Why Step 3 Matters for Neurology Residency and Beyond
USMLE Step 3 is often treated as “just the last exam,” but for neurology residents it plays a more strategic role than many realize.
How Step 3 fits into neurology training and the neuro match:
For the neurology residency application (neuro match):
- Most programs do not require Step 3 for initial ranking, but:
- A strong Step 3 score can help offset a weaker Step 1 or Step 2 CK.
- Passing Step 3 before PGY-2 can reassure PDs about your ability to pass future board exams.
- For IM/Transitional Year + Neurology pathways (categorical vs advanced):
- Some advanced neurology programs prefer applicants who have passed or scheduled Step 3 during internship.
- Most programs do not require Step 3 for initial ranking, but:
For residency progression and licensure:
- Many states require USMLE Step 3 for unrestricted medical licensure, which you’ll need by PGY-3 or PGY-4 in many neurology programs.
- Some institutions link Step 3 passage to promotion or eligibility for moonlighting.
For long-term neurology career:
- Step 3 is less “neuro-heavy” than you might hope. However:
- It tests your ability to manage neurologic problems in the context of the whole patient (cardiac risk, pregnancy, anticoagulation, ICU care, etc.).
- It’s a rehearsal for the style of ABPN neurology boards: broad, management-focused, and highly clinical.
- Step 3 is less “neuro-heavy” than you might hope. However:
Understanding this context helps you set a smart strategy: passing once, efficiently, at a time that supports your neurology residency rather than competes with it.
Understanding Step 3: Structure, Timing, and What’s Different from Step 2
Before diving into Step 3 preparation, you need to understand how this exam is built and how it differs from Step 2 CK, especially for neurology-focused trainees.
Exam Structure Overview
USMLE Step 3 is a two-day exam:
Day 1 – Foundations of Independent Practice (FIP):
- Focus:
- Basic medical science as applied to clinical practice
- Diagnosis, initial workup, epidemiology, ethics, biostatistics
- Format:
- Multiple-choice questions (MCQs) only
- ~6–7 blocks, ~38–40 questions per block
- 7 hours total testing time
Day 2 – Advanced Clinical Medicine (ACM):
- Focus:
- Management, prognosis, monitoring, and follow-up decisions
- Complex and multi-system patients
- Format:
- MCQs in multiple blocks
- Clinical Case Simulations (CCS) – interactive patient management cases
- ~9 hours total testing time
How Step 3 is Different from Step 2 CK
From a neurology resident’s perspective, the differences are important:
Emphasis on management over diagnosis
- Step 2 CK: “What’s the diagnosis?” and “What initial test do you order?”
- Step 3: “How do you manage this patient over time?” including:
- Admission vs outpatient decision
- Starting, adjusting, or stopping medications
- Monitoring toxicity and side effects
- Long-term follow-up and preventive care
Systems-based and generalist-oriented
- Even as a neurology resident, expect:
- A lot of internal medicine, pediatrics, and OB/GYN.
- Neuro questions embedded in systemic disease (e.g., seizure in pregnancy, stroke in AFib, neuropathy in diabetes).
- You’re tested as a general physician who can manage common conditions, not just a neurologist.
