
Understanding Step 3 in the Context of Medicine-Psychiatry
USMLE Step 3 is often framed as an exam about “independent practice,” but for a med psych residency applicant or resident, it’s more than just a box to check. It influences visa status, licensure timelines, fellowship applications, and even how confidently you manage complex patients who sit squarely at the medicine–psychiatry interface.
What Step 3 actually tests
Step 3 is a two-day exam with two broad components:
Day 1 – Foundations of Independent Practice (FIP)
- Focus: Basic medical knowledge, pathophysiology, epidemiology, biostatistics, and ethics.
- For med psych: Many questions feel like advanced Step 2 CK, with heavy internal medicine, some neurology, some psych, and public health/quality improvement.
Day 2 – Advanced Clinical Medicine (ACM)
- Focus: Diagnosis and management, clinical decision making, and Computer-based Case Simulations (CCS).
- For med psych: Rich in primary care, chronic disease management, ER/urgent care scenarios, and psychosocial factors (substance use, adherence, safe discharge planning, etc.).
For a medicine psychiatry combined trainee, Step 3 is an opportunity to demonstrate you can:
- Integrate medical and psychiatric reasoning under time pressure.
- Make safe, guideline-concordant decisions in complex biopsychosocial cases.
- Prioritize workup and management in patients with multimorbidity (e.g., COPD, diabetes, and bipolar disorder).
Why Step 3 matters uniquely in med psych residency
Licensure and moonlighting:
Many states require Step 3 for an unrestricted license, which can affect your ability to moonlight during upper years of residency.Immigration/visa issues (for IMGs):
Some visa categories or institutional policies expect completion of Step 3 early in residency.Program expectations:
Combined medicine-psychiatry programs may:- Encourage Step 3 completion during PGY-1 or early PGY-2.
- Use performance to identify residents who might benefit from academic support.
Clinical preparedness:
Step 3’s emphasis on chronic disease management, emergency stabilization, and psychosocial factors is directly relevant to:- Med-psych inpatient units
- Consultation-liaison psychiatry
- Primary care–behavioral health integration settings
Understanding these stakes helps you plan not just to pass, but to use Step 3 preparation as a scaffold for your med psych clinical growth.
When to Take Step 3 During a Medicine-Psychiatry Residency
Timing is a strategic decision. For medicine psychiatry combined trainees, it must fit across both medicine and psychiatry rotations, call schedules, and personal life.
Common timing scenarios
Late PGY-1 (intern year)
- Pros:
- Step 2 CK knowledge is still fresh.
- Frees up mental space in later years for electives, research, or fellowship planning.
- Helps IMGs with visa or licensure needs.
- Cons:
- You are still adapting to residency workflow and call.
- Less exposure to psychiatry and longitudinal primary care may make some psychosocial/ambulatory questions feel less intuitive.
- Pros:
Early PGY-2
- Pros:
- A stable base of inpatient medicine and initial psych exposure.
- Better feel for real-world decision making, which aligns with Step 3’s emphasis.
- Still early enough that Step 2 CK–level content is relatively fresh.
- Cons:
- PGY-2 responsibilities and night float may complicate study scheduling.
- Overlaps with increased autonomy and, in some programs, heavier rotations.
- Pros:
Late PGY-2 or PGY-3
- Pros:
- More clinical maturity in both medicine and psychiatry.
- Broader exposure to integrated care (CL psych, med-psych clinics) that maps well to exam scenarios.
- Cons:
- Risk of knowledge drift from Step 2 CK fundamentals (micro, biostats, etc.).
- Competes with evolving interests: fellowship applications, scholarly projects, leadership roles.
- Pros:
How to choose the best time for you
Use these factors to guide timing of Step 3 during residency in a med-psych program:
Current cognitive bandwidth:
Are you still in “exam mode” from Step 2 CK? Or are you mentally burnt out and need a few months before restarting high-intensity study?Rotation schedule:
Aim to prepare during:- A lighter outpatient block
- Or a psychiatry month with relatively predictable hours
Avoid: New ICU or night float blocks if possible.
Program culture and requirements:
- Some med psych programs explicitly want Step 3 done before the end of PGY-2.
- Ask seniors when residents typically take it and what has worked (or not).
Personal circumstances:
- Major life events (moving, weddings, children, health issues) might make a given period suboptimal.
- For IMGs, coordinate with GME and institutional policies on Step 3 timelines—especially if linked to visa extensions.
