
Understanding Geographic Flexibility as a DO Graduate
Geographic flexibility is one of the most powerful—and often underused—levers you have in the residency match. For a DO graduate interested in HBCU-affiliated residency programs, it can be the difference between a highly aligned match and a disappointing outcome.
In the context of the osteopathic residency match, geographic flexibility refers to:
- How many regions or states you’re willing to train in
- Your openness to urban vs. suburban vs. rural practice environments
- Whether you’ll consider relocation far from family, social support, or current community
- Your adaptability to different hospital systems, patient populations, and state licensure climates
For DO graduates targeting schools and hospitals with historical ties to Black communities—such as programs affiliated with Meharry Medical College, Howard University, Morehouse School of Medicine, and other HBCU-linked institutions—geographic flexibility intersects with mission fit, cultural alignment, and community impact.
Because DO graduates sometimes face marginally lower interview numbers in certain competitive settings, strategically expanding your geographic preference for residency can offset those limitations. The more open and well-planned your geographic strategy, the better your odds of securing a residency that matches your clinical interests, values, and long-term goals.
This article focuses on:
- How to think strategically about geography as a DO graduate
- Where HBCU-affiliated programs are concentrated and how they differ by region
- How to balance mission alignment with personal and family needs
- Practical steps to communicate your location flexibility in the match
- Specific considerations for Meharry residency and other HBCU-affiliated pathways
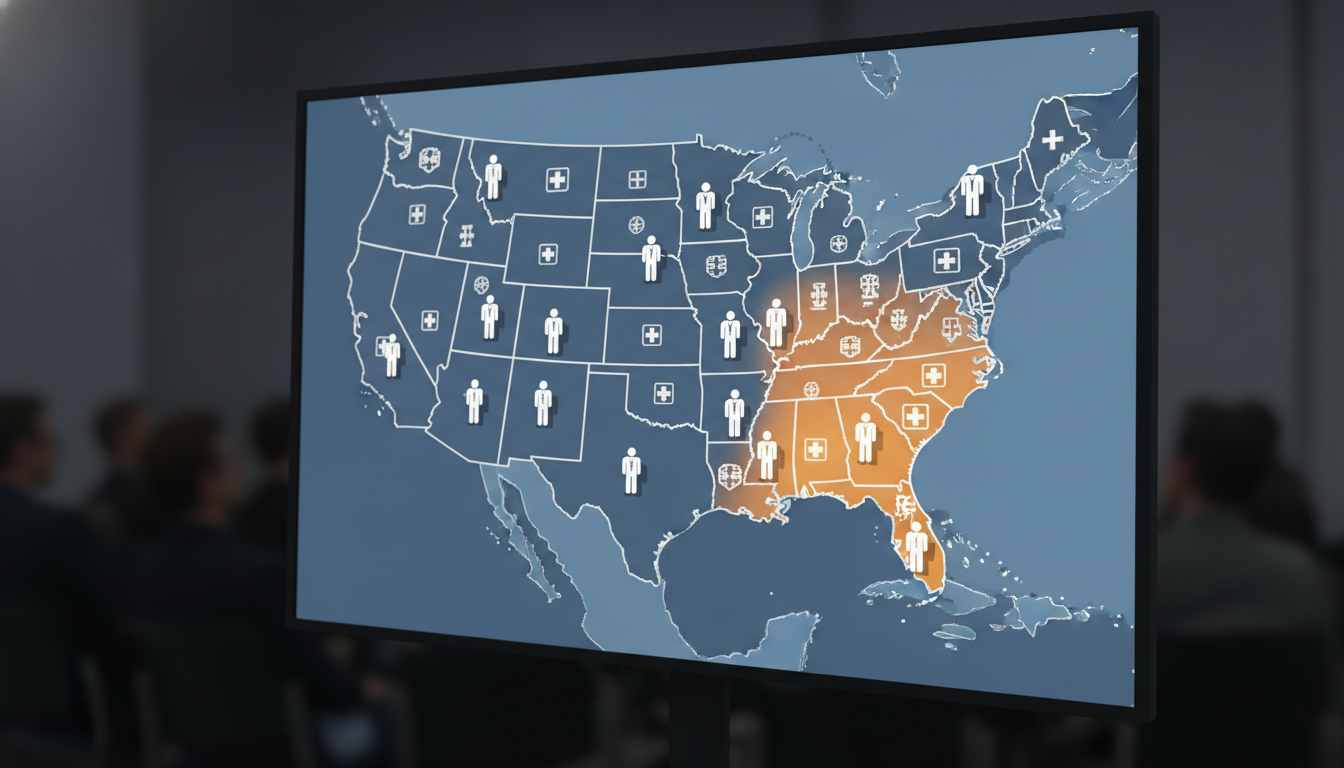
Mapping the Landscape: HBCU-Affiliated Programs and Regions
HBCU-affiliated programs are not all clustered in the same environment. Understanding their regional distribution and culture will shape your regional preference strategy.
