
The average “community service” project looks impressive on a CV and changes almost nothing about health equity. You can do much better through an SNMA chapter—if you design like a researcher, execute like a QI team, and document like you are going to publish.
Let me break this down specifically.
You are not just trying to “serve the community.” You are trying to build a high‑yield health equity project: one that meaningfully targets a disparity, uses real data, fits SNMA’s mission, and is strong enough to influence residency applications, scholarship committees, and future institutional change.
(See also: How to Use AMSA to Practice Policy Advocacy Before Med School Starts for more details.)
This is absolutely doable at the premed and medical student level. But you cannot improvise it two months before application season. You need a blueprint.
Step 1: Define “High‑Yield” for a Health Equity Project
High‑yield is not a vibe. It is a set of specific characteristics.
A high‑yield SNMA health equity project usually has most of these features:
Clear disparity focus
You can state in one sentence what inequity you are targeting and for whom.- “Decrease missed postpartum follow‑up visits among Black patients.”
- “Improve HPV vaccination completion rates in Black adolescents in X ZIP codes.”
- “Increase MCAT pipeline access for URM students at local HBCUs.”
Measurable outcomes
Before–after data or at least robust process measures:- Vaccination rates, screening uptake, appointment attendance
- Knowledge scores (pre/post), number of enrolled participants who complete a program
- Applications completed, students matriculating into summer or premed bridge programs
Alignment with SNMA’s mission
The project should hit at least one core SNMA pillar:- Increasing the number of African‑American/URM physicians
- Addressing health disparities in Black communities
- Supporting the academic and professional success of Black medical students
Feasible within a student lifecycle
A project that requires 5 years of continuous work from the same leader will die. High‑yield means:- Can show early outcomes in 6–12 months
- Has built‑in continuity (underclassmen, written protocols, faculty oversight)
Scalable or replicable
Ideal SNMA projects can be:- Repeated annually with minor tweaks
- Adapted by other SNMA chapters or regional bodies
- Packaged as toolkits, posters, or how‑to guides
Evidence‑informed
Even if you cannot run an RCT, you can:- Base your intervention on existing literature and guidelines
- Use established frameworks (e.g., community health worker models, group visits, peer mentoring)
If you cannot check at least 4–5 of these boxes, you do not have a high‑yield project yet. You have an idea. The rest of this article is about turning that idea into something structurally sound.
Step 2: Anchor the Project in a Specific Health Equity Problem
Vague equity language kills projects. “Helping the underserved” is not a project definition.
You need a specific problem statement.
A. Identify a real, local disparity
Start with data and lived experience together.
Sources you can tap:
Hospital and clinic data
Work with:- Office of Health Equity / Office of Diversity & Inclusion
- Population health or quality improvement teams
- Resident QI projects you can piggyback on
Examples:
- Black patients in your safety‑net clinic have lower rates of blood pressure control than white patients.
- Black children have higher ED utilization for asthma exacerbations.
Public health data
Look at:- City/county health department dashboards
- CDC PLACES, Behavioral Risk Factor Surveillance System (BRFSS)
- Local FQHC or community health center reports
SNMA‑relevant pipeline disparities
For premed‑focused SNMA work:- Low acceptance rates from local HBCUs into your medical school
- Limited MCAT prep access for URM students within a defined region
B. Write a sharp project aim
Use a modified QI style aim:
“By [timeframe], our SNMA chapter will [increase/decrease] [specific outcome] among [defined population] at/within [setting or geographic area].”
Examples:
- “By May 2026, our SNMA chapter will increase the proportion of Black hypertensive patients with controlled blood pressure (BP <140/90) from 48% to 60% at the X Community Clinic.”
- “By March 2025, our SNMA Pipeline Initiative will increase the number of URM undergraduates at Y College who complete at least 2 full‑length MCAT practice exams from 5 to 30 students.”
That one sentence becomes the anchor. If an idea does not move that metric, it is noise.

Step 3: Build the Right Project Team Through SNMA Structure
Most student projects fail due to manpower and memory, not motivation.
Use your SNMA chapter’s structure strategically.