Actionable step:
Within your first 3–6 months of residency, sketch a 12–18 month academic plan that includes:
- Tentative Step 3 window
- High-yield study blocks
- Time-off requests for test days
Then review it with your program director or advisor, ideally one who understands the med psych residency structure.

Building an Integrated Step 3 Study Plan for Med-Psych Residents
A strong Step 3 preparation strategy for medicine-psychiatry trainees must be realistic about time, emphasize integration, and make test-prep reinforce your daily clinical work instead of competing with it.
Step 1: Establish your baseline
Before designing a plan:
Review your Step 2 CK experience:
- Which sections were weak (e.g., psychiatry, biostats, OB/GYN)?
- Did timing or test anxiety play a role?
Take a self-assessment:
- Use NBME or UWorld self-assessments within the first 1–2 weeks of studying.
- Note:
- Overall score range vs passing cutoff
- Domains that underperform (e.g., endocrine, renal, psych, emergency care)
- Timing issues
Inventory your schedule:
- How many “protected” study hours can you reliably carve out per week (not theoretical, but realistic)?
- Consider:
- Call
- Commute time
- Family responsibilities
Step 2: Choose core resources (less is more)
Avoid resource overload. A focused list is enough:
Question banks (non-negotiable):
- UWorld Step 3 Qbank
- Primary resource; aim to complete at least 80–100% of questions.
- Do timed, random blocks to simulate test conditions.
- Optional: Amboss Step 3 for targeted reinforcement if you learn well from their articles.
CCS practice:
- Official NBME/USMLE CCS cases and practice software.
- A dedicated CCS resource (e.g., CCS cases from UWorld or a reputable prep company).
- Practice until:
- You are comfortable with opening moves.
- You can systematically order appropriate tests/consults.
- You know when to advance time and adjust treatment.
Text and review material (select one main resource):
- High-yield Step 3 review book or concise notes.
- For med psych, supplement with:
- A quick psychiatry handbook (e.g., pocket psych or CL psych guide)
- Short reference on psychotropic medications in medically ill patients
Step 3: Create a 6–10 week study framework
A pragmatic schedule for a busy medicine psychiatry combined resident:
Weeks 1–2: Foundation and structure
- 20–30 UWorld questions/day (timed, mixed, or by system if you prefer).
- Start CCS orientation: complete tutorial and 2–3 practice cases.
- Daily 30–45 minutes of:
- Biostatistics
- Ethics and patient safety
- Use commute or downtime for quick review (anki, phone-based qbank review).
Weeks 3–6: Peak question volume
- 40–60 UWorld questions/day, 5–6 days/week.
- 2–3 CCS cases per week.
- Identify weak domains (e.g., OB, peds, psych emergencies) and schedule targeted review sessions.
- Weekly plan:
- 1 focused block on psychiatry / neuro / addiction content.
- 1 block on chronic medical conditions in psychiatric patients (diabetes, HTN, CAD, COPD).
- 1 session on cross-cutting issues: substance use, adherence, social determinants.
Weeks 7–8 (and 9–10 if you extend): Refinement
- Self-assessment exam to gauge readiness.
- Prioritize:
- Remaining weak areas.
- Full-length timed blocks.
- CCS fluency—at least 10–15 cases completed by now.
- Practice 1–2 “mock half-days”:
- Several question blocks + CCS cases back-to-back.
Step 4: Align daily clinical work with Step 3 prep
As a med psych resident, your clinical environment is an active study tool.
When you see a patient:
On medicine service with psychiatric comorbidity:
- Think: “How would this case appear on Step 3?”
- Example: A patient with COPD, heart failure, and severe depression refusing medications.
- Exam angle: medication adherence strategies, risk assessment (self-harm), optimizing heart failure therapy, addressing barriers to care.
On inpatient psychiatry:
- Think about:
- Medical screening for psych admissions.
- QTc monitoring with antipsychotics.
- Workup of first-episode psychosis (e.g., rule out thyroid disease, B12 deficiency).
- Ask: What would Step 3 test about this scenario?
