
Choosing where to apply in internal medicine residency can feel overwhelming. There are hundreds of programs, each with different cultures, strengths, and expectations. A thoughtful, structured program research strategy can transform this from a stressor into a strategic advantage for your IM match.
Below is a comprehensive, step‑by‑step guide on how to research residency programs in internal medicine—what to look for, where to find information, and how to interpret what you see.
Understanding Your Priorities Before You Start Researching
Before diving into databases and websites, clarify what you want. You can’t meaningfully evaluate residency programs if you don’t know your own priorities.
1. Clinical Training and Case Mix
For internal medicine residency, think specifically about:
- Breadth vs. depth of exposure
- Do you want high-volume tertiary/quaternary care (e.g., transplant, LVAD, advanced oncology)?
- Or a more generalist, community-focused experience?
- Inpatient vs. outpatient balance
- Are you aiming for hospitalist work, primary care, or subspecialty training?
- Look for clinics per week, continuity clinic structure, ambulatory blocks.
- ICU and procedural exposure
- How much time do residents spend in MICU/CCU?
- Are residents the primary operators for procedures (paracentesis, thoracentesis, LP, central lines), or are these mostly done by procedure teams?
Clarify your ideal training environment:
- “I need strong ICU training; I want to be a comfortable hospitalist anywhere.”
- “I want robust outpatient training; I’m primary-care oriented.”
- “I want complex tertiary/quaternary care for fellowship preparation.”
2. Fellowship and Career Goals
List your top 1–3 possible paths:
- Subspecialty fellowship (e.g., cardiology, GI, heme/onc, pulm/crit, nephrology, ID, rheum, endo)
- Hospitalist medicine
- Primary care / ambulatory IM
- Clinical educator, QI/leadership, or clinician-scientist roles
This directly shapes how you evaluate programs:
- Fellowship-aimed applicants may prioritize:
- Program’s fellowship match list
- Research opportunities and mentorship
- Reputation and network in desired subspecialty
- Hospitalist-/primary-care–aimed applicants may prioritize:
- Autonomy in inpatient management
- Strong ambulatory curriculum
- Community exposure and transition-of-care experiences
3. Geography and Lifestyle
Be honest with yourself about:
- Region: Northeast vs. Midwest vs. South vs. West; urban vs. suburban vs. rural
- Support system: Proximity to family/partner/friends
- Cost of living: How far your salary will stretch, especially in high-cost cities
- Commute & housing: Parking, safety, public transportation
Decide:
- Regions you must consider
- Regions you’re open to
- Regions you will not consider
4. Program Culture and Learning Environment
Culture is harder to quantify, but crucial. Reflect on:
- Do you prefer a high-intensity, academic environment or a more relaxed, community feel?
- How important is resident camaraderie and wellness initiatives to you?
- Are you comfortable in a hierarchical environment, or do you prefer flatter structures with more informality between residents and faculty?
Write down 5–7 non‑negotiable or high-priority features, such as:
- “Supportive environment, not malignant”
- “Strong mentorship and career guidance”
- “Active diversity, equity, and inclusion initiatives”
- “Safe neighborhoods and reasonable commute”
These will anchor your program research strategy.
Where to Find Information on Internal Medicine Residency Programs
Once your priorities are clear, use multiple information sources. Each has strengths and limitations; triangulating across them improves accuracy.

1. Official Databases and Directories
FREIDA (AMA Residency & Fellowship Database)
FREIDA is one of the most comprehensive tools for how to research residency programs:
- Shows:
- Program size (number of residents per year)
- Program type (university, community, university-affiliated)
- Visa sponsorship details
- Work hours, call structure (self-reported)
- Benefits and salary (approximate)
- Use filters for:
- Location (state, region)
- Program type
- IMGs, DO-friendliness (if indicated)
- Research opportunities
Action step: Export or manually record FREIDA data into a spreadsheet with columns such as:
- Program name
- City, state
- Program type (university, community, hybrid)
- Residents per class
- Research track (Y/N)
- Fellowship programs on-site (Y/N)
- Visa (if applicable)
- Notes/initial impressions
ERAS / NRMP Data & Program Lists
- ERAS will list programs to which you can apply.