A. Define roles, not just titles
At minimum, assign:
Project Lead (often a chapter officer)
- Owns the timeline and deliverables
- Serves as the primary contact with faculty and community partners
Data/Outcomes Coordinator
- Designs tracking sheets, REDCap/Qualtrics forms, or simple Excel logs
- Keeps pre/post surveys standardized
- Works with any institutional data stewards if clinical data is involved
Community/School Liaison
- Coordinates with churches, schools, or clinics
- Handles scheduling and site logistics
- Keeps communication clear and respectful
Succession/Continuity Lead (usually an M1/MS1 or premed)
- Creates written SOPs (standard operating procedures)
- Ensures onboarding of next‑year volunteers
- Holds institutional memory—simple but crucial
If you are a premed chapter working under MAPS (Minority Association of Premedical Students) connected to an SNMA chapter, mirror these roles on both sides and designate clear point‑people.
B. Secure faculty and institutional backing early
High‑yield projects almost always have a faculty sponsor who:
- Co‑signs IRB applications if needed
- Helps navigate institutional politics
- Opens doors to data and community partnerships
- Stabilizes the project when student leaders graduate
Your best bets:
- Faculty involved in:
- Office of Health Equity
- Family medicine, internal medicine, pediatrics, OB/GYN with a community health focus
- SNMA faculty advisors or alumni in community‑based organizations
Approach them with:
- A one‑page concept summary
- Your specific aim statement
- A realistic ask (e.g., “We need 1 hour per month for advice and your name on an IRB application.”)
Step 4: Choose a Project Type That Fits SNMA and Your Capacity
Three project archetypes tend to be both high‑impact and realistic for SNMA chapters.
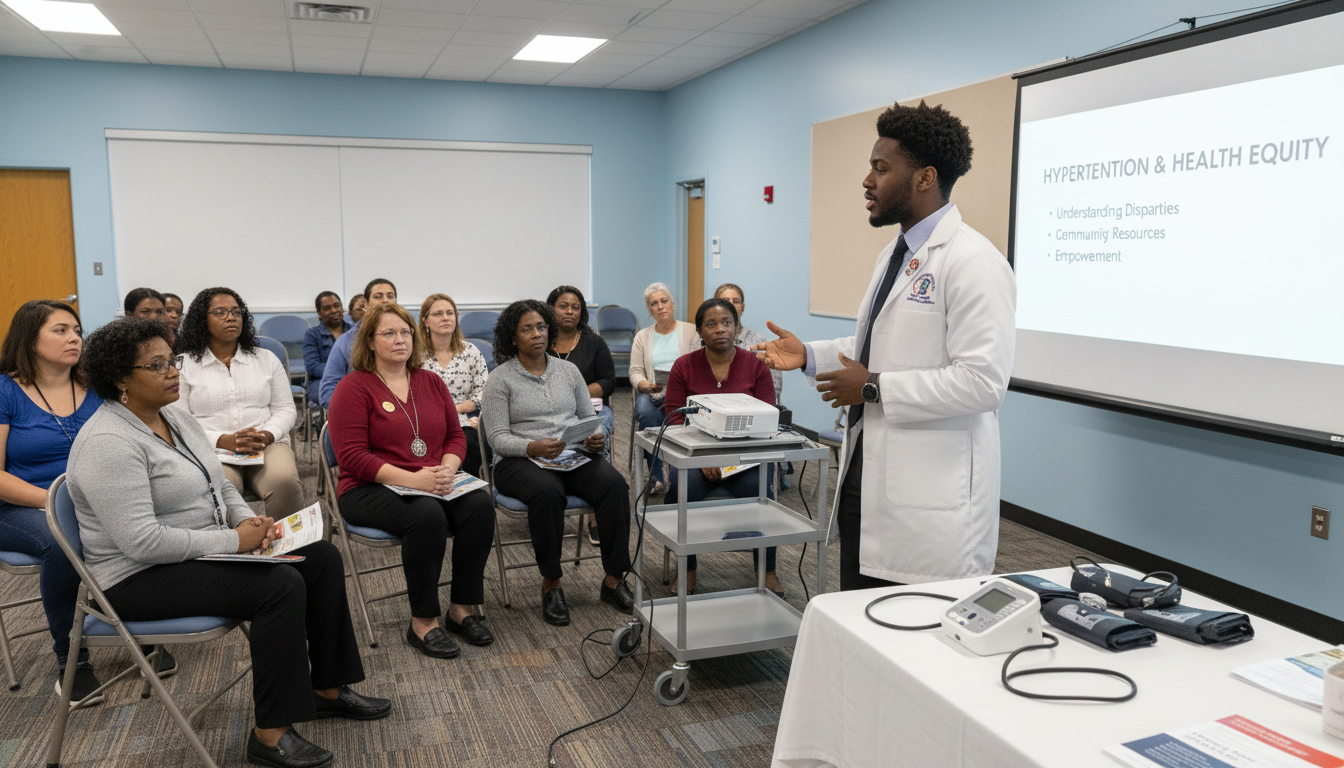
1. Community Health Education + Navigation
You are not just “teaching” but bridging access.
