USMLE Step 3 can feel like a distant afterthought when you’re busy crafting the perfect derm application, but your approach to Step 3 has real implications for your dermatology residency journey. It affects visa status (for some), state licensure timelines, and—importantly—the time and bandwidth you’ll have to invest once you’re actually in a dermatology residency.
This guide focuses on how to approach USMLE Step 3 preparation in the context of a dermatology career—whether you’re an MS4 planning ahead, a derm-prelim or transitional year intern, or an early dermatology resident trying to finish the exam efficiently and strategically.
Understanding USMLE Step 3 in the Dermatology Context
USMLE Step 3 is the final examination in the USMLE sequence. While it is not a primary screening tool for dermatology residency programs (unlike Step 1 and Step 2 CK), it still matters for several reasons that directly affect your derm career and match strategy.
What Step 3 Covers
Step 3 tests whether you can apply foundational medical knowledge and clinical reasoning to unsupervised practice, with emphasis on:
- Diagnosis and management in ambulatory and inpatient settings
- Emergency and critical care decisions
- Preventive medicine and population health
- Interpretation of labs, imaging, and consult notes
- Safe prescribing and management of common medications
- Longitudinal care and follow-up decisions
Although dermatology is not heavily represented, skin-related topics appear through:
- Dermatologic manifestations of systemic disease (e.g., lupus, dermatomyositis, vasculitis)
- Common outpatient rash and lesion complaints
- Infections with cutaneous findings (e.g., cellulitis, erysipelas, varicella, measles)
- Drug eruptions and hypersensitivity reactions
- Skin emergencies (SJS/TEN, necrotizing fasciitis, meningococcemia)
Why Step 3 Matters for Dermatology Residency and Derm Match
For many dermatology applicants and residents, Step 3 feels like an extra hurdle with unclear payoff. Here’s where it concretely intersects with dermatology:
Licensure and moonlighting
- Many states require Step 3 for full medical licensure, which can affect your ability to moonlight during derm residency or practice after graduation.
- Programs in certain states strongly encourage or require residents to complete Step 3 by the end of PGY-1.
Visa considerations (IMGs)
- If you’re on a H-1B visa, many institutions require a passed Step 3 before they can sponsor you.
- This can influence your derm match strategy: taking Step 3 early may expand the programs you can apply to.
Application signaling for reapplicants or at-risk profiles
- If you previously had a marginal Step 1 or Step 2 CK score, a strong Step 3 performance can help signal improvement in clinical reasoning and test-taking.
- For reapplicants to dermatology, having Step 3 completed shows readiness and commitment to clinical excellence.
Protecting your bandwidth during dermatology residency
- Dermatology training is dense—learning medical derm, procedural skills, pathology, cosmetics, research, and clinic efficiency.
- Taking Step 3 at a high-stress time of derm residency can detract from your performance and career-building activities (research, networking, conferences).
- Strategically planning Step 3 during residency—or before—is therefore a key part of long-term success.
When to Take Step 3 if You’re Pursuing Dermatology
Choosing the right timing is one of the most important decisions you’ll make regarding Step 3.
Common Timing Options
- Late MS4 / Immediately after graduation
- During internship (prelim medicine, transitional year, or TY with derm)
- Early in dermatology residency (PGY-2 / PGY-3)
Each path has pros and cons.
Option 1: Late MS4 / Immediately After Graduation
Pros:
- Step 2 CK knowledge is still fresh—shorter dedicated prep time.
- You often have more control of your schedule (electives, lighter months).
- You enter internship and dermatology residency with USMLE obligations fully completed.
- No need to juggle Step 3 with intern-year call, notes, and fatigue.
Cons:
- You may be busy with ERAS, interviews, sub-internships, and away rotations.
- Some schools and states restrict when you can register for Step 3 (you may need your diploma and/or certain credentials first).
- If you’re still actively optimizing for derm match, you may feel stretched between Step 3 prep and derm-related activities.
Best for:
- US grads with predictable graduation timelines.
- Applicants with strong Step 1/Step 2 CK who can afford a slightly shorter prep.
