Understanding the Role of USMLE Step 1 in a Radiation Oncology Career
USMLE Step 1 has transitioned to pass/fail, but it still matters—especially if you are interested in a competitive field like radiation oncology. While a 3-digit score no longer appears on your transcript, your performance indirectly influences how strong your application looks overall and how solid your knowledge base will be when you reach clinical radiation oncology rotations and, later, residency.
Radiation oncology is a specialty that sits at the intersection of radiobiology, physics, oncology, and clinical medicine. Many of the intellectual foundations of rad onc—DNA damage and repair, cell cycle checkpoints, tumor biology, immunology, pharmacology of chemotherapeutics, and basic imaging—are heavily tested on Step 1. Thoughtful USMLE Step 1 preparation will:
- Build a strong foundation in cancer biology and treatment principles that you will revisit throughout your rad onc career
- Make your preclinical and early clinical oncology experiences easier and more productive
- Free up time and cognitive bandwidth later to focus on research, away rotations, and rad onc–specific learning, because you are not struggling with core basic science concepts
- Signal to radiation oncology faculty (during MS3/MS4 rotations) that you understand the science behind their field and can talk intelligently about mechanisms
Even though residency program directors in radiation oncology can no longer see a Step 1 score, many still ask about your preparation strategy, use preclinical performance as a proxy, and—importantly—expect you to demonstrate Step 1–level understanding of relevant science when you interact with them on rotations or interviews.
This guide will help you design a USMLE Step 1 study plan that simultaneously maximizes your chances of passing the exam and strategically aligns with your long‑term goal of matching into a radiation oncology residency.
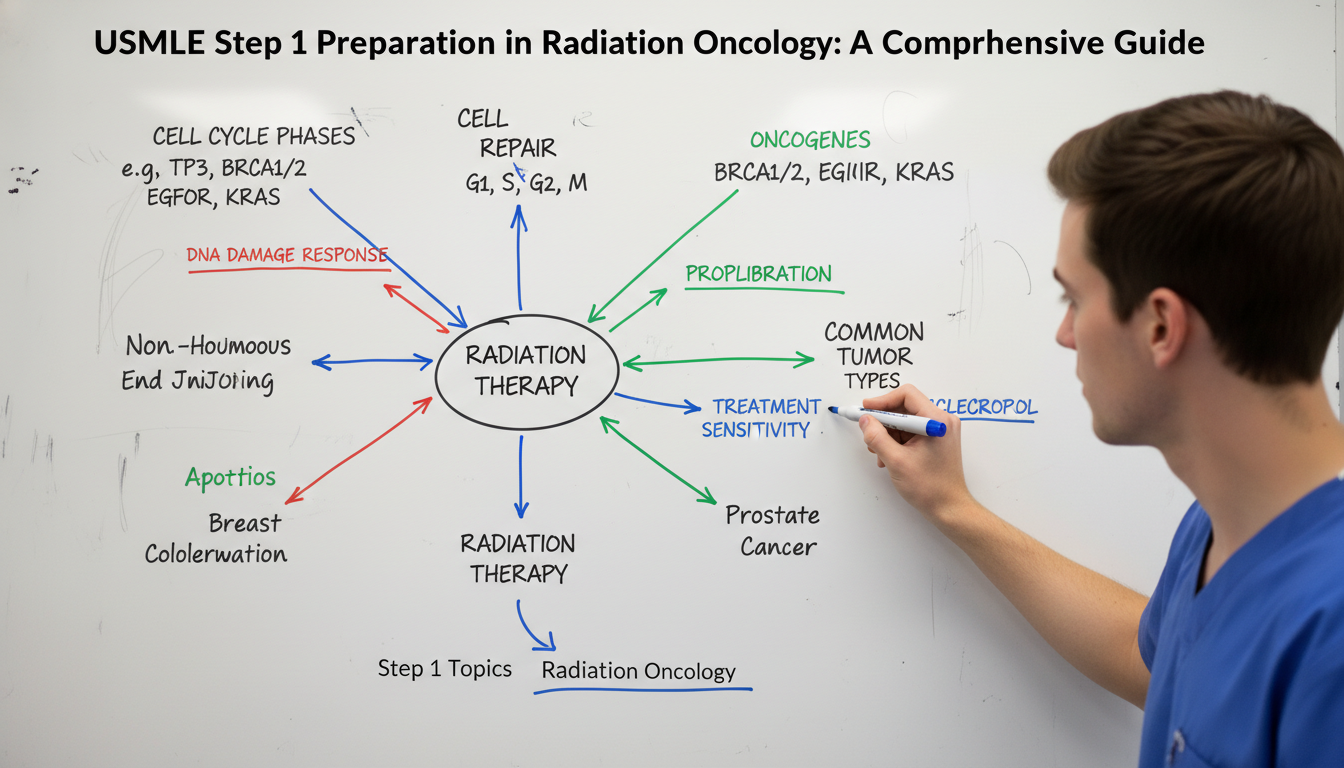
Core Principles of Step 1 Preparation with a Radiation Oncology Mindset
Step 1 is not an “oncology exam,” but many of its high‑yield domains map closely onto the foundation of a career in radiation oncology. Think of your USMLE Step 1 study as your first real pass through the language and framework you’ll need as a radiation oncologist.
1. Adopt a Systems and Mechanisms Mindset
Radiation oncology revolves around understanding how treatments affect tissues and tumors at the molecular, cellular, and organ levels. Build this mindset into your Step 1 preparation by focusing less on memorizing isolated facts and more on mechanisms:
- For pharmacology, ask: How does this drug affect DNA replication, cell division, or apoptosis? Is it radiosensitizing or radioprotective?
- For pathology, ask: How does this tumor’s mutation profile affect proliferation, survival signaling, and treatment response?
- For physiology, ask: How do organs respond to injury and radiation-induced inflammation? How does vascular, pulmonary, and GI physiology change after damage?
This approach not only helps retention but also creates a natural bridge between your USMLE knowledge and later radiation oncology training.
2. Focus on High-Yield Cancer-Adjacent Topics
You must still cover the entire USMLE blueprint, but several content areas are particularly relevant for future radiation oncologists and worth emphasizing:
- Cell cycle and apoptosis (cyclins, CDKs, p53, Rb, Bcl-2, caspases)
- DNA damage and repair pathways (NHEJ, homologous recombination, mismatch repair, nucleotide excision repair, base excision repair)
- Oncogenes and tumor suppressors (e.g., KRAS, BRAF, MYC, TP53, BRCA1/2, APC, PTEN, NF1)
- Signal transduction in cancer (RTKs, MAPK, PI3K/AKT/mTOR, Wnt, Hedgehog)
- Immunology (T-cell activation, checkpoints like CTLA-4/PD-1, tumor immune evasion)
- Radiation-sensitive tissues and organ tolerance concepts (even at a simplistic preclinical level)
- General oncologic pathology (solid tumors and hematologic malignancies)
- Pharmacology of chemotherapeutics (platinum agents, antimetabolites, alkylating agents, topoisomerase inhibitors, taxanes, and targeted/biologic agents)
For each of these, don’t just memorize what Step 1 might test. Instead, ask, “How would this matter for a patient receiving radiation therapy?” That clinical anchor improves long-term retention.
3. Use Active Learning Tools That Mirror Oncology Thinking
The same tools that help everyone prepare for Step 1—anki, spaced repetition, question banks—can be calibrated in ways useful for your future rad onc practice:
- Create conceptual Anki cards that link, for example, “BRCA mutation → faulty homologous recombination → sensitivity to DNA-damaging therapies (e.g., platinum, PARP inhibitors, potentially radiation).”
- When reviewing question bank explanations, add a second reflection: “If this patient later needed radiation, what special considerations might exist?” For example, baseline pulmonary disease before thoracic radiation.