Examples:
- Hypertension group visits in partnership with a community clinic
- Cancer screening education plus scheduling support for mammograms or colonoscopies
- Maternal health workshops plus connection to doula services or postpartum support
High‑yield features:
- Use evidence‑based content (CDC, AHA, ACOG resources)
- Include navigation: helping people make appointments, understand insurance, access transportation
- Track:
- Attendance
- Pre/post knowledge
- Completed screenings or follow‑up visits when possible
2. Pipeline and Academic Support Interventions
Directly aligned with SNMA’s mission of increasing Black and URM physicians.
Examples:
- Structured MCAT prep cohorts for URM students at specific colleges or HBCUs
- Application bootcamps: personal statement workshops, mock interviews, financial aid sessions
- Longitudinal premed mentorship matching undergrads with SNMA members
High‑yield features:
- Cohort‑based rather than one‑off workshops
- Clear deliverables:
3. Clinic‑Embedded QI with an Equity Lens
You integrate into existing clinical workflows and push them toward equity.
Examples:
- Closing racial gaps in no‑show rates for primary care visits
- Improving diabetes education uptake among Black patients through text reminders and peer educators
- Increasing use of standardized depression screening in Black adolescents at a pediatric clinic
High‑yield features:
- Embedded in clinic’s existing QI infrastructure
- Data extraction supported by clinic staff
- Uses Plan‑Do‑Study‑Act (PDSA) cycles
For premeds, clinic‑embedded work requires stricter boundaries. But you can still:
- Do survey design, literature reviews, and material development
- Support patient education in waiting rooms with supervision
- Assist with outreach calls (if the institution permits non‑clinical volunteers)
Step 5: Design the Intervention With Rigor, Not Just Enthusiasm
This is where most student organizations lose their edge. You must design like a small QI or implementation‑science project.
A. Use a basic framework: PDSA cycles
Even if you do not call it that in your poster, internally you should think:
- Plan – Define aim, participants, setting, content, data plan
- Do – Run the intervention with a pilot group
- Study – Analyze what worked / did not work using your data
- Act – Adjust and scale or re‑design
Example: Pipeline project
Plan:
- Aim: Increase URM undergrad MCAT practice completion from 5 to 30 students.
- Design: 8‑week virtual MCAT cohort, weekly 90‑minute sessions, SNMA tutors, scheduled practice tests.
- Data: attendance, pre/post self‑rated confidence, number of participants who complete two full‑lengths.
Do:
- Recruit 20 students from one HBCU.
- Run the full cycle once.
Study:
- Only 12 students completed the course.
- Most cited time conflicts with evening labs.
- Confidence improved, but most took fewer practice exams than planned.
Act:
- Move sessions to Saturdays.
- Offer asynchronous recordings.
- Add an accountability partner system.
Run a second cohort with the new structure.
B. Clarify inclusion criteria and reach
Define who your project is for.
Example: Hypertension education project
- Adults age 18+ with documented hypertension
- Receiving care at X Community Clinic
- Self‑identified as Black/African American
- English or Spanish speaking (if you have language capacity)
Track:
This is basic implementation reporting and looks very strong in abstracts and residency applications.
C. Develop culturally grounded materials
Health equity without cultural grounding is cosmetic.