- Even as a neurology resident, expect:
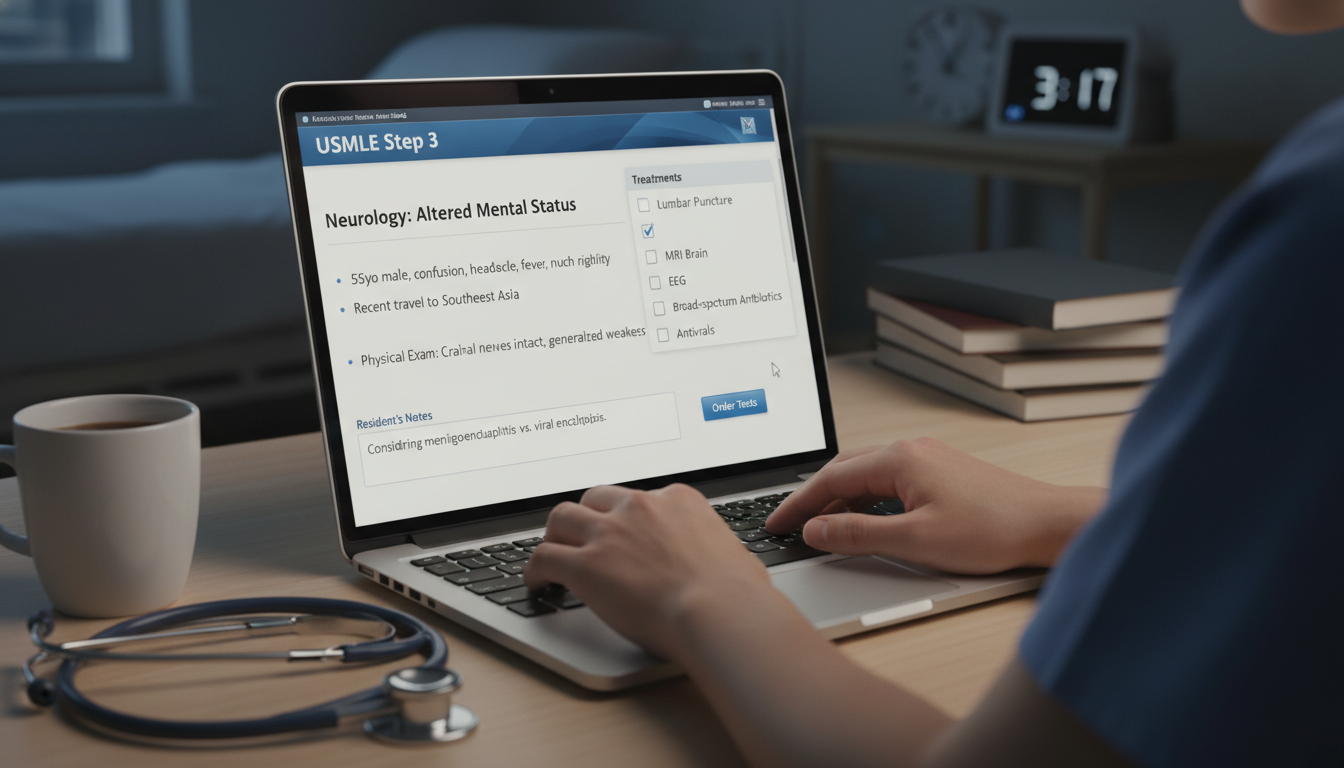
CCS cases are unique
- You will order tests, medications, and interventions in real time.
- Neurology is frequently represented: stroke, status epilepticus, meningitis/encephalitis, trauma, delirium.
- You’re graded on:
- Correct and timely actions
- Avoiding harmful or unnecessary testing
- Logical sequence of stabilization → diagnosis → management → follow-up
When to Take Step 3 During Neurology Residency
Timing is one of the most strategic decisions you’ll make.
1. Before Neurology Residency (During Intern Year)
Common for categorical IM + Neuro or TY + Neuro pathways.
Pros:
- Knowledge from Step 2 CK is still relatively fresh.
- Some IM or TY programs actively encourage/require Step 3 during residency, usually by the end of PGY-1.
- Clears USMLE requirements early, letting you focus on neurology boards later.
Cons:
- Intern year is demanding; balancing call, ICU rotations, and study time can be stressful.
- You may feel insecure about areas you haven’t rotated in yet (e.g., pediatrics, OB/GYN).
Best candidates:
- Graduates with a solid Step 2 CK foundation.
- Those in programs with predictable schedules and protected study time.
- Applicants to neurology fellowships who want Step 3 out of the way early.
2. Early Neurology Residency (PGY-2)
Pros:
- You have more clinical maturity.
- You’ve seen many neurologic emergencies (stroke, seizure, status, neuro-ICU).
- Still relatively close to medical school across other disciplines.
Cons:
- You’re adjusting to neurology call, consults, and ICU rotations.
- Cognitive load is heavy learning specialty content and hospital systems.
Best candidates:
- Neurology residents who finished intern year with strong general medicine but need a bit more time to stabilize their schedule.
- Those whose states or programs require Step 3 for early licensure or moonlighting.
3. Mid to Late Neurology Residency (PGY-3 or PGY-4)
Pros:
- Strong clinical experience; you can easily reason through management decisions.
- Supports cognitive overlap with board exam prep strategies.
Cons:
- Farther from core pediatrics, OB/GYN, and some outpatient IM.
- Step 3 can feel like a distraction from neurology boards/fellowship application.
- Risky if your program or state requires Step 3 earlier for promotion or licensure.