- Maintain a “cancer and radiation” notebook or digital document where you collect Step 1 topics that feel especially relevant: gene mutations, radiosensitivity syndromes, endocrine cancers, and molecular target pathways.
By USMLE test day, you’ll have a curated mini–radiation oncology primer built out of Step 1 content.
Designing a USMLE Step 1 Study Plan that Supports a Future in Rad Onc
A well-structured study schedule is crucial for Step 1 preparation. For those considering a radiation oncology residency, you want a plan that balances efficiency with deeper learning in oncology-related areas.
1. Map Out Your Timeline
Your timeline will depend on your school’s curriculum and when you’re allowed to take Step 1, but a common structure is:
Foundation Phase (Ongoing during preclinical years)
- Goal: Integrate Step 1 resources with your courses
- Focus on building conceptual understanding of physiology, biochemistry, and pathology
- Begin light exposure to oncology-related mechanisms
Dedicated Study Period (4–10 weeks)
- Goal: Consolidate and review, heavy use of question banks and practice exams
- Refine weak areas, including cancer‑adjacent topics and integrated systems
- Incorporate targeted revisits of key tumor biology and pharmacology
Post-Step 1 “Consolidation” Phase
- Even after passing, revisit high-yield oncology-related content ahead of clinical rotations. This will support your radiation oncology rotations, research, and interviews.
2. Blend Course Learning and USMLE Step 1 Resources
Many students struggle to reconcile preclinical lectures with USMLE Step 1 study materials. The key is integration:
- For each block (e.g., hematology/oncology, GI, neuro), align:
- Your lectures/slides
- A primary review text (e.g., First Aid, Boards & Beyond, or similar)
- A question bank (UWorld, AMBOSS)
- Before or after each lecture, quickly skim the relevant section of your Step prep resource so everything is anchored in a USMLE framework.
- When your curriculum covers cancer or radiobiology-relevant topics (e.g., DNA repair, immunology), give those sections extra attention and link them explicitly to your interest in radiation oncology.
This integrated approach ensures your USMLE Step 1 study time pays dividends both for the exam and for your future rad onc trajectory.
3. Use Question Banks Strategically for Cancer-Related Content
Your rad onc match prospects don’t depend on answering all the cancer questions correctly on Step 1—but those questions highlight areas you’ll revisit repeatedly in your career.
As you work through a USMLE question bank:
- Tag or flag oncology-related questions (heme/onc, immunology, pathology, pharm) to review again later.
- When you encounter a tumor type (e.g., small cell lung cancer, glioblastoma, squamous cell carcinoma of the head and neck):
- Note key mutations, pathways, and paraneoplastic syndromes.
- Briefly reflect on how that tumor is commonly treated, including whether radiation plays a major or minor role.
- Make a “top 20 tumors to remember” list that you revisit near the end of your dedicated period.
This targeted approach gives you a small but meaningful early exposure to the epidemiology and biology of cancers you’ll see frequently in radiation oncology residency.
4. Manage Time and Burnout: Think Like a Future Specialist
Radiation oncology requires sustained attention and precision. Build these habits now:
- Use time‑blocked schedules: 60–90 minutes focused study, 10–15 minutes rest.
- Protect non‑negotiable daily recovery (sleep, brief exercise, meals without screens). Cognitive performance for USMLE Step 1 study—and later for rad onc boards—depends heavily on sleep and physical health.
- Accept that you do not need to master every esoteric detail. Emphasize patterns and mechanisms; let rare trivia go. This is particularly important as Step 1 is now pass/fail.
By learning to preserve your bandwidth and focus, you’re practicing the same skills that will support you during residency, where precision and cognitive stamina are critical.
High-Yield Step 1 Domains for Aspiring Radiation Oncologists
Radiation oncology is deeply rooted in basic science that you study for Step 1. The following domains are particularly important for your future specialty and warrant focused, conceptual understanding.