- NRMP “Charting Outcomes” and program characteristics reports help you:
- Calibrate competitiveness
- Understand average Step scores, publications, etc. (by specialty, not by individual program)
- See IM match trends (e.g., number of positions, fill rates, USMD/DO/IMG distributions)
Use these to create a realistic range of:
- “Reach” programs
- “Target” programs
- “Safety” programs
2. Program Websites
Program websites are crucial for evaluating residency programs, though sometimes outdated. Focus on key sections:
a. Curriculum and Rotations
Look for:
- Rotation schedule by PGY year
- Ward months vs. ICU vs. electives vs. ambulatory blocks
- Night float vs. 24-hour call
- Continuity clinic structure
- ½ day weekly vs. longer blocks
- Patient population and preceptor consistency
Ask:
- Does the schedule align with how you want to train?
- Is there a clear progression of autonomy across PGY1–3?
b. Faculty and Leadership
Check:
- Program Director (PD) and Associate PD bios
- Core faculty and their interests (clinical, teaching, research)
- Subspecialty representation—especially relevant if you have a fellowship in mind
Signs of strength:
- Multiple faculty with educational leadership roles
- Faculty with clear mentoring and scholarly interests aligned with your goals
c. Research & Scholarly Opportunities
For fellowship-aimed applicants, look for:
- Research infrastructure
- Dedicated research tracks or pathways
- Protected research time (if any)
- On-site clinical trials, QI projects, health services research
- Productivity indicators
- Resident publications and presentations listed
- Support for conference travel (ACP, ATS, AHA, ASH, etc.)
d. Fellowships at the Institution
Check if the institution offers:
- On-site IM subspecialty fellowships (cardiology, GI, heme/onc, etc.)
- Combined or research-oriented pathways
Programs with robust fellowships can offer:
- More subspecialty electives
- Strong mentors
- Internal pipeline for fellowship applicants
But note: absence of on-site fellowships doesn’t preclude strong fellowship outcomes, especially at some community or hybrid programs.
3. Program Social Media and Virtual Content
Twitter/X, Instagram, and YouTube can give insights into program culture and day-to-day life:
- Look for:
- Resident takeovers and “day in the life” content
- Photos of conferences, retreats, wellness events
- Recognition of resident achievements (awards, publications)
- YouTube:
- Virtual tours of hospital and clinics
- Program overview videos
- Chief resident introductions
Ask:
- Do residents seem collegial and happy?
- Does the program celebrate teaching and scholarship?
4. Word of Mouth: Advisors, Residents, and Alumni
Your Home Institution
- Talk to:
- IM clerkship director
- Internal medicine advisors
- Subspecialists in your area of interest
- Ask:
- “Which programs do you think are a good fit for my goals?”
- “Where have recent grads with similar profiles matched?”
Current Residents and Recent Graduates
If possible, reach out (politely) to:
- Alumni from your school currently in IM residency
- Residents you met on rotations, conferences, or through mentors
Ask concrete questions:
- “What surprised you most about your program (positively and negatively)?”
- “How is the balance between autonomy and supervision?”
- “How approachable are attendings and leadership?”
- “How is the program responding to resident feedback?”
5. Independent Review Platforms and Forums (Use With Caution)
Websites and forums may include:
- Program reviews
- Anecdotal reports of culture, workload, or PD changes
Use them as:
- Signal detectors: identify potential red flags that you can later confirm via official channels or resident conversations
- Not as definitive truth—bias and outdated information are common
How to Systematically Compare Internal Medicine Residency Programs
Information is only useful if you organize and interpret it. Create a system that allows you to consistently evaluate programs side by side.