- Those who strongly want all exams done before starting internship.
Option 2: During Internship (Prelim/TY Year)
This is the most common option for dermatology-bound trainees.
Pros:
- Clinical experience from internship helps with management and CCS-style reasoning.
- You can choose a lighter rotation (e.g., outpatient, elective, consults) for your exam window.
- Taking Step 3 early in intern year often aligns well with H-1B visa requirements.
Cons:
- Internship is tiring; studying after long days or call is challenging.
- Scheduling can be tricky—many states require a few months of GME before you’re eligible to sit for Step 3.
- Poor planning can lead to last-minute cramming before a strict program deadline.
Best for:
- Most dermatology applicants and matched residents, especially those in medicine prelim or TY with enough outpatient exposure.
- IMGs who need Step 3 completed for visa reasons and want it done before derm residency.
Option 3: Early in Dermatology Residency
Some residents defer Step 3 until PGY-2 (first derm year) or even PGY-3.
Pros:
- Stronger real-world clinical insight, especially for outpatient med-derm cases.
- More maturity in clinical reasoning and comfort with guidelines.
Cons:
- Dermatology residency is fast-paced and content-heavy; Step 3 becomes an additional burden.
- Less time for research, QI projects, and building your derm portfolio.
- You may be limited by licensure timelines or institutional expectations.
Best for:
- Those who absolutely could not take it earlier (visa delays, personal reasons).
- Residents at programs that allow flexible Step 3 timing and don’t tie it to licensure in the first year or two.

Content Emphasis: What Dermatology Applicants Should Focus On
USMLE Step 3 is not a dermatology exam; it’s a general clinical practice exam. But as a future dermatologist, you can leverage your strengths while shoring up common weak areas.
Major Content Domains
Internal Medicine and Ambulatory Care
- Hypertension, diabetes, CAD, CHF, COPD, asthma
- Thyroid and endocrine disorders
- Chronic disease follow-up, screening, vaccinations
- Geriatrics, multimorbidity, polypharmacy
Emergency Medicine and Acute Care
- Chest pain, shortness of breath, sepsis, shock
- Acute neurologic deficit, trauma, toxicology
- Immediate stabilization and disposition decisions
Obstetrics & Gynecology
- Prenatal care, pregnancy complications
- Labor, postpartum issues, contraception
- Gynecologic emergencies