For SNMA‑led initiatives:
- Involve community partners in reviewing:
- Educational content
- Flyers and social media posts
- Survey language
- Use images and examples that reflect your target population
- For Black communities:
- Address medical mistrust explicitly and respectfully
- Highlight Black clinicians and scientists when relevant
- Incorporate church, sorority/fraternity, or barbershop/salon partnerships when appropriate
Step 6: Build a Realistic Data and Evaluation Plan
If you cannot show outcomes, your project’s yield is mostly narrative. Narrative matters, but data amplifies.
A. Choose 2–4 key measures
Think in three categories:
Reach and participation
- Demographics (age, sex, race/ethnicity if appropriate)
Short‑term outcomes
- Knowledge scores (pre/post quiz)
- Self‑efficacy or confidence scores
- Completed applications, completed MCAT practice exams
Intermediate or clinical outcomes (when feasible)
- Screening completion (e.g., mammograms done within 3 months)
- BP control, A1c changes, appointment adherence
- For pipeline projects: number of med school or post‑bac offers over a 1–2 year follow‑up
You do not need all three, but you need at least one in a rigorous way.
B. Make data collection simple enough that it actually happens
Over‑designed data plans die first.
Options:
- Paper surveys at events, later entered into Excel or REDCap
- Short QR‑code linked forms (Qualtrics, Google Forms) for pre/post evaluations
- Clinic‑provided monthly reports if embedded in QI
Key principles:
- Same questions pre and post, clearly linked
- Minimal identifiers, but enough to match pre/post when needed
- IRB consultation if you are going to publish or present outside your institution
Premeds: if you are outside an academic health system, partner with a faculty member who can advise whether IRB is needed. For internal SNMA reporting only, formal IRB is often not required, but do not guess—ask.
Step 7: Integrate Health Equity Competencies Explicitly
Many students do equity work informally but never learn the language of health equity. High‑yield projects integrate both practice and vocabulary.
Deliberately incorporate:
Structural competency
When designing and reflecting on your project, discuss:- How housing, transportation, insurance, or incarceration patterns shape the problem you are addressing
- How your intervention does or does not address structural factors
Social determinants of health (SDOH) screening or linkage
For clinic or community interventions, consider:- Standardized SDOH screener (e.g., food insecurity, housing instability)
- A clear referral pathway to social work or community resources
Anti‑racism framing
Use accurate language privately and publicly:- “Racism, not race, is the risk factor”
- “We are addressing a disparity that emerges from historic and current inequities, not from biological race.”
When you later describe your SNMA project on ERAS, secondaries, or scholarship applications, phrases like “structural competency,” “SDOH integration,” and “anti‑racist praxis” mean something specific—if you can back them up with real work.
Step 8: Formalize Sustainability and Handoff
A brilliant one‑year project that dies when the MS4 graduates is only partially high‑yield.
You want SNMA continuity baked in.
A. Write it down like someone who will graduate
Create:
One‑page project overview
- Aim statement
- Target population
- Main intervention components
- Key measures
- Community and institutional partners
Step‑by‑step SOPs
- How to schedule events or cohort sessions
- Templates for emails, flyers, social media posts
- How to access shared drives and data files
Onboarding slides
- 10–15 slides you can present at the first SNMA meeting each year
- Explain history, results so far, and where new members fit in
Store everything in:
- A shared drive (institutional OneDrive, Google Drive)
- With access controlled by SNMA officer roles, not individual student emails
B. Build a pipeline of student leadership
Integrate the project into your chapter’s internal structure:
- Make the project a standing committee (e.g., “Hypertension Equity Committee,” “Pipeline Equity Committee”).
- Elect or appoint a committee chair annually.
- Intentionally recruit:
- M1s/MS1s or early premeds as co‑leads
- At least one person per year class
Some chapters have succeeded by making their highest‑yield project the signature event or initiative of the chapter. That identity helps sustain it long after the original founder leaves.
Step 9: Translate Your Project into Academic and Career Capital
Health equity work should be impactful and visible. You want your SNMA project to speak loudly on paper.