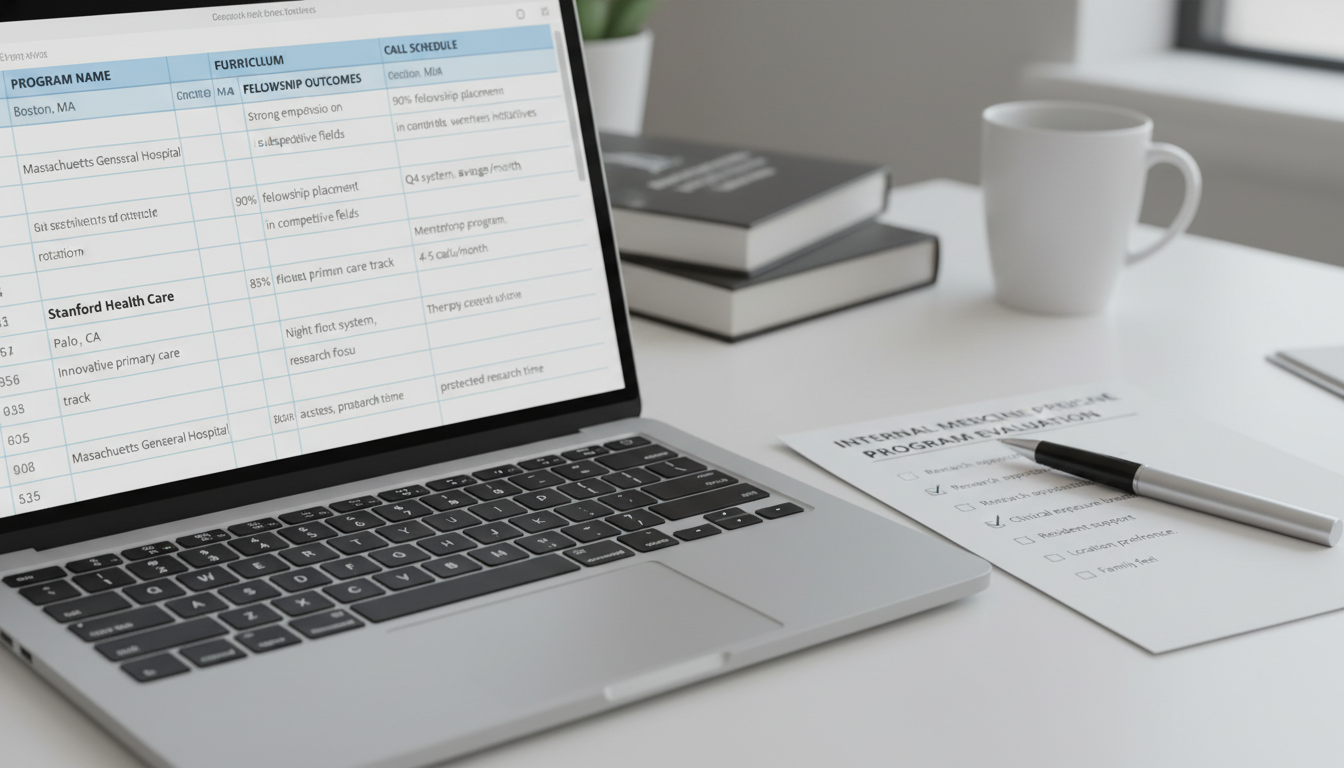
Step 1: Build a Master Spreadsheet
Set up columns for:
Program Basics
- Program name
- City, state, region
- Program type (university, community, hybrid)
- Program size (residents per class)
Training Environment
- Primary hospital type (county, VA, private, academic center)
- ICU months and structure
- Night float vs. 24-hr call
- Average duty hours and day-off policies (as reported)
- Outpatient / ambulatory structure
Academic & Career Outcomes
- On-site IM fellowships (Y/N; which ones)
- Recent fellowship match list (if available)
- Research opportunities (Y/N; structured track?)
- Conference support
Culture and Support
- Wellness initiatives (formal)
- DEI and inclusion efforts
- Perceived resident camaraderie (your impression from socials/conversations)
- Leadership responsiveness (comments from residents)
Logistics
- Cost of living (estimate: high/medium/low)
- Salary & benefits (rough comparison)
- Visa sponsorship (if applicable)
- Proximity to support system
Also include:
- Categorization: Reach / Target / Safety
- Overall fit score (1–5 or 1–10, subjective)
- Notes: Quick reactions or comments (e.g., “Loved PD video,” “Weak ambulatory info,” “Strong cardiology reputation”)
Step 2: Define Your “Fit Criteria” and Weight Them
Not all factors matter equally for everyone. Assign relative importance:
Example weighting:
- Clinical training & case mix: 30%
- Fellowship outcomes & research: 25%
- Culture and resident satisfaction: 25%
- Geography & lifestyle: 15%
- Salary/benefits: 5%
Then, for each program, rate it (e.g., 1–5) on each category and compute a weighted “fit score.” This doesn’t have to be perfectly precise—it’s a tool to clarify your thinking.