Pediatrics
- Well-child visits, vaccination schedules
- Common pediatric infections and rashes
- Growth and development, failure to thrive
Psychiatry and Substance Use
- Depression, anxiety, psychosis, suicidality
- Substance use disorders and withdrawal
- Capacity, safety, and disposition reasoning
Surgery and Orthopedics
- Pre-op risk assessment, post-op complications
- Wound management, DVT prophylaxis
Population Health, Ethics, and Biostatistics
- Study design, bias, risk reduction, NNT, sensitivity/specificity
- Informed consent, autonomy, confidentiality
- Public health interventions and screening criteria
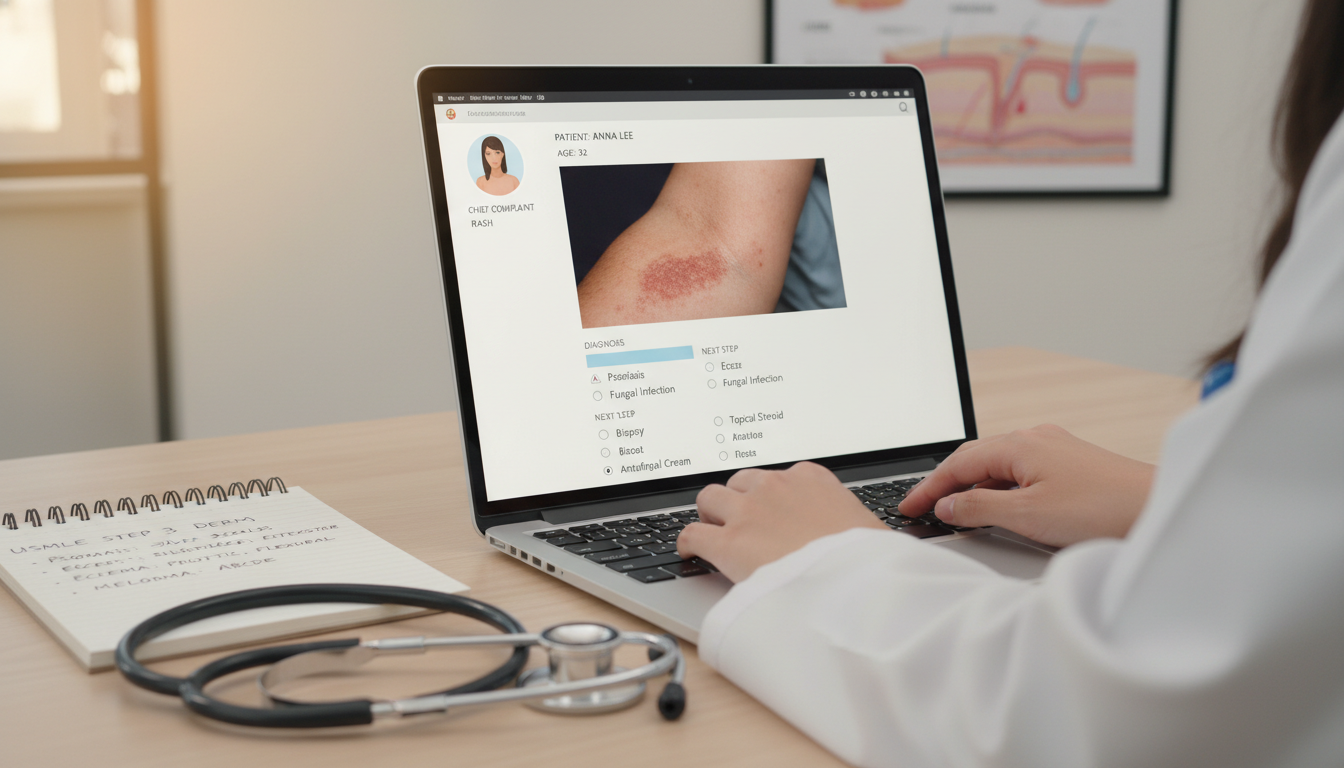
Skin and Dermatology-Related Topics on Step 3
While dermatology content is not dominant, it appears enough that you should recognize it quickly and manage it appropriately:
Acute rashes and eruptions
- Urticaria vs. angioedema vs. anaphylaxis
- Drug eruptions (morbilliform rash, DRESS, SJS/TEN)
- Eczema, psoriasis flares, contact dermatitis
Infections involving skin
- Cellulitis vs. erysipelas vs. abscess
- Necrotizing fasciitis (key red flags, urgent surgical consult)
- Lyme disease rash, RMSF, meningococcemia
Systemic disease with cutaneous signs
- Lupus malar rash, dermatomyositis (heliotrope rash, Gottron papules)
- Vasculitis (palpable purpura)
- Endocrine-related skin changes (Cushing, Addison, diabetes)
Oncology and skin cancer basics
- Melanoma warning signs, biopsy indications
- Basal and squamous cell carcinoma management at a primary care level
You don’t need board-level derm detail, but you must recognize red-flag skin findings and know initial management, when to biopsy, and when to refer urgently.
Building a Derm-Friendly Step 3 Study Plan
Step 1: Clarify Your Deadline and Constraints
Before you choose resources or dive into questions:
- Check state and institutional requirements:
- How long after graduation can you wait to take Step 3?
- Does your program have a required deadline (e.g., by end of PGY-1)?
- Identify personal constraints:
- Heavy ICU or night-float months?
- Research blocks or electives that could serve as “lighter” studying periods?
- Visa-related timing needs?
Write down a target test window and work backwards to develop your timeline.
Step 2: Decide on Overall Study Duration
For most dermatology-bound trainees:
If close to Step 2 CK (within 6–9 months):
- 4–6 weeks of focused prep, 1–2 hours/day on non-call days, more on off days.