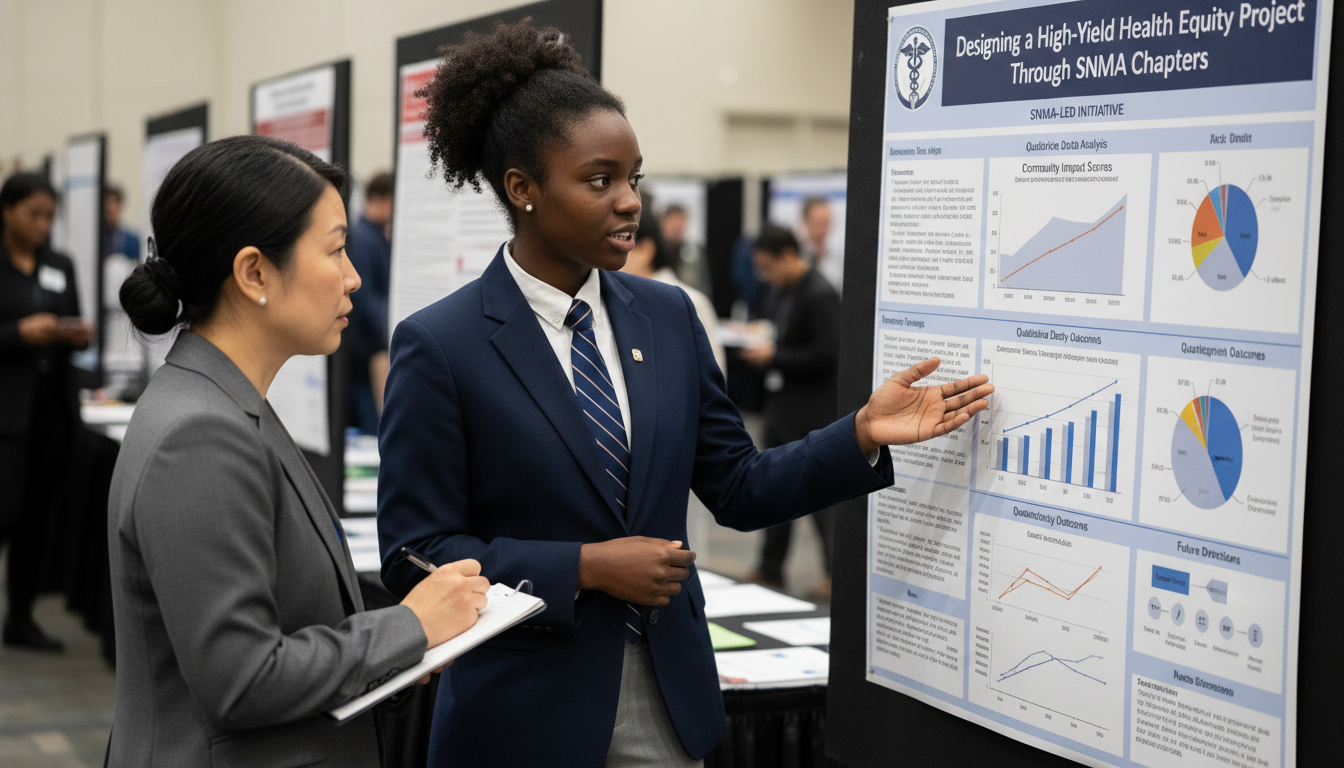
A. Manuscripts, abstracts, and posters
With a minimal data framework, you can usually generate at least one:
- Medical student research day poster
- Regional or national SNMA conference presentation
- Abstract for a specialty conference (e.g., NMA, SGIM, AAFP, APHA)
Structure your poster/manuscript more like QI:
- Background: the specific disparity, relevant data
- Methods: target population, setting, intervention, measures
- Results: key numbers, simple stats if possible
- Discussion: feasibility, challenges, equity implications, next steps
You do not need fancy statistics. Clear denominator and numerator reporting is already valuable:
- “Out of 65 eligible patients, 40 attended at least one session, and 28 completed three or more. BP control improved from 45% to 63% over 6 months among completers.”
B. Application language (premed and residency)
Do not write “Participated in community service through SNMA.”