1. Core HBCU-Affiliated Medical Schools and Teaching Hospitals
While there are many HBCUs, only a few award MD or host major GME programs directly—but numerous hospitals train residents in partnership with them or share historical ties to HBCU communities.
Key hubs include:
Meharry Medical College (Nashville, TN)
- Meharry residency programs are often community-focused, with strong emphasis on health equity, primary care, and service to underserved populations.
- Affiliations may include community hospitals, safety-net institutions, and VA systems in the Southeast region.
Howard University College of Medicine (Washington, DC)
- Howard-affiliated residencies (e.g., at Howard University Hospital and affiliated sites) serve a large urban Black population and emphasize academic medicine, advocacy, and urban health.
Morehouse School of Medicine (Atlanta, GA)
- Morehouse-affiliated GME programs, often in collaboration with regional health systems, are built around health disparities research, community engagement, and leadership in primary care and select specialties.
Other historically Black and minority-serving systems
- Some programs are not formally at an HBCU but have long-standing ties to HBCU colleges or historically Black communities (e.g., safety-net hospitals in the South and Mid-Atlantic).
- These environments often share mission overlap with HBCU residency programs even if not HBCU-labeled.
2. Typical Regional Clusters
While not exhaustive, most HBCU-related and HBCU-adjacent opportunities cluster in:
- Southeast: Tennessee, Georgia, Alabama, Louisiana, North Carolina, South Carolina, Florida
- Mid-Atlantic: Washington, DC; Maryland; Virginia
- South-Central: Texas and surrounding areas with strong Black community health networks
For a DO graduate, this means that geographic flexibility is particularly valuable if:
- You’re originally from the Midwest, West Coast, or Northeast but are open to relocating southward or to the Mid-Atlantic for training
- You did not attend an HBCU but strongly value work with underserved, predominantly Black communities
- You want a geographic preference residency that aligns with specific missions more than with proximity to your original home region
3. DO-Specific Considerations by Region
As a DO applicant, your osteopathic residency match strategy should adapt to regional realities:
- Some regions and systems have a strong history of training DOs and value osteopathic principles.
- Others are still building comfort with DO graduates, but HBCU-affiliated and safety-net institutions often prioritize mission alignment and community engagement over pedigree.
In many HBCU-related environments, a DO graduate who has demonstrated commitment to underserved communities, health disparities research, or community outreach can be highly competitive, even if their board scores are modest.
Balancing Mission, Personal Life, and Career: Defining Your Geographic Priorities
DO graduates often struggle to reconcile mission-driven goals (e.g., training at Meharry or Howard) with real-life constraints like family, finances, or partner careers. A clear framework helps you articulate what you will and will not compromise on.