- Think about:
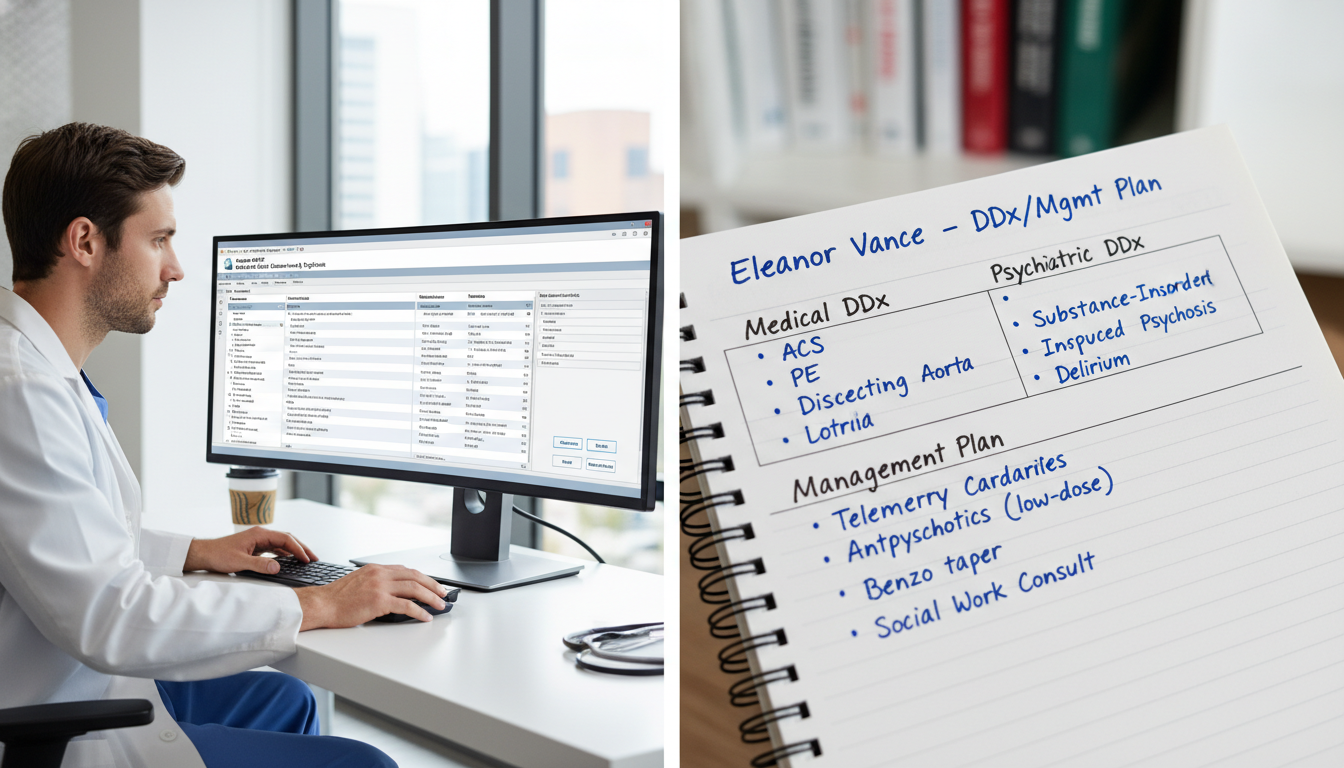
On CL psychiatry or med-psych unit:
- Treat every consultation as a potential exam question:
- Capacity evaluations
- Delirium vs psychosis vs dementia
- Substance withdrawal with concurrent medical illness
- Treat every consultation as a potential exam question:
Consciously linking real cases with exam-style reasoning builds the mental “scripts” Step 3 expects you to use quickly and safely.
High-Yield Clinical Themes for Medicine-Psychiatry on Step 3
While Step 3 remains broad, med psych residents benefit from extra focus on topics that bridge medicine and psychiatry.
1. Medical management in patients with psychiatric illness
Expect cases where psychiatric comorbidity alters standard medical care.
Key areas:
Chronic disease + psychiatric nonadherence
- Example: Uncontrolled diabetes in a patient with schizophrenia.
- Be ready to:
- Prioritize safety (check for DKA/HHS).
- Optimize regimens (simplify insulin schedules if needed).
- Consider social supports, visiting nursing, case management.
- Integrate motivational interviewing strategies (often in answer choices).
Side effects of psychotropics with medical implications
- Antipsychotics:
- Metabolic syndrome, weight gain, dyslipidemia, hyperglycemia.
- QTc prolongation (know cutoffs and monitoring).
- Lithium:
- Renal function, thyroid function, toxicity risk (NSAIDs, ACEi, diuretics).
- SSRIs/SNRIs:
- Hyponatremia, bleeding risk with NSAIDs/anticoagulants, serotonin syndrome.
- Antipsychotics:
Pregnancy and psychotropics
- Cases may ask:
- Which medications to continue, switch, or avoid.