1. Molecular Biology, DNA Repair, and Cell Cycle
Radiation therapy primarily works by inducing DNA damage, especially double-strand breaks. Step 1 repeatedly examines the molecules involved in maintaining genomic integrity:
DNA repair pathways
- Nucleotide excision repair: defects → xeroderma pigmentosum (UV sensitivity)
- Base excision repair: important for single-base lesions
- Mismatch repair: defects → Lynch syndrome (colorectal and other cancers)
- Nonhomologous end joining: error-prone pathway; defects → ataxia-telangiectasia, SCID variants
- Homologous recombination: high-fidelity; defects in BRCA1/2 and Fanconi anemia
Cell cycle checkpoints
- G1–S checkpoint: governed heavily by p53 and Rb
- G2–M: important for many chemotherapeutic agents and radiosensitivity
- Cyclins and CDKs: dysregulation leads to uncontrolled proliferation
Understanding these pathways is central to both Step 1 and rad onc: many hereditary cancer syndromes, radiosensitivity syndromes, and targeted therapies revolve around these mechanisms.
2. Tumor Biology and Oncogenes/Tumor Suppressors
For the rad onc match, you’ll eventually need to discuss tumors at a molecular level during interviews and on rotations. Use your USMLE Step 1 study to internalize:
- Oncogenes (gain-of-function): e.g., BCR-ABL, MYC, KRAS, HER2/neu
- Tumor suppressors (loss-of-function): e.g., TP53, RB, APC, PTEN, VHL
- Hallmarks of cancer: sustained proliferation, evasion of apoptosis, angiogenesis, immune evasion
When studying specific tumors on Step 1 (e.g., colon cancer with APC loss, CML with BCR-ABL, melanoma with BRAF mutation), mentally connect:
Mutation → protein/function change → altered pathway → phenotype → therapeutic target
This pattern thinking will be invaluable later when you’re considering combinations of radiation and targeted or immunotherapies.
3. Immunology and Cancer Immunotherapy Foundations
Modern radiation oncology increasingly overlaps with immunotherapy. Step 1 immunology can feel abstract, but for a future radiation oncologist, it’s crucial.
Prioritize:
- T-cell activation (signal 1 and 2), costimulatory molecules (CD28/B7)
- Major histocompatibility complex (MHC I and II) and antigen presentation
- Key cytokines (IL-2, IFN-γ, TNF-α) and their effects
- Immune checkpoints: CTLA-4, PD-1/PD-L1 pathway (even if Step 1 only lightly touches these, know the basics independently)
- Mechanisms of tumor immune evasion (downregulating MHC I, secreting immunosuppressive cytokines)
Radiation can modulate the tumor microenvironment and immune response (e.g., abscopal effect), concepts that will be much easier to understand if you’ve built a strong immunology foundation now.
4. Organ System Pathology: Where Radiation Matters
As you work through organ system pathology for Step 1, note which tumors are commonly treated with radiation and which are not. You don’t need residency-level detail, but a rough mental map helps.
Examples:
- Head & Neck: squamous cell carcinomas, nasopharyngeal carcinoma—radiation plays a major role
- Central Nervous System: glioblastoma, meningioma, brain metastases—radiation (including stereotactic radiosurgery) is central
- Breast: adjuvant radiation after lumpectomy; particular importance in DCIS, early-stage invasive cancers
- Prostate: definitive radiation is a mainstay alternative to surgery
- Lung: small cell (chemo + radiation), limited-stage NSCLC (surgery ± radiation), stereotactic body radiotherapy for early-stage or inoperable disease
- Hematologic malignancies: historically extensive radiation; now more focused but remains critical in some lymphomas and CNS prophylaxis strategies
As you study Step 1 pathology, develop a brief one-line association: “Is radiation important in this disease?” and “What organ toxicities would I worry about if irradiated?”