1. The Three-Lens Framework
Use three lenses to define your geographic preferences:
Mission and Training Fit
- Passion for serving underserved or predominantly Black communities
- Interest in health equity, policy, or community-based research
- Desire to work with faculty and residents who share your values and background
- Alignment with osteopathic principles—whole-person care, prevention, and community wellness
Personal and Family Needs
- Partner or spouse employment and licensing
- Children’s schooling and family support systems
- Proximity to aging parents or core support networks
- Cost of living, safety, and lifestyle preferences
Career Trajectory
- Specialty goals: primary care vs. competitive specialties
- Long-term practice location (urban vs. rural; South vs. other regions)
- Desire for academic medicine vs. community practice
- Fellowship aspirations and how geographic training might shape opportunities
Write down your top 3–5 non-negotiables and 3–5 “nice-to-haves.” For example:
Non-negotiables:
- Must train in a program committed to underserved populations
- Must have at least one family/friend network or community support
- Must be a program that historically interviews or matches DO graduates
Nice-to-haves:
- Within a 6-hour drive of home
- Mild climate
- Access to a particular fellowship, research niche, or faculty mentor
2. Understanding “Geographic Flexibility” vs. “Geographic Indifference”
Being geographically flexible doesn’t mean you’re indifferent to location. It means you are:
- Clear about your priorities
- Open to multiple regions that meet those priorities, even if they aren’t “home”
- Willing to train outside your comfort zone if the program’s mission and training are strong
Example:
A DO graduate from Chicago deeply interested in Black maternal health may rank:
- Howard University Hospital (DC)
- Meharry-affiliated programs (TN)
- Morehouse-affiliated programs (GA)
- Select community-based programs in Alabama or North Carolina that serve predominantly Black communities
They’re not chasing a single city; they’re targeting a mission-focused region cluster that fits their training goals.
3. How Far Is “Too Far”?
Only you can decide this, but consider:
- Flying distance vs. driving distance for emergencies
- Cost of multiple flights per year for holidays and crises
- Emotional resilience when living without nearby family support
- The intensity of your specialty (e.g., surgery vs. psychiatry) and how much time/energy you’ll have for travel
DO graduates often benefit by being more geographically open than their MD peers, especially in competitive specialties or popular metro areas. However, if you choose to move far from support systems, intentionally build community early—especially in demanding programs with night shifts and call.
Designing a Regional Preference Strategy for the Match
A regional preference strategy is your deliberate plan for where and how widely to apply, interview, and rank programs across the map. For DO graduates targeting HBCU-affiliated or HBCU-adjacent residencies, this strategy is especially important.
1. Stepwise Regional Expansion
Consider a stepwise expansion:
Primary Target Region: HBCU-Affiliated and Mission-Aligned Sites
- Examples: Meharry residency programs in Tennessee, Howard in DC, Morehouse in Georgia, and other safety-net systems serving predominantly Black communities in the Southeast and Mid-Atlantic.
Secondary Regions with Similar Patient Populations and Values
- Larger cities with significant Black or underserved populations, even if not HBCU-affiliated (e.g., Baltimore, Philadelphia, Houston, New Orleans, Charlotte).
- Programs known for health equity, community medicine, or public hospital training.
Tertiary Regions for Match Security
- Regions where you may not have strong preferences but that:
- Have a track record of training DOs
- Offer solid clinical exposure
- Provide a reasonable lifestyle and cost of living
- These may include smaller community programs in less competitive states.
- Regions where you may not have strong preferences but that:
By structuring your application this way, you support your core goal (HBCU and mission fit) without over-constricting your options.
2. Calibrating Number of Programs by Specialty and Competitiveness
Your DO graduate residency strategy must match your specialty’s competitiveness:
- Primary Care (FM, IM, Pediatrics)
- You may be able to keep a tighter geographic focus, with ~20–35 programs, including a core HBCU or safety-net cluster plus a modest expansion region.
- Moderately Competitive Specialties (EM, OB/GYN, Psychiatry)
- Aim for broader geographic reach, often 35–50+ programs, prioritizing institutions open to DOs and aligned with your values.
- Highly Competitive Specialties (Derm, Ortho, ENT, etc.)
- Expect to apply more broadly, often 50+ programs, including many regions—then selectively highlight your interest in HBCU or equity-focused sites where applicable.
3. Strategic Use of Program Signaling and Preference Signaling (If Applicable)
If the match cycle you’re applying in includes program signaling tools:
- Use a portion of your signals for HBCU-affiliated or equity-centered programs, demonstrating clear mission alignment.