If >1 year out from Step 2 CK or significant clinical gap:
- 6–10 weeks of prep, possibly with a short “content-review” stage before heavy question practice.
Step 3: Choose High-Value Resources
You don’t need a huge library—depth beats breadth.
Recommended core resources for USMLE Step 3 preparation:
Question Banks (Qbanks)
- A primary Step 3 Qbank (e.g., UWorld Step 3 or similar) is your central resource.
- Aim to complete at least 60–75% of the Qbank, ideally timed and mixed to simulate the exam.
CCS (Clinical Case Simulations) Practice
- Use the official CCS practice software and cases from your Qbank provider.
- Learn:
- How to order tests efficiently
- When to admit vs. manage outpatient
- Appropriate initial management orders (e.g., oxygen, IV access, monitoring)
- Practice enough cases that you feel comfortable navigating the interface and thinking in “stepwise management.”
Focused Review Summaries
- A concise text or notes focusing on:
- Preventive care guidelines
- OB/GYN, pediatrics, and psych key algorithms
- Biostatistics and ethics
- Avoid overly detailed specialty texts; this is not derm boards.
- A concise text or notes focusing on:
Optional: Quick Dermatology Refreshers
- Brief review of rash algorithms, emergency derm, drug eruptions, and skin infection management.
- This can be as simple as:
- Skimming relevant derm sections in a Step 2 CK book
- Using a short outline or table you create for yourself.
Execution: Day-to-Day Study Strategy for a Busy Derm-Track Trainee
Designing a Practical Weekly Schedule
Example for an intern on a moderately busy rotation:
Weekdays (non-call days):
- 60–90 minutes of Qbank (approximately 1–2 blocks of 10–20 questions)
- Rapid review of explanations, focusing on:
- Why wrong choices were tempting
- Management algorithms and decision thresholds
Weekends or post-call off days:
- One longer block (e.g., 40–60 questions)
- 1–2 CCS cases
- 30–45 minutes of targeted review (statistics, OB, peds, psych)
Key principles:
- Mixed and timed blocks: Simulate the real test; don’t do only system-based, untimed blocks.
- Active notes: Keep a high-yield Step 3 notebook or document with:
- Screening ages and intervals
- Vaccination catch-up schedules
- First-line vs. second-line treatments
- “Do not miss” red-flag signs (e.g., nec fasc, ectopic pregnancy).
Focusing on Your Weakest Areas
As a dermatology-bound trainee, you may be stronger in:
- Pattern recognition
- Ambulatory medicine
- Basic internal medicine and diagnostic reasoning
But you may be relatively weaker in:
- OB/GYN and labor management
- Pediatric vaccine schedules and neonatal issues
- Complex psychiatry and legal/ethical nuances
- Biostats and epidemiology calculations
Use self-assessment exams and Qbank performance analytics to identify and prioritize these weaker areas. Dedicate one focused session per week to each major weak domain.
CCS Strategy for Step 3
CCS is often anxiety-provoking because of its unique format. For dermatology applicants—who may not regularly manage acute inpatient cases during derm training—solid CCS performance helps compensate.
Core CCS habits:
Always stabilize first:
- Airway, breathing, circulation, pain control, monitoring (cardiac monitor, pulse oximetry), IV access.
Know “automatic” orders for key presentations:
- Chest pain: EKG, troponin, aspirin (unless contraindicated), oxygen if hypoxic, beta-blocker depending on scenario.
- Suspected sepsis: Cultures, broad-spectrum antibiotics, fluids, lactate, source control.
- Pregnancy bleeding or abdominal pain: Pregnancy test, transvaginal ultrasound, Rh status.
Advance time thoughtfully:
- Reassess after key labs return or after therapy is started.
- Move the clock forward enough to see intervention effects, but not so far you miss necessary monitoring.
Use inpatient vs. outpatient appropriately:
- Admit for unstable vitals, concerning imaging, high-risk conditions (e.g., SJS/TEN, status asthmaticus).
- Follow up outpatients at reasonable intervals (e.g., 2–4 weeks for chronic condition titrations).