- Risk–benefit of maintaining SSRI vs relapse.
- Postpartum depression screening and management options while breastfeeding.
- Cases may ask:
2. Psychiatric emergencies in medically ill patients
Step 3 frequently tests risk assessment and safety, especially in complex patients.
Must-know scenarios:
Suicidal ideation in a medically hospitalized patient
- Safe disposition: one-to-one observation, psych consult, restriction of lethal means.
- When to involuntarily hospitalize: imminent risk, inability to contract for safety.
Agitated delirium vs primary psychosis
- Distinguish:
- Acute onset, fluctuating course, inattention → delirium.
- Gradual onset, stable vitals, normal labs → more likely psychiatric.
- Management:
- Address underlying medical cause (infection, medications).
- Use low-dose antipsychotics for severe agitation; avoid benzodiazepines except in withdrawal states.
- Distinguish:
Substance intoxication and withdrawal
- Alcohol withdrawal:
- CIWA scoring, benzodiazepine treatment, thiamine before glucose.
- Opioid use disorder:
- Safe prescribing of opioids, initiation of buprenorphine (in some Step 3 cases), harm-reduction strategies.
- Stimulant intoxication:
- Treat agitation and hypertension, monitor for MI or stroke.
- Alcohol withdrawal:
3. Capacity, consent, and ethics
Medicine psychiatry combined residents will recognize how often capacity questions arise.
Core principles to master:
- Capacity is decision-specific and can fluctuate.
- Assess:
- Understanding
- Appreciation
- Reasoning
- Ability to express a choice
- On the exam:
- Do not equate psychiatric diagnosis with lack of capacity.
- Use surrogates or advance directives only when capacity is clearly absent.
- Protect patient autonomy while ensuring safety.
4. Integration of psychosocial and social determinants of health
Step 3 increasingly tests real-world barriers to care:
- Housing instability, food insecurity, limited health literacy.
- Insurance constraints and access to medications.
- Cultural considerations and language barriers.
As a med psych resident, you already see this daily. For test questions, choose options that:
- Acknowledge and address barriers.
- Use interdisciplinary collaboration (social work, case management, addiction services).
- Avoid dismissive or punitive approaches to nonadherence.
CCS Strategy and Test-Day Tactics for Med-Psych Residents
Many residents underestimate the Computer-based Case Simulations (CCS) portion of the USMLE Step 3, yet efficient CCS performance can significantly boost your score.
CCS basics to master
Each CCS case simulates a clinical encounter over minutes to months of “simulated time.” Your goals:
- Stabilize the patient.
- Make appropriate diagnostic decisions.
- Initiate evidence-based treatment.
- Disposition safely (admit vs discharge; floor vs ICU vs psych unit).
For med psych cases, common themes include:
- Suicidal ideation in the ED.
- Agitation with suspected delirium or substance withdrawal.
- Chest pain or shortness of breath in a patient on multiple psychotropics.
- New-onset confusion or mania related to medications, endocrine disorders, or infection.
CCS approach you can apply broadly
Initial orders (first 1–2 minutes):
- Vital signs, physical exam, mental status exam.
- For unstable patients: O2, IV access, monitor, glucose check, EKG.
- In psych/med overlap:
- Evaluate for delirium (orientation, attention).
- Assess for self-harm risk (if feasible and safe).
Diagnostic workup:
- Order targeted labs and imaging.
- Don’t forget:
- Basic metabolic panel, CBC, LFTs.
- Thyroid studies if mood/psychosis vs medical cause is unclear.
- Toxicology screen and serum levels where appropriate (e.g., lithium, valproate).
Therapeutic orders:
- For agitation:
- Use evidence-based doses of antipsychotics.
- Avoid contraindicated meds (e.g., benzodiazepines in active delirium unless withdrawal).
- For depression with suicidality:
- Consider inpatient psych admission, safety measures, and appropriate antidepressant if indicated.
- For agitation:
Consults and multidisciplinary care:
- Use psychiatry consult in appropriate medical cases.
- Use social work, addiction medicine, or case management for complex psychosocial issues.
- CCS rewards appropriate and timely consults—not overuse.
Time advancement and follow-up:
- Advance time after ordering key tests.
- Reassess vitals, labs, and mental status regularly.
- Adjust treatment based on clinical response (e.g., titrating benzodiazepines in withdrawal).
Test-day strategy: Surviving two long days
Day 1 tips:
- Emphasize stamina: plan meals, hydration, and pacing.