- Use some signals to build geographic credibility in your secondary target region (e.g., “I grew up in North Carolina” or “I did a sub-I in Georgia”).
Even if there’s no formal signaling system, your personal statements and geographic preference essays (where offered) can serve the same purpose.
4. Communicating Geographic Interest Without Sounding Restrictive
When asked about geography:
Emphasize flexibility:
“I’m open to training across the Southeast and Mid-Atlantic, particularly in communities that serve large Black or underserved populations.”Link location to mission:
“My priority isn’t a specific city; it’s working where I can have the most impact on health disparities, which is why I’m particularly drawn to this region and your patient population.”Avoid ultimatums:
Don’t say: “I’m only ranking programs in Nashville and DC.” Instead:
“I’ve focused my applications on regions with strong communities of color and safety-net hospitals, such as Tennessee, DC, Georgia, and neighboring states.”
Practical Steps to Demonstrate Location Flexibility and Fit
Geographic flexibility only helps you if programs believe you actually want to be there. Here’s how to prove it.
1. Use Rotations and Away Electives Strategically
If possible:
- Arrange an away rotation or audition rotation at Meharry-affiliated, Howard, or Morehouse-related sites—or at regional safety-net hospitals with similar missions.
- If you can’t rotate at those exact institutions, choose a hospital in the same region (e.g., a community program in Georgia or North Carolina) to show comfort with the region and its patient population.
On your CV and in your ERAS application, highlight:
- Clinical experiences with underserved, predominantly Black, or low-income populations
- Community outreach projects, free clinics, or public health work in similar communities
This signals to HBCU residency leadership that you are not just location-flexible, but mission-anchored.
2. Tailor Personal Statements and Supplemental Essays by Region
Where the application allows multiple personal statements or location-specific essays:
For HBCU or equity-centered programs:
- Focus on your commitment to health equity, Black community health, and structural competency.
- Mention specific reasons you’re drawn to Meharry residency or similar programs, such as their history, alumni impact, or research strengths.
For secondary and tertiary regions:
- Emphasize your adaptability and excitement to learn from diverse communities.
- Tie in any regional familiarity (family, college, past jobs, or rotations).
Avoid generic, copy-paste statements; specificity is how you communicate genuine interest.
3. Leverage Networking and Mentorship
As a DO graduate, visible support helps overcome biases:
- Connect with alumni from your osteopathic school who matched into HBCU-affiliated or southern safety-net programs.
- Ask them:
- How their programs view DO graduates
- How they framed geography and mission in their applications
- Which programs are especially DO-friendly
Attend virtual open houses and regional info sessions. Ask smart, substantive questions about:
- Community engagement and outreach
- How residents are involved in health disparities work
- Support for residents new to the region (housing, onboarding, wellness)
Programs are more likely to believe your location flexibility if they see you proactively showing up and engaging with their institution.
4. Highlight Ties and Preparedness for Relocation
In your interviews:
- Mention any real ties: extended family in the region, prior college or high school, church or community roots, or long-standing interest in the area’s history and culture.
- If you have no direct ties, emphasize thematic ties: a career-long focus on Black community health, interest in the civil rights history of the South, or prior work with similar patient populations in other states.
Example answer for “Why this region?”:
“Although I didn’t grow up in the South, most of my clinical work has focused on Black patients in under-resourced urban settings. The mission of HBCU-affiliated institutions and the Southeast’s rich Black medical history align with my goal to be a physician-advocate. I’m excited to put down roots here for residency and beyond if the opportunity arises.”

Special Considerations: Meharry, Howard, and Similar Programs for DO Graduates
Many DO graduates see Meharry residency, Howard, and Morehouse-style programs as ideal settings to live their values. To compete successfully, you’ll need to blend mission alignment with realistic expectations and geographic strategy.
