettes
Dedicated study period (typically 4–8 weeks):
- Priority: Passing with margin and building a solid platform for Step 2 and clinical years.
- Ophthalmology angle:
- Aim to master neuroanatomy and neuro‑ophthalmology topics (high test density).
- Solidify pharmacology, especially drug mechanisms and systemic side effects involving the eye.
- Ensure you can cleanly interpret visual field defects and pupillary/ocular motor findings in the context of neurologic and endocrine disease.
Integrating Step 1 resources thoughtfully
There is no single best resource; it’s about combination and execution. High‑yield Step 1 resources used by successful ophtho applicants often include:
1. Core content primers
First Aid for the USMLE Step 1 (or a comparable concise reference)
- Quick, high‑yield review of:
- Visual pathways and lesions (with diagrams)
- Glaucoma drugs and other eye‑related pharmacology
- Selected ocular pathology
- Use it as a map, not a textbook—highlight and annotate with insights from question banks.
- Quick, high‑yield review of:
Boards & Beyond, Pathoma, Sketchy
- Boards & Beyond or a similar video resource: strong for neuroanatomy, endocrine, and pharm.
- Pathoma: basic pathology foundations, including vascular disease impacting retina.
- Sketchy: micro and pharm images help you recall organisms and drugs with ocular impact.
2. Question banks (the backbone of your plan)
Your USMLE Step 1 study should revolve around doing, reviewing, and learning from questions.
UWorld Step 1 QBank
- Ground zero for high‑quality questions.
- Use in tutor mode initially (early in pre‑dedicated) to learn; switch to timed blocks in dedicated.
- Pay special attention to:
- Questions involving visual field defects, cranial nerve palsies, and myasthenia gravis.
- Systemic disease with eye findings (e.g., sarcoidosis patient with uveitis).
Other Qbanks (e.g., AMBOSS, Kaplan) can supplement, but ensure UWorld is fully completed and carefully reviewed.
3. Anki or spaced‑repetition system
For ophtho‑relevant Step 1 content, spaced repetition is especially helpful for:
- Visual pathways and field defects
- Drug mechanisms and side effects affecting the eye
- Critical micro organisms and associated ocular manifestations
You can:
- Use a popular shared deck (e.g., AnKing) and tag/filter for neuro, pharm, micro and retina/eye content.
- Add custom cards from missed question bank items—this is key.
High‑Yield Ophthalmology Concepts for Step 1
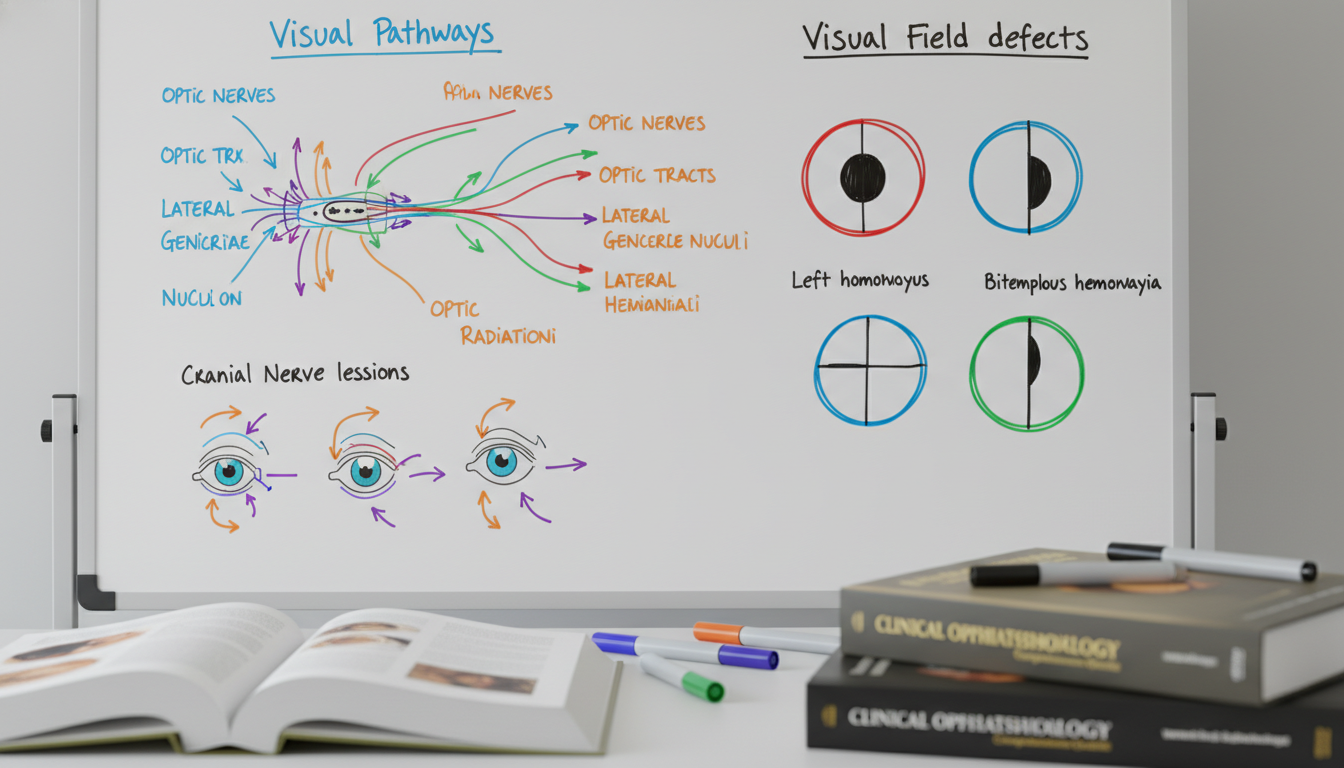
1. Visual pathways and visual field defects
This is arguably the most classic ophthalmology‑relevant Step 1 topic.
Key structures:
- Retina → optic nerve → optic chiasm → optic tract → lateral geniculate nucleus (LGN) → optic radiations → primary visual cortex (occipital lobe)
High-yield patterns:
- Right optic nerve lesion: complete blindness in right eye.
- Optic chiasm lesion (e.g., pituitary adenoma): bitemporal hemianopia.
- Right optic tract lesion: left homonymous hemianopia.
- Meyer's loop (temporal lobe) lesion: contralateral upper quadrantanopia (“pie in the sky”).
- Dorsal optic radiations (parietal lobe) lesion: contralateral lower quadrantanopia.
- PCA infarct affecting occipital lobe: contralateral homonymous hemianopia with macular sparing.
Actionable advice:
- Draw the visual pathway from memory until you can do it in 30–60 seconds.
- Practice translating a clinical vignette’s visual field description into a lesion location.
Example vignette approach:
A 45‑year‑old woman with a history of pituitary adenoma surgery develops progressive difficulty seeing objects on the lateral sides of her visual fields. What is the most likely lesion location?
- Clue: Loss of temporal fields in both eyes → bitemporal hemianopia → optic chiasm.
2. Cranial nerve lesions and ocular motility
Step 1 loves cranial nerve lesions involving eye movement.
Essential patterns:
CN III (oculomotor) palsy
- Eye: down and out
- Ptosis, mydriasis, loss of accommodation
- Common causes: posterior communicating artery aneurysm, uncal herniation, diabetic ischemic neuropathy (often pupil-sparing)
CN IV (trochlear) palsy
- Affected muscle: superior oblique
- Vertical diplopia, worse when going down stairs or reading
- Patient may tilt head away from affected side to compensate.
CN VI (abducens) palsy
- Inability to abduct eye
- Horizontal diplopia, especially when looking toward the affected side
- May be early sign of increased intracranial pressure.
Study tip: For each cranial nerve, know:
- Muscle innervations
- Function
- Presentation of lesion
- Classic causes (e.g., microvascular ischemia vs compressive lesion)
3. Pupillary reflexes and autonomic control
Afferent (sensory): CN II
Efferent (motor): CN III (parasympathetic) → constrictor pupillae
Classic Step 1 scenarios:
- Marcus Gunn pupil (relative afferent pupillary defect, RAPD)
- Defect in afferent limb (CN II or retina)
- Swinging flashlight test: both pupils constrict when light shone in the normal eye; both dilate when light shone in affected eye.
- Horner syndrome
- Triad: ptosis, miosis, anhidrosis
- Lesion of the sympathetic pathway: e.g., Pancoast tumor, carotid dissection, brainstem lesions.
Step 1 preparation tip: Pair these physiologic pathways with clinical examples in your Anki deck; link signs (ptosis, anisocoria) to lesion sites.