Step 3: Create Shortlists by Tiers
Using your spreadsheet and scores:
- Initial long list: 60–100+ programs, depending on your competitiveness and applicant category (USMD vs DO vs IMG).
- Refined list: Remove clear mismatches (wrong geography, visa limitations, no fellowship focus if you need that, etc.).
- Tiered list:
- Tier 1: Top-choice programs (where you’d be thrilled to match)
- Tier 2: Strong fits (where you’d be happy to train)
- Tier 3: Backup programs (where you can get solid training but perhaps with some trade-offs)
Be realistic: ensure you have enough programs in each tier, especially target and safety tiers, to maximize your IM match chances.
Key Factors to Evaluate in Internal Medicine Residency Programs
When performing deeper dives on each program, systematically evaluate these domains.
1. Clinical Training Quality
Look for:
- Inpatient Training
- Who admits and follows patients—residents vs hospitalists vs private attendings?
- Daily team census and caps
- Intern vs senior responsibilities
- ICU Experience
- Open vs closed ICU
- Resident autonomy in critical care decisions and procedures
- Supervision by intensivists and fellows
- Procedural Training
- Are residents performing IM-relevant procedures?
- Is there a procedure service residents can join?
Signs of strong training:
- Residents clearly articulate robust experience with bread-and-butter and complex cases.
- Graduates feel “ready to be a hospitalist” or “prepared for fellowship” by end of PGY-3.
2. Ambulatory and Primary Care Experience
Even if you plan on fellowship, ambulatory IM is foundational:
- Continuity clinic:
- Number of sessions per week
- Panel size and responsibility
- Ambulatory rotations:
- Exposure to common outpatient issues (diabetes, hypertension, chronic pain, mental health)
- Integrated behavioral health, social work, pharmacists
If primary care is your interest, look for:
- Dedicated primary care or ambulatory tracks
- Community-based clinics
- Faculty with general internal medicine focus
3. Fellowship Match and Career Outcomes
For evaluating residency programs on fellowship strength, ask:
- Does the website provide a recent fellowship match list?
- Where do graduates match?
- In which subspecialties?
- Are there:
- Subspecialty-specific mentorship structures?
- Regular “fellowship application prep” sessions?
Don’t overinterpret single-year anomalies; look at patterns over several years if available.
4. Academic Environment and Teaching
Indicators of strong teaching culture:
- Daily or near-daily conferences (morning report, noon conference)
- Bedside teaching during rounds
- Protected educational time (and actual adherence to it)
- Faculty recognized for teaching (awards, roles as clerkship directors, etc.)
Ask current residents (during interview season):
- “Do you feel like teaching is protected, or does it get overshadowed by workflow?”
- “How often do attendings teach at the bedside?”
5. Program Culture and Wellness
Culture is often what makes or breaks residency satisfaction.
Look for:
- Evidence of resident advocacy:
- Changes made in response to resident feedback (e.g., improved night coverage, added wellness days)
- Wellness initiatives:
- Formal wellness curriculum
- Access to mental health services
- Retreats, social events, mentorship programs
- Diversity and inclusion:
- Representation among residents and faculty
- DEI committees and initiatives
- Support for underrepresented groups
During interviews or informal calls, ask:
- “How does the program support residents during difficult rotations?”
- “Can you tell me about a time resident feedback led to a real change?”
6. Workload, Schedule, and Logistics
Training is demanding everywhere, but there are differences in:
- Call schedules and night float
- Number of days off per month
- Cross-coverage and ancillary staff support
- EMR system and efficiency tools
Also pay attention to:
- Parking availability and cost
- Hospital location vs. typical housing options
- Commute times and safety considerations
A Step-by-Step Program Research Strategy Timeline
To make this actionable, here’s a suggested timeline for researching internal medicine residency programs.