Best candidates:
- Residents who absolutely need additional time (e.g., family reasons, remediation, research focus).
- International graduates who need more clinical exposure in the U.S. before attempting Step 3.
Practical Timing Advice for Neurology Residents
- Aim to take USMLE Step 3 by the end of PGY-2 if possible.
- This generally balances retained general medicine knowledge with enough neurology exposure to handle complex neuro cases confidently.
- Plan to study during:
- Lighter outpatient blocks
- Electives with predictable daytime hours
- Periods away from neuro-ICU and night float
- Discuss with:
- Your neurology program director and chief residents.
- Former residents in your program who can tell you when most neurology residents take Step 3 and what worked best.

High-Yield Content Areas for Neurology Residents
Even though Step 3 is a general exam, you can and should use your neurology background to your advantage.
1. Core Neurology Topics That Frequently Appear
Focus on clinical reasoning and acute management:
Stroke and TIA
- Inclusion/exclusion criteria for IV thrombolysis (tPA/tenecteplase).
- Time windows and imaging requirements (non-contrast CT, CTA, CT perfusion).
- Blood pressure management pre- and post-thrombolysis or thrombectomy.
- Secondary prevention: antiplatelets vs anticoagulation, statins, carotid interventions.
Seizure and Status Epilepticus
- First-time seizure workup: labs, imaging, EEG indications.
- Stepwise management of status:
- Benzodiazepines → IV antiepileptics → intubation and anesthetic infusions.
- Pregnancy and epilepsy: teratogenic medications, folate, seizure vs eclampsia.
Headache and Migraine
- Red flag features (thunderclap, fever, focal deficit, immunosuppression).
- Proper use of CT vs MRI vs LP.
- Migraine acute and preventive therapy.
Neuromuscular Emergencies
- Myasthenic crisis vs cholinergic crisis.
- Guillain-Barré syndrome: respiratory monitoring (NIF, VC), indications for IVIG/plasmapheresis.
- Spinal cord compression: steroids, emergent MRI, neurosurgery involvement.
Infectious Neurology
- Meningitis/encephalitis: when to get CT before LP, empiric antibiotic and antiviral regimens.
- Brain abscess: imaging, when to avoid LP, surgical consults.
Actionable tip: For each of these categories, build simple 1-page algorithms (e.g., “Stroke at 2 hours from onset: what do I do?”) and revisit them several times during your Step 3 preparation.
2. Non-Neurology Areas That Neurology Residents Often Need to Revisit
Neurology residents tend to be under-prepared in these for Step 3:
Obstetrics and Gynecology
- Prenatal care, screening, management of preeclampsia/eclampsia.
- Early pregnancy complications and ectopic pregnancy.
- Contraception choices, especially in women with chronic illnesses (epilepsy, migraines).
Pediatrics
- Vaccination schedules and catch-up.
- Common pediatric infections, neonatal jaundice.
- Pediatric seizures and febrile seizure management.
General Internal Medicine
- Hypertension, diabetes, dyslipidemia—long-term management and follow-up.
- Anticoagulation: DOACs vs warfarin, bridging, management around procedures.
- Infectious disease basics: pneumonia, UTI, endocarditis.
- Renal and hepatic dosing adjustments for medications.
Psychiatry and Substance Use
- Depression, anxiety, bipolar, and psychosis management.
- Substance withdrawal syndromes, acute intoxications.
Strategy: Make a list of content areas you haven’t touched since medical school and deliberately build them into your study schedule (e.g., “Peds + OB/GYN on weekends”).
3. Ethics, Biostatistics, and Systems-Based Practice
Step 3 includes questions on:
- Medical ethics (capacity, consent, confidentiality, minors).
- Quality improvement, patient safety (checklists, root cause analysis).
- Biostatistics: hazard ratios, odds ratios, confidence intervals, NNT/NNH.
- Practice-based learning (screening recommendations, guideline-based care).
These are often high-yield “easy points” if you review the basics systematically.
Building an Effective Step 3 Study Plan as a Neurology Resident
Now that you know what’s on the exam, let’s structure how to prepare—efficiently and realistically—around residency.
1. Define Your Timeframe
Ask yourself:
- How many weeks can you realistically dedicate to focused USMLE Step 3 preparation?
- How many hours per week (not per day) are sustainable with your rotation schedule?
Typical effective ranges:
- 4–6 weeks (40–80 hours total) for those close to medical school with strong Step 2.