4. Glaucoma drugs and other eye-related pharmacology
Pharmacology is central to USMLE Step 1 study; eye‑related drugs are high yield.
Glaucoma drug categories (very testable):
- Prostaglandin analogues (e.g., latanoprost)
- ↑ outflow of aqueous humor via uveoscleral pathway
- Side effect: darkening of iris, eyelash growth
- β‑blockers (e.g., timolol)
- ↓ aqueous humor production
- Side effects: systemic β‑blockade (bronchospasm, bradycardia)
- α2‑agonists (e.g., brimonidine)
- ↓ aqueous production and ↑ outflow
- Carbonic anhydrase inhibitors (e.g., acetazolamide)
- ↓ aqueous humor production
- Side effects: metabolic acidosis, kidney stones
- Cholinomimetics (e.g., pilocarpine)
- ↑ outflow by contracting ciliary muscle and opening trabecular meshwork
- Side effects: miosis, decreased night vision, brow ache
Other drug‑related eye findings frequently tested:
- Steroids → cataracts, glaucoma.
- Ethambutol → optic neuropathy (red‑green color blindness, central scotoma).
- Amiodarone → corneal microdeposits, optic neuropathy.
- PDE5 inhibitors (sildenafil) → blue‑tinged vision, ischemic optic neuropathy (rare).
- Isotretinoin → pseudotumor cerebri, nyctalopia.
When you review pharm questions, explicitly note any ocular side effects and create flashcards.
5. Microbiology and immunology with ocular manifestations
You don’t need fellowship‑level detail, but Step 1 expects you to connect pathogens and immune processes to ocular findings.
Organisms and conditions often examined:
- Neisseria gonorrhoeae & Chlamydia trachomatis
- Neonatal conjunctivitis; difference in timing and exudate.
- Adenovirus
- Epidemic keratoconjunctivitis: red eye, often after swimming pools or outbreaks.
- HSV/VZV
- Dendritic keratitis, uveitis, acute retinal necrosis.
- CMV retinitis
- HIV/AIDS, low CD4; “pizza pie” retina on exam.
- Toxoplasma gondii
- Chorioretinitis, especially congenital.
Immunologic diseases:
- Sarcoidosis → uveitis, lacrimal gland involvement.
- Sjögren syndrome → keratoconjunctivitis sicca (dry eyes).
- Granulomatosis with polyangiitis (GPA) → scleritis, orbital inflammation.
Always link ocular signs back to systemic disease and immune pathophysiology. This aligns perfectly with USMLE Step 1’s integrative style.
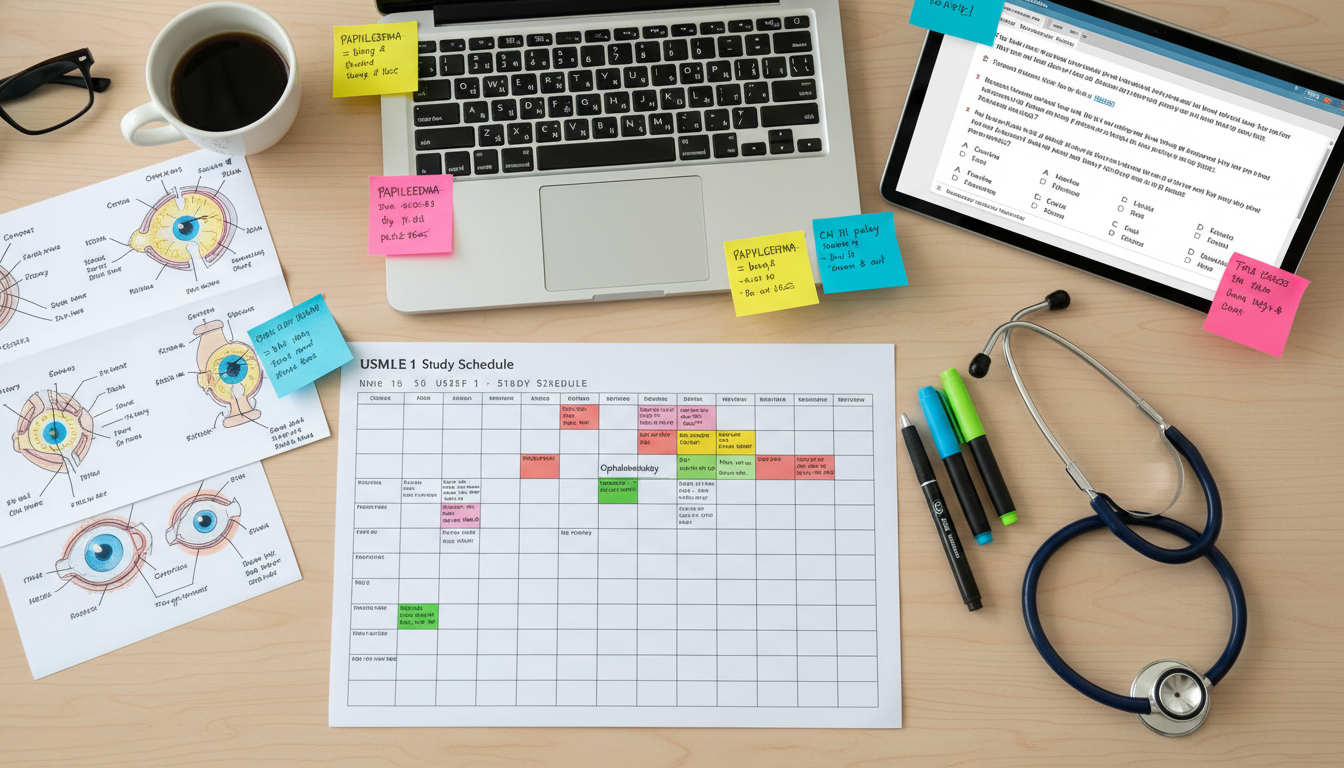
A Practical Step 1 Study Timeline for Future Ophthalmologists
Phase 1: Early preclinical (6–18 months before exam)
Objectives:
- Build a solid foundation in basic sciences.
- Start USMLE Step 1 resources lightly and consistently.
Action steps:
- During neuro and head/neck blocks:
- Focus deeply on visual pathways, cranial nerves III/IV/VI, and brainstem anatomy.
- Draw neuro‑ophthalmic tracts frequently.
- During pharm and micro blocks:
- Tag any eye‑related drugs or microbes in your notes/Anki.
- As you learn new medications, think: “Does this drug have important ocular side effects?”
- Start modest use of a Step 1 Qbank (e.g., 10–20 questions/day) tied to your current coursework.
Phase 2: Intensified preparation during late preclinical (3–6 months before dedicated)
Objectives:
- Transition from course‑based studying to exam‑based thinking.
- Identify and fix weak areas relevant to neuro‑ophthalmology and pharm.
Action steps:
- Increase Qbank volume to 20–40 questions/day, mixed blocks.
- Begin structured USMLE Step 1 study plan using:
- First Aid (or equivalent) + Pathoma/Boards & Beyond.
- Active annotation of neuro and pharm sections.
- Take a baseline NBME to understand where you stand.
- Meet or email a mentor in ophthalmology to:
- Get guidance on balancing Step 1 study with early ophthalmology exposure.
- Discuss research possibilities that can continue during dedicated.
Phase 3: Dedicated study (4–8 weeks)
Objectives:
- Pass Step 1 with margin.
- Solidify understanding of high‑yield systems, especially neuro, pharm, path, and micro.
Daily structure (example for 6‑week dedicated):
- Morning: 2 UWorld blocks (40 questions each), timed, mixed.
- Midday: Review explanations, annotate First Aid/notes, create/adjust Anki cards.
- Afternoon: Focused content review (e.g., neuroanatomy for 2 days, pharm for 2 days).
- Evening: 200–400 targeted Anki cards; short review of weak topics.
Ophthalmology‑relevant checklist:
- You can:
- Draw visual pathways and field defects from memory.
- Localize cranial nerve lesions based on eye position and diplopia description.
- Explain pupillary light reflex and identify RAPD patterns.
- List major glaucoma drug classes and mechanisms without notes.
- Recognize key ocular manifestations of systemic disease (diabetes, hypertension, autoimmune conditions, HIV).
Phase 4: Post‑Step 1: Leveraging knowledge for ophthalmology residency
Even after Step 1:
- Continue to use your neuro‑ophthalmology base for Step 2 CK preparation and clinical neurology/internal medicine rotations.