Write:
- “Co‑led an SNMA hypertension equity project in partnership with X Community Clinic, conducting four PDSA cycles over 18 months to improve BP control among Black adults in ZIP codes 12345 and 12346. Helped increase BP control from 48% to 61% among participants (n=72), presented results at the 2026 SNMA National Conference.”
Or for a pipeline project:
- “Founded the SNMA‑MAPS MCAT Equity Cohort in collaboration with Y HBCU to address inequitable access to exam preparation resources. Over two years, recruited 46 URM undergraduates into an 8‑week structured prep program; 38 completed at least two proctored full‑length exams, and 24 matriculated into medical school, post‑bac, or SMP programs.”
This level of specificity separates you from the generic “I care about underserved communities” crowd.
Step 10: Concrete Project Models You Can Adapt Tomorrow
To make this even more actionable, here are three fully sketched project models you can adapt for your SNMA chapter.
Model 1: Hypertension Equity Through Barbershop and Clinic Partnership
Aim:
By June 2027, increase the proportion of Black male patients aged 25–65 with controlled BP from 45% to 60% at X Community Clinic, using SNMA‑supported barbershop‑based BP checks plus clinic navigation.
Design:
Partner with:
- 2–3 local Black‑owned barbershops
- One community health center
Intervention components:
Train barbers to:
- Offer BP checks with validated automated cuffs
- Provide SNMA‑developed educational cards
- Refer high readings to SNMA students present or directly to the clinic
SNMA students:
- Staff barbershops on designated days, help with BP checks, and reinforce messaging
- Schedule clinic follow‑ups on the spot via a dedicated phone line
- Track referrals and appointment completion
Measures:
- Clinic‑level BP control before vs after implementation
Model 2: SNMA‑MAPS Longitudinal MCAT Equity Cohort
Aim:
By April 2026, double the number of URM students from Y College and Z Community College who take the MCAT with at least two full‑length practice exams completed.
Design:
Cohort structure:
- 12‑week hybrid curriculum
- Weekly 2‑hour sessions (1 hr content review, 1 hr practice questions)
- Assigned SNMA mentors for each small group of 5–6 students
Supports:
- Negotiate access to discounted or donated prep materials (AAMC Fee Assistance, institutional funds, sponsorships)
- Provide test‑taking strategy workshops and application timeline overviews
Measures:
- Official MCAT attempts and scores (voluntary self‑report)
- Med school, post‑bac, or SMP matriculation within 1–2 years
Model 3: Postpartum Follow‑up Equity for Black Birthing People
Aim:
By December 2026, reduce missed 6‑week postpartum visits among Black birthing people at X Hospital from 35% to 20% using SNMA‑led patient navigation and reminder systems.
Design:
Target group:
- Black patients delivering at X Hospital
- Especially those with hypertensive disorders, diabetes, or NICU infants
Intervention components:
During inpatient stay:
- SNMA students (trained and supervised) provide brief education on warning signs, mental health, and importance of follow‑up
- Confirm preferred contact method and schedule postpartum visit before discharge
After discharge:
- SNMA students, under staff supervision, send text/phone reminders at set intervals
- Offer to help with transportation resources or childcare referrals where available
Measures:
- Postpartum visit attendance rates pre vs post implementation
- Patient‑reported satisfaction and perceived support (simple survey)
Each of these models is:
- Grounded in a clear disparity
- Payable in “student time” rather than needing massive institutional budgets
- Adaptable to many settings, both premed‑ and med‑student heavy
The Bottom Line
Three key points to keep crystal clear:
Start with a specific disparity, not with a generic volunteer idea.
Define a sharp aim, a defined population, and measurable outcomes. Everything else should serve that.Use SNMA’s structure as an engine, not just a label.
Assign concrete roles, recruit across classes, secure faculty backing, and write down your processes so the project survives turnover.Treat your project like a small QI study with equity at the center.
Plan–Do–Study–Act, collect simple but real data, anchor your language in structural and anti‑racist frameworks, and translate your work into posters, manuscripts, and compelling application narratives.
If you design your SNMA health equity initiative this way, it will not just look good on paper. It will leave something behind in the community that keeps working long after you graduate.





