1. How DO-Friendly Are These Programs?
The answer varies by specialty and year, but general trends:
Primary care and core specialties at HBCU-affiliated institutions often welcome DOs, especially when applicants:
- Have strong clinical evaluations
- Show initiative in community outreach or advocacy
- Demonstrate clear commitment to underserved populations
Some surgical and subspecialty programs may be more competitive and more MD-predominant, but DOs still match when they have:
- Strong board scores (COMLEX and/or USMLE)
- Solid letters of recommendation from known faculty
- Rotations at that institution or strong networking support
Research specific programs through FREIDA, program websites, and alumni reports to see how many DOs they’ve historically matched.
2. Making a Strong Case as a DO Applicant
For your Meharry, Howard, and similar applications:
- Emphasize how osteopathic principles align with the program’s mission:
- Whole-person care
- Prevention and lifestyle medicine
- Emphasis on social determinants of health
- Showcase experiences where you:
- Addressed barriers to care
- Worked with historically marginalized or racially minoritized patients
- Advocated for systemic change (e.g., quality-improvement projects, policy work)
Your status as a DO graduate is not a liability in these contexts if you can demonstrate:
- Clinical readiness
- Cultural humility
- Long-term commitment to service
3. Keeping Backup Geographies Without Losing Focus
Even if Meharry or Howard is your dream destination, avoid an all-or-nothing approach:
- Apply to multiple mission-aligned programs across the Southeast and Mid-Atlantic, including community programs and state university affiliates that serve similar populations.
- Use a location flexibility match mindset: you might train in North Carolina, Alabama, or Texas and still build a career deeply intertwined with Black health and equity-focused work.
Ultimately, your career impact is shaped more by your ongoing choices than by a single residency zip code. Geographic flexibility widens the door to meaningful training environments—even if they aren’t your single top-choice institution.
FAQs: Geographic Flexibility for DO Graduates in HBCU-Affiliated Programs
1. As a DO, do I hurt my chances by limiting myself to HBCU-affiliated programs only?
Yes, usually. While targeting HBCU-affiliated sites like Meharry or Howard can be a powerful strategy, overly narrow geography can reduce your overall match probability—especially in more competitive specialties. A better approach is to:
- Prioritize HBCU-affiliated programs
- Add mission-aligned safety-net and public hospitals in the same and neighboring regions
- Include a small set of broader geographic options where DOs have historically matched well
This keeps your core focus while maintaining a safety net.
2. How can I show that I’m genuinely willing to relocate to the Southeast or Mid-Atlantic?
You can demonstrate serious geographic interest by:
- Completing rotations or electives in those regions
- Participating in regional virtual open houses and info sessions
- Writing region-specific personal statements highlighting what draws you there
- Asking thoughtful interview questions about community partnerships, local health disparities, and long-term practice opportunities in the area
Programs can tell when an applicant’s interest is genuine versus perfunctory.
3. Should I mention personal geographic limitations (e.g., caring for a family member) during interviews?
Yes—but thoughtfully and professionally. If there are true constraints (such as a co-parenting agreement or caregiving responsibility), be honest without sounding rigid or negative. For example:
“I’m the primary caregiver for a family member in [Region X], so I’ve focused my applications in this broader area. Within this region, I’m very flexible and excited about diverse training environments, especially those serving underserved communities.”
Programs appreciate clarity and advanced planning more than vague hints.
4. If I don’t match at an HBCU-affiliated program, can I still build a career in Black community health?
Absolutely. Training at an HBCU-affiliated site is a powerful path, but not the only one. You can:
- Choose residencies at safety-net or public hospitals with large Black patient populations
- Focus your QI, research, and advocacy projects on Black community health
- Join national organizations and interest groups dedicated to health equity and racial justice
- Later, pursue fellowships or faculty roles at Meharry, Howard, Morehouse, or similar institutions
Your geographic flexibility in residency can be a stepping-stone, not a detour, on the path to long-term impact.
Geographic flexibility, when guided by clear values and realistic strategy, allows DO graduates to access a wide range of HBCU-affiliated and mission-aligned residency opportunities. By understanding the regional landscape, articulating your priorities, and demonstrating both adaptability and authenticity, you can position yourself for a residency experience that advances both your career and the communities you’re called to serve.






