5. Pharmacology: Cytotoxic and Targeted Oncologic Drugs
USMLE Step 1 pharmacology is notoriously dense. For a future radiation oncologist, focus especially on:
- DNA-damaging agents: cisplatin, carboplatin, cyclophosphamide, ifosfamide, bleomycin
- Antimetabolites: methotrexate, 5-FU, cytarabine, gemcitabine
- Topoisomerase inhibitors: doxorubicin, etoposide, irinotecan
- Microtubule agents: paclitaxel, vincristine, vinblastine
- Hormonal agents: tamoxifen, aromatase inhibitors, antiandrogens (commonly used with radiation for breast and prostate cancers)
- Targeted and biologic therapies: imatinib, trastuzumab, EGFR inhibitors, BRAF inhibitors, and checkpoint inhibitors
You don’t need fellowship-level detail now, but aligning your Step 1 pharmacology with a framework of “how these combine with radiation later” will make both the exam and future learning more coherent.
Step 1 Resources and Study Strategies Tailored for Future Rad Onc Residents
Nearly everyone uses similar core Step 1 resources, but how you use them can be adjusted to support your radiation oncology residency goals.
1. Foundational Content Resources
Common choices include:
- Boards & Beyond / Pathoma / similar video series
- A standard “big book” (e.g., First Aid or an equivalent integrated resource)
- Your school’s notes and review materials
Tips for rad onc–minded use:
- During biochemistry and molecular biology units, slow down for DNA replication, repair, and cell cycle content. Tag these for later dedicated review.
- During pathology units, build your “oncology core” list—tumors, mutations, and patterns worth remembering.
- In immunology, add a small side project: summarize how T cells and antigen presentation relate to tumor recognition.
2. Question Banks: A Dual Purpose
UWorld, AMBOSS, and similar banks are central to USMLE Step 1 study:
- Do questions timed and in mixed mode once you’re comfortable; this mirrors real exam conditions.
- After each oncology-related question, spend 30–60 seconds reflecting beyond the explanation: “Would radiation be involved? What baseline organ risks does this patient have (lung, heart, kidney, spinal cord)?”
- Mark especially good oncology questions so you can quickly review them in the last 1–2 weeks of your dedicated period.
This not only improves test performance but naturally introduces rad onc clinical reasoning into everyday Step 1 study.
3. Anki and Spaced Repetition: Build an Oncology Spine
If you use Anki:
- Integrate Step 1 decks that cover foundational science comprehensively.
- Add custom oncology and radiobiology cards:
- DNA repair defects → disease → cancer risk → therapy implications
- Oncogene/tumor suppressor → common associated tumor → one clinical feature
- Organ-specific radiation concerns (high-level): e.g., “Lung: risk of pneumonitis and fibrosis; Heart: coronary artery disease, cardiomyopathy; Spine: myelopathy risk.”
Revisiting these cards throughout preclinical years ensures that when you finally rotate in radiation oncology, the language and concepts will already feel familiar.
4. Practice Exams and Self-Assessment
Even though Step 1 is pass/fail, practice tests (NBME forms, UWorld self-assessments) are essential:
- Schedule at least 2–3 self-assessments during your dedicated period.
- Use your results to identify both general weaknesses and specific cancer-related gaps. For example, if you repeatedly miss questions on lymphomas or brain tumors, target those topics.
- Avoid obsessing over predicted 3-digit scores; instead, ask: “Is my knowledge stable enough that I can focus on more advanced learning later, including for my radiation oncology goals?”
Connecting Step 1 Preparation to the Rad Onc Match and Beyond
Your USMLE Step 1 performance is now pass/fail, but your preparation has ripple effects across your entire radiation oncology residency application.
1. How Step 1 Preparation Supports Your Rad Onc Match
Program directors in radiation oncology increasingly emphasize:
- Strong clinical evaluations and letters of recommendation
- Research productivity, especially in oncology or related fields
- USMLE Step 2 CK performance, now more heavily weighted
- Demonstrated interest in and understanding of oncology
Deep, thoughtful USMLE Step 1 study:
- Makes your Step 2 CK preparation easier, because the same mechanistic framework applies to clinical oncology scenarios.