- 8–10 weeks (80–120 hours total) for those further out, with more gaps in OB/peds/IM.
Avoid overlong timelines (e.g., 4–6 months) unless you’re only studying very lightly once a week; burnout and content drift are real.
2. Core Resources: Keep It Simple
You don’t need a library; you need focus. For most neurology residents, a lean but deep resource list works best:
Question Bank (QBank) – Non-negotiable
- UWorld is the standard and generally sufficient alone.
- Target:
- 1 full pass of the Step 3 QBank (≈1,600–2,000 questions).
- Mode:
- Start in tutor mode to learn.
- In the final 2 weeks, shift to timed blocks simulating the exam.
CCS Practice
- Official USMLE CCS interactive cases (highly recommended).
- Supplement with a structured CCS guide (e.g., online CCS strategy resources or a dedicated Step 3 CCS book).
Concise Review Text/Video (Optional but often helpful)
- Use only if you have specific weak content areas.
- Many residents prefer system-based video reviews or a concise IM review text.
Step 3 CCS Templates
- Create or download templates/checklists for common CCS patterns (e.g., chest pain, stroke, DKA, sepsis, seizure).
3. Weekly Structure Example
A realistic 6-week plan for a busy neurology resident:
Weeks 1–2: Foundation and Coverage
- 15–20 QBank questions per day on weekdays; 40–60 per day on 1 weekend day.
- Use tutor mode; read explanations thoroughly.
- Tag or notebook:
- Neurology pearls
- OB/peds/IM areas you keep missing
Weeks 3–4: Integration + CCS Introduction
- Increase to 20–30 Qs/day on weekdays, 60–80/day one weekend day.
- Start CCS practice: 2–3 cases every other day.
- Take one self-assessment (NBME or UWorld simulation if available) to gauge progress.
Weeks 5–6: Simulation and Refinement
- Focus on:
- Timed question blocks (38–40 questions per block).
- Daily CCS practice.
- Identify top 3–5 weak content areas and schedule targeted review sessions.
- Use the week before the exam for:
- One more self-assessment.
- Light review of notes, algorithms, and ethics/biostatistics.
4. Daily Routine Principles for Residents
- Short, consistent sessions (e.g., 1–2 hours) are better than intermittent long marathons.
- Use “micro-study” blocks:
- 10–15 minutes between consults or during downtime to read 2–3 question explanations.
- Protect:
- One larger study block per week (e.g., Saturday morning) for CCS and deeper review.
Mastering CCS (Clinical Case Simulations) with a Neurology Lens
CCS often feels unfamiliar but is very learnable. It can significantly boost your Step 3 score if you approach it systematically.
1. CCS Fundamentals
Each case requires you to:
- Stabilize the patient
- ABCs: airway, breathing, circulation.
- Immediate interventions: oxygen, IV access, EKG, monitoring.
- Order appropriate initial tests
- Labs, imaging, cultures, etc.
- Initiate treatment
- Medications, fluids, emergency medications (e.g., tPA, lorazepam).
- Advance time appropriately
- Minutes, hours, days based on case.
- Reassess symptoms, vitals, labs.
- Disposition and follow-up
- Admit level (ICU vs floor) or outpatient follow-up schedule.
- Counseling, screening, preventive care.
2. Common Neurology-Related CCS Patterns
You’re likely to encounter neurology and neuro-adjacent issues. Practice templates for:
Acute stroke
- ED orders: vitals, oxygen, IV access, cardiac monitor, EKG, glucose, CT head non-contrast, PT/INR, CBC, BMP.
- NPO, neuro checks, head-of-bed elevation.
- Thrombolysis or thrombectomy decisions based on time window and imaging.
- ICU admission for post-tPA monitoring.
Seizure or status epilepticus
- Immediate: airway assessment, IV access, fingerstick glucose, thiamine/glucose if needed.
- Benzodiazepines → IV antiepileptic (e.g., levetiracetam, fosphenytoin).
- Imaging (CT head), labs, EEG, LP if infection suspected.
- Management of triggers: infection, medication withdrawal, metabolic issues.
Meningitis/encephalitis
- Immediate empiric antibiotics after blood cultures.
- CT head before LP if focal deficits or papilledema.
- Addition of steroids and antivirals when appropriate.
For each, write a stepwise checklist and rehearse until it’s automatic.
3. General CCS Tips for All Cases
Always:
- Place the patient on cardiac monitor and pulse oximetry in acute/unstable situations.