6–9 Months Before ERAS Submission
Self-assessment and priority setting
- Clarify goals (fellowship vs hospitalist vs primary care).
- Identify geographic and lifestyle constraints.
Macro-level research
- Use FREIDA and NRMP data to understand the IM landscape.
- Build your initial long list of programs.
4–6 Months Before ERAS Submission
Deep dive into program websites
- Fill in your spreadsheet with key information.
- Start excluding clear non-fits (e.g., wrong region, major deal-breakers).
Seek guidance
- Meet with an internal medicine advisor.
- Show your spreadsheet and get feedback on reach/target/safety balance.
2–4 Months Before ERAS Submission
Refine shortlist
- Narrow to a realistic application list based on competitiveness and budget.
- Group programs into tiers.
Begin networking (appropriately)
- Attend virtual open houses.
- Engage with program social media (follow, attend live Q&As if offered).
During Interview Season
Update data with real impressions
- For each interview, take structured notes immediately afterward:
- Culture, resident happiness
- PD and APD accessibility
- How well the program addressed your priority areas
- Adjust your initial fit scores based on what you learn.
- For each interview, take structured notes immediately afterward:
Prepare for rank list
- After interviews, re-rank programs based on:
- Training quality
- Culture
- Career alignment
- Personal life considerations
- After interviews, re-rank programs based on:
This structured approach ensures your IM match list reflects both objective research and subjective fit.
Frequently Asked Questions (FAQ)
1. How many internal medicine residency programs should I research and apply to?
The number depends on your competitiveness, USMD/DO/IMG status, and geographic flexibility.
- Research phase: It’s reasonable to preliminarily review 60–100+ programs.
- Application phase:
- Highly competitive USMDs may apply to ~20–30 IM programs.
- Many USMD/DO applicants apply to ~30–40.
- Many IMGs and more at-risk applicants may apply to 60+.
Use your advisor’s input and NRMP “Charting Outcomes” to calibrate. Better to over-research early and then strategically narrow than scramble late.
2. How do I evaluate program reputation for internal medicine?
For internal medicine residency, reputation is multi-dimensional:
- Regional reputation: Often more influential for job/fellowship prospects than national name alone.
- Fellowship matches: Where do graduates go, especially in your desired subspecialty?
- Academic output: Are residents publishing and presenting?
Ask mentors:
- “How is this program viewed within the internal medicine community?”
- “Would training here support my goal of [specific fellowship or career]?”
Avoid relying solely on informal “rank lists” or hearsay; they’re often biased and outdated.
3. I’m interested in fellowship—should I only apply to big academic centers?
Not necessarily. Many excellent fellows come from community or hybrid programs. Consider:
- Academic centers:
- Pros: More subspecialty exposure, research, internal fellowships.
- Cons: Sometimes less autonomy, more competition for research mentors.
- Community/hybrid programs:
- Pros: High autonomy, strong clinical training, often excellent hospitalist preparation.
- Cons: May require more initiative to find research/fellowship mentors (though many have formal structures now).
Focus on:
- Demonstrated fellowship match success
- Availability of mentorship and scholarly projects
- Clear, supportive advising for fellowship applications.
4. How can I assess program culture before interview day?
You can get early clues by:
- Reviewing social media:
- Are residents frequently highlighted?
- Do posts reflect camaraderie and inclusion?
- Attending open houses:
- Listen to how residents talk about each other and leadership.
- Look for consistency across speakers.
- Talking to alumni or current residents (if you have connections):
- Ask open-ended questions about support, burnout, and how the program handles conflicts or feedback.
Ultimately, program culture becomes clearest during interviews and post-interview reflection, but early research can help you prioritize programs more likely to fit your values.
By approaching how to research residency programs in internal medicine with a structured, intentional strategy, you greatly increase the odds that your IM match will place you in a setting where you’ll thrive—clinically, academically, and personally. Use data, mentorship, and your own values in equal measure, and let your research guide you to programs where you can become the internist you aspire to be.






