- Don’t obsess over any single question; move on once you’ve chosen the best of the options.
- For ethics and systems questions, think:
- Safety first.
- Evidence-based practice.
- Respect for autonomy and patient-centered care.
Day 2 tips (includes CCS):
- Adjust sleep the night before to be fully alert.
- For CCS:
- Don’t panic if you “finish early”; use remaining time to double-check orders and ensure follow-up.
- If stuck, go back to fundamentals: stabilize, diagnose, treat, disposition.
General exam-day advice for med psych residents:
- Avoid using highly idiosyncratic or cutting-edge practices from your institution that aren’t mainstream yet; Step 3 usually lags a bit behind current controversies.
- For ambiguous psychiatry cases, choose:
- The safest, least restrictive option that adequately protects the patient and others.
- Standard-of-care pharmacologic choices over off-label outliers.
Balancing Wellness, Burnout, and Step 3 During Med-Psych Residency
Med psych residents face a unique emotional load: heavy medical acuity plus psychiatric complexity. Adding intensive USMLE Step 3 preparation can push you toward burnout if not managed deliberately.
Protecting your bandwidth
Set realistic daily goals:
- Instead of “I’ll do 80 questions every day,” aim for:
- “I’ll do 40 questions on heavy call days; 60–80 on lighter days.”
- Build in one lighter study day per week.
- Instead of “I’ll do 80 questions every day,” aim for:
Use micro-studying:
- 10–15 question blocks while waiting for sign-out or between consults (only when truly free, not at the expense of patient care).
- Flashcards for key psych and medicine interactions (e.g., QT-prolonging combos, dangerous drug–drug interactions).
Leverage peer support:
- Study with another med psych resident if possible.
- Do occasional group case discussions:
- Present a complex inpatient med-psych patient.
- Ask: “What would Step 3 test in this scenario?”
Recognize signs of burnout:
- Emotional exhaustion.
- Cynicism or detachment.
- Reduced sense of accomplishment. When these appear, scale back, talk to faculty mentors, and use institutional wellness resources.
Getting your program on board
Med psych programs benefit when their residents pass Step 3 smoothly. Ask for:
- A relatively lighter block during your peak study weeks.
- Faculty recommendations on Step 3 prep specific to your institution’s patient population.
- Formal or informal “Step 3 pearls” teaching sessions during noon conference or didactics.
Being transparent with your chiefs and program leadership about your Step 3 during residency plan can help prevent scheduling conflicts and reduce your stress.
FAQs: USMLE Step 3 Preparation in Medicine-Psychiatry
1. How long should I study for Step 3 as a med psych resident?
Most medicine psychiatry combined residents do well with 6–10 weeks of focused preparation, averaging 1–3 hours per day depending on rotation intensity. If your Step 2 CK score was marginal or you’ve had a long gap since taking exams, plan closer to 10–12 weeks with a strong emphasis on fundamentals and question practice.
2. Is Step 3 harder for medicine-psychiatry residents compared to categorical internal medicine or psychiatry residents?
Not inherently. In fact, med psych residents often find integrated and psychosocially complex questions more intuitive. The challenge is time management, because your training is split across two disciplines. If you maintain a solid foundation in general medicine and reinforce psych knowledge through your daily work, you’re well-positioned to succeed.
3. Which question bank is best for Step 3 preparation?
For most residents, UWorld Step 3 remains the primary resource and is sufficient when used thoroughly. Amboss or other banks can be helpful adjuncts if you finish UWorld early or prefer their article-style explanations. The key is to fully commit to one high-quality qbank, complete most or all questions in timed mode, and thoroughly review explanations.
4. How much psychiatry is on Step 3, and how should I prepare for it?
Psychiatry typically comprises a moderate portion of Step 3, often embedded within primary care and emergency scenarios. For a med psych resident, specific focus areas should include:
- Depression, bipolar disorder, anxiety disorders, psychosis.
- Substance use disorders and withdrawal states.
- Capacity, consent, and involuntary treatment.
- Management of psychotropics in medically ill patients (side effects, interactions, monitoring).
Leverage your psych rotations and CL consult experiences; mentally reframe complex patients as Step 3 vignettes and actively practice articulating diagnostic criteria and first-line treatments.
By planning your USMLE Step 3 preparation thoughtfully, integrating it with your med psych clinical experiences, and focusing on high-yield, cross-disciplinary themes, you can not only pass the exam but also strengthen the very skills that define an excellent medicine-psychiatry physician.






