- Order basic labs (CBC, BMP, LFTs, UA, pregnancy test in women of childbearing age) when appropriate.
- Address pain control and other supportive measures.
Think in phases:
- Emergency phase: Stabilize and rule out life threats.
- Diagnostic phase: Targeted testing based on working differential.
- Therapeutic phase: Definitive treatment + monitoring.
- Follow-up phase: Outpatient care, counseling, preventive care.
Don’t:
- Order every test under the sun. Unnecessary tests can hurt your score.
- Advance time too quickly without reassessing.
Practice with the official USMLE Step 3 CCS software so the interface feels familiar on exam day.
Practical Exam-Day Strategy and Neurology-Specific Mindset
1. Managing the Two Exam Days
- Day 1 (FIP):
- Focus on pacing MCQs—don’t dwell too long on any single question.
- Expect more foundational and epidemiologic questions.
- Day 2 (ACM + CCS):
- Fuel and sleep are critical; this is a long day.
- Approach MCQs with a “ward team senior” mindset: what is the safe, guideline-consistent next step?
2. Neurology Resident Advantage
As a neurology trainee:
- You likely outperform in:
- Acute neurologic presentations, imaging interpretation, ICU-level complications.
- Use this to:
- Maximize points in neuro-heavy questions and CCS cases.
- Confidently rule out dangerous neurologic conditions in general cases (e.g., when a headache is not a SAH).
The flip side: don’t let your neurology training lead you to over-order advanced tests when a simpler primary-care-level approach is appropriate.
3. Dealing with Fatigue and Stress
- During Step 3 during residency, you’ll already be fatigued:
- Schedule the exam away from night float, neuro-ICU, or heavy call blocks.
- Take full advantage of exam breaks.
- Use your resident experience:
- You’re used to making decisions under time pressure. Treat each question as a concise version of a consult.
Frequently Asked Questions (FAQ)
1. How important is Step 3 for neurology residency and the neuro match?
Step 3 is less central than Step 1 and Step 2 CK for the neurology residency match. Most programs do not require a Step 3 score at the application stage. However:
- A pass is necessary for full licensure and progression in many programs.
- A strong Step 3 score can help if you:
- Have weaker earlier scores.
- Are an IMG wanting to demonstrate testing consistency and readiness for independent practice.
- Some advanced neurology programs value applicants who have demonstrated they can pass Step 3 early, particularly if they hire residents as junior faculty or allow early moonlighting.
2. Is it better to take Step 3 before starting neurology or during residency?
For many neurology residents, late PGY-1 to end of PGY-2 is ideal. If you’re still in intern year with a strong Step 2 CK base, taking Step 3 then can work well and free your neurology years for specialty learning and board prep.
Consider:
- Your program’s policies (any deadlines? ties to promotion or licensing?).
- Your schedule (avoid ICU-heavy months).
- Your own readiness (do you feel your general medicine and pediatrics knowledge is still solid?).
3. How much time do I really need to prepare for USMLE Step 3?
For a neurology resident with decent Step 2 performance:
- Focused 4–6 weeks with 40–80 hours total of high-yield study is enough for most to pass comfortably.
- If you’ve had a long gap since medical school, struggled with earlier USMLEs, or feel weak in OB/peds/IM, lean toward 8–10 weeks of lighter but consistent study.
Your main goals are: one full pass through a high-quality QBank, and sufficient CCS practice to feel comfortable with the interface and typical case patterns.
4. How should I adapt my Step 3 preparation as a neurology resident compared with other specialties?
As a neurology resident:
- Leverage your strengths:
- You may need less time on acute neuro emergencies and more on outpatient IM, OB, and peds.
- Deliberately target weak areas:
- Block dedicated time for OB/GYN and pediatric topics, which are heavily tested and often underrepresented in neurology training.
- Use neurology cases as anchors:
- When studying general medicine, relate back to how conditions affect the nervous system (e.g., stroke in AFib, neuropathy in diabetes, seizures in eclampsia). This helps you remember content with a neuro context.
By approaching USMLE Step 3 preparation in neurology with a clear understanding of the exam, a realistic schedule around your rotations, focused resources, and a deliberate plan for CCS and non-neurology content gaps, you can turn Step 3 from a looming burden into a manageable—and even useful—step toward independent neurology practice.






