Practice enough cases to build patterned responses—you want your brain free to think about content, not button-clicking.
USMLE Step 3 During Dermatology Residency: Special Considerations
If you’re taking Step 3 during derm residency, your needs differ slightly from an intern’s.
Choosing the Right Rotation
Aim for:
- Lighter, more predictable months:
- Outpatient clinics with minimal call
- Research or academic blocks
- Electives without heavy inpatient responsibilities
Avoid:
- First month of derm residency (you’re still adjusting)
- Very procedure-heavy or cosmetic blocks if your program has them early—and you want to maximize learning
- Times when major conferences, presentations, or board review sessions are clustered
Integrating Derm Learning with Step 3 Prep
You can leverage Step 3 preparation to support derm learning:
When Step 3 presents a rash or lesion, take an extra minute after review to:
- Look at a few clinical images for the diagnosis.
- Read 1–2 key derm pearls (distribution, morphology, distinguishing features).
During derm clinic:
- Mentally practice “Step 3-style” reasoning:
- If this were a primary care setting, what would be the correct initial step?
- When is biopsy indicated?
- When is urgent admission vs. outpatient follow-up appropriate?
- Mentally practice “Step 3-style” reasoning:
This dual mindset sharpens both derm and Step 3 clinical judgment.
Impact on Derm Match and Long-Term Career
For those still in the match pipeline (e.g., applying for advanced dermatology positions while in a TY year):
A clean, first-attempt Step 3 pass:
- Prevents negative red flags in your application.
- Reassures programs you won’t struggle professionally with licensure requirements.
A strong score (if reported) can be an additional signal of:
- Good test-taking skills and clinical reasoning
- Consistency with strong Step 1/2 performance, or improvement after earlier weaker scores
Once in dermatology residency:
- Having Step 3 completed:
- Frees you to concentrate on derm boards, research productivity, procedural skills, and fellowship exploration.
- May allow you to moonlight where permitted, which can be financially and educationally beneficial.
Frequently Asked Questions (FAQ)
1. Does Step 3 score really matter for dermatology residency?
For most applicants, Step 3 is not a primary selection tool for derm match. Step 1 and Step 2 CK, research, letters, and derm-specific experiences carry more weight.
However, your Step 3 pass/fail status and number of attempts matter:
- Multiple failures can raise concerns about future licensing exams (e.g., dermatology boards).
- A strong Step 3 performance can help reassure programs if you previously had borderline scores or are a reapplicant.
2. Should I take Step 3 before or after matching into dermatology?
If feasible and allowed by your state and institution, taking Step 3 during late MS4 or early internship is often ideal:
- Your Step 2 CK knowledge is fresh.
- You can clear the exam before derm residency.
- It may help with visa options and match flexibility.
If that’s not feasible, plan for early in internship with a lighter rotation, rather than postponing to a busy derm year unless you have no alternative.
3. What’s the best way to balance intern year duties with Step 3 study?
- Protect a consistent daily minimum (even 45–60 minutes can work).
- Choose a less demanding rotation around your test date.
- Focus on Qbank + CCS as your core, rather than spreading yourself across many resources.
- Use clinical experiences to reinforce learning: when you see a patient with COPD or gestational diabetes, quickly review the Step-3-level management algorithm.
4. I’m an IMG aiming for dermatology. Is Step 3 more important for me?
It often is:
- Many programs that sponsor H-1B visas require Step 3 before they can rank or onboard you.
- Having Step 3 passed before interview season can expand your program list and simplify visa discussions.
- A strong Step 3 performance provides additional evidence of clinical readiness and professional reliability, which can be particularly valuable in a competitive specialty like dermatology.
By approaching USMLE Step 3 preparation with a structured plan tailored to your dermatology trajectory—choosing smart timing, using high-yield resources, and integrating studying with your clinical schedule—you can complete this final USMLE hurdle efficiently. Doing so protects your bandwidth for what matters most: becoming an excellent dermatologist and positioning yourself strongly in the derm match and beyond.






