- Speeds up your ability to contribute meaningfully to radiation oncology research, since you won’t struggle with basic pathways or tumor biology.
- Helps you stand out on rad onc electives by asking higher-level questions that integrate molecular biology, immunology, and treatment planning concepts.
2. Leveraging Oncology Interest During Preclinical Years
You can align your Step 1 preparation with broader actions that strengthen your radiation oncology residency application:
- Join your school’s oncology interest group; apply your growing knowledge to journal clubs.
- Seek out radiation oncology mentors early. Demonstrating that your Step 1 preparation ties into an authentic interest in their specialty is compelling.
- If you do early research, your understanding of DNA repair, immunology, or tumor biology—built during USMLE Step 1 study—makes you more efficient and valuable in the lab or retrospective clinical projects.
3. Perspective: Don’t Over-Optimize the “Rad Onc Angle”
It is important not to distort your study priorities: USMLE Step 1 is still a broad, basic science exam, and your primary goal is to pass comfortably while building a robust general medical foundation. Being “rad onc‑aware” in your preparation should refine, not dominate, your strategy.
- Cover all systems comprehensively, not just oncology-heavy ones.
- Use your interest in radiation oncology as a motivational tool—a way to make abstract mechanisms more meaningful—not as an excuse to neglect non-oncologic content.
- Remember that residency programs value well-rounded physicians who can handle all aspects of patient care, not just their eventual subspecialty.
FAQs: USMLE Step 1 Preparation for Future Radiation Oncologists
1. Does a pass/fail Step 1 still matter for a radiation oncology residency?
Yes, though indirectly. Programs no longer see a numerical Step 1 score, but they still care that you:
- Passed comfortably (no failures or late attempts)
- Built a strong basic science foundation that supports good Step 2 CK scores and clinical performance
- Can discuss cancer biology, immunology, and treatment principles intelligently on rotations and in interviews
Strong USMLE Step 1 preparation sets the stage for all of those outcomes.
2. Should I use different Step 1 resources because I’m interested in radiation oncology?
You do not need entirely different Step 1 resources. The same core materials (question banks, comprehensive review books, videos) are appropriate. What changes is how you use them:
- Pay extra attention to DNA repair, cell cycle, oncology pathology, and immune mechanisms.
- Connect pharmacology of chemotherapeutics and targeted agents to potential use with radiation.
- Keep a running list of oncology-related concepts you want to revisit later.
This approach supports both the exam and your future rad onc training.
3. How much should I focus on cancer topics compared with everything else on Step 1?
Cancer-related content is important but remains a subset of the exam. You should:
- Study all Step 1 domains thoroughly; there is no “oncology-only” path to passing.
- Use your interest in radiation oncology to make certain topics (DNA repair, immunology, cell biology) particularly strong.
- Aim for balance: perhaps give an extra review pass to oncology-related topics during dedicated, but never at the expense of major weaker systems like cardio, renal, or neuro.
4. Can I talk about my Step 1 preparation in radiation oncology interviews?
Yes, and it can be powerful if framed correctly. Instead of saying, “I studied extra hard for Step 1,” focus on:
- How Step 1 preparation deepened your understanding of tumor biology, immunology, and DNA repair
- How that foundation helped you in rad onc research or clinical rotations
- How you now view radiation therapy through the lens of the basic science you learned
Interviewers appreciate candidates who connect preclinical learning to clinical practice in a thoughtful way.
Thoughtful, structured USMLE Step 1 preparation does far more than check a licensing box. It builds the scientific backbone of your future career in radiation oncology. By aligning your Step 1 study with an understanding of cancer biology, DNA damage and repair, immunology, and therapeutics, you not only prepare to pass the exam—you also lay the groundwork to thrive in a radiation oncology residency and beyond.






