- During ophthalmology electives:
- Connect the pathology seen on slit lamp or fundoscopy to your Step 1 pathophysiology.
- Ask residents to “teach up” the systemic disease link: e.g., “How does poorly controlled diabetes cause this specific retinal finding?”
This continuity strengthens your application narrative: a consistent, stepwise path from basic science mastery to clinical ophthalmology.
Common Mistakes and How to Avoid Them
Mistake 1: Ignoring general content to over‑focus on niche ophthalmology details
Some future ophthalmologists get drawn to subspecialty‑level material (e.g., OCT patterns, surgical pearls) that are not Step 1‑relevant. For USMLE Step 1 preparation, your priority is broad, high‑yield basic science.
Fix:
Limit subspecialty ophtho learning during dedicated to:
- Brief, enjoyable reading or podcasts as breaks.
- Clinical shadowing if it doesn’t compromise core Step 1 study.
Mistake 2: Memorizing diagrams without clinical context
Students sometimes memorize visual pathway diagrams but struggle to apply them to vignettes describing visual complaints.
Fix:
- Practice with cases:
- “A patient with a stroke now has right homonymous hemianopia; where is the lesion?”
- “Vertical diplopia worsening when reading – which CN is affected?”
- Use UWorld’s explanations and NBME questions to reinforce lesion localization.
Mistake 3: Under‑utilizing pharmacology and micro
Both disciplines are high‑yield for Step 1 and heavily integrated with ophthalmology (glaucoma drugs, infectious eye disease).
Fix:
- Make pharmacology central in your USMLE Step 1 study routine.
- Create or review Anki cards that tie:
- Drug → Mechanism → Systemic effect → Ocular effect (if important).
- Pathogen → Virulence factors → Systemic manifestations → Eye manifestations.
Mistake 4: Neglecting mental and physical health
Competitive specialties like ophthalmology can tempt students into unsustainable Step 1 preparation schedules.
Fix:
- Build in:
- Regular sleep schedules (7–9 hours).
- Short, daily exercise sessions.
- One lighter study half‑day per week for recovery.
- Seek support early if feeling burnt out; sustained performance matters more than a perfect short burst.
FAQs: USMLE Step 1 Preparation for Future Ophthalmologists
1. Does pass/fail Step 1 still matter for ophthalmology residency?
Yes. While programs no longer see a numeric score, a first‑time pass remains essential, especially in a competitive field like ophthalmology residency. Programs will likely shift more emphasis to Step 2 CK, clinical grades, research, and letters—but a failure on Step 1 can significantly weaken your application. Strong USMLE Step 1 study habits also set you up for a better Step 2 CK performance.
2. How much time should I dedicate to ophthalmology‑specific content versus general Step 1 material?
During dedicated, over 90–95% of your time should be on general high‑yield Step 1 content (neuro, pharm, path, micro, etc.). The “ophthalmology” portion is mostly embedded within these core disciplines—visual pathways, cranial nerves, glaucoma pharmacology, and systemic disease with eye findings. True subspecialty ophtho reading is optional and should not displace core exam prep.
3. Which Step 1 resources are best if I know I want ophthalmology?
Use the same high‑yield Step 1 resources as other top performers:
- A primary reference (First Aid or similar)
- A high‑quality question bank (UWorld as the cornerstone)
- Video resources for tough topics (e.g., Boards & Beyond, Pathoma, Sketchy)
- Anki or another spaced‑repetition system
The “ophtho‑specific” twist comes from how you use them: pay particular attention to neuro‑ophthalmology, pharm with ocular effects, and systemic disease with prominent eye findings.
4. How can I balance Step 1 preparation with early ophthalmology research and shadowing?
During heavy preclinical periods and especially dedicated Step 1 study, prioritize coursework and USMLE Step 1 preparation. You can:
- Engage in low‑intensity, longitudinal research that doesn’t require daily benchwork (e.g., chart reviews, retrospective projects).
- Shadow ophthalmologists on occasional half‑days or weekends, not at the cost of your core studying.
- Ramp up research intensity and ophtho exposure after Step 1, when you can build on your strong basic science foundation with more clinical ophthalmology experiences.
By aligning your USMLE Step 1 preparation with the knowledge base you’ll need as an ophthalmology resident, you turn an exam requirement into a strategic advantage in the ophtho match.






















