
Understanding the Big Picture: Why Program Research Matters in Ortho
Orthopedic surgery is among the most competitive specialties in the allopathic medical school match. As an MD graduate, your odds of a successful ortho match are influenced not only by your board scores, research, and letters, but also by how strategically you research and select programs.
Many strong applicants fail to match because they:
- Aim only at “name-brand” programs they don’t realistically fit
- Apply too broadly and shallowly without clear priorities
- Don’t understand how to evaluate orthopedic surgery residency programs beyond prestige
- Cannot articulate why they’re a good fit for a given program when writing personal statements or interviewing
Thorough program research helps you to:
- Build a balanced program list (reach/target/safety)
- Identify environments where you’ll thrive and grow, not just survive
- Tailor your application to demonstrate fit with each program
- Avoid unpleasant surprises after Match Day (case volume, culture, location, or fellowship exposure that don’t match your career goals)
This article will walk you through a step-by-step program research strategy specifically tailored for orthopedic surgery residency and MD graduates. You’ll learn how to research residency programs efficiently, what metrics and factors actually matter, and how to synthesize the data into a clear, actionable plan.
Step 1: Define Your Priorities as an MD Graduate in Orthopedic Surgery
Before you even open a program website, you need clarity on what you want. Without this, evaluating residency programs becomes a flood of unorganized information.
A. Clarify Your Professional Goals
Ask yourself:
What type of orthopedist do I think I want to be?
- Undecided (most applicants)
- General orthopedics
- Sports medicine
- Hand and upper extremity
- Spine
- Trauma
- Adult reconstruction (joints)
- Pediatric orthopedics
- Foot and ankle
- Orthopedic oncology
Academic vs. community practice orientation
- Do you see yourself at a university/academic center, doing research, teaching residents?
- Or a community practice with higher clinical volume and less research?
- Or a hybrid model?
Fellowship vs. generalist
- Almost all modern orthopedists complete a fellowship, but:
- Are you set on highly competitive fellowships (e.g., sports at big-name institutions)?
- Do you want a program with a strong track record of matching into your preferred subspecialty?
- Almost all modern orthopedists complete a fellowship, but:
Your answers here drive how you interpret program data later, especially case volume, research infrastructure, and fellowship match outcomes.
B. Identify Personal and Lifestyle Priorities
You will spend five demanding years in this program. Consider:
Geographic constraints
- Must be near family or partner?
- Can’t tolerate extreme cold/heat?
- Preference for urban vs. suburban vs. mid-sized city?
Work-life balance realities
- Orthopedic surgery is demanding everywhere, but:
- Some programs have unrelenting trauma call, others more balanced rotations.
- Some cultures are more supportive, others more “sink or swim.”
- Orthopedic surgery is demanding everywhere, but:
Support system
- Are you moving with a partner who needs a job?
- Childcare or schooling requirements?
- Immigration/visa considerations (if applicable)?
C. Self-Assessment of Competitiveness
An honest assessment protects you from building an unrealistic list.
Key elements:
- USMLE/COMLEX scores (or equivalent)
- Medical school reputation and resources
- Ortho-specific letters of recommendation (including from orthopedic faculty or chair)
- Research productivity in orthopedics or related fields
- Away rotation performance and evaluations
- Red flags: leaves of absence, professionalism issues, exam failures
Rough orientation (not rigid cutoffs):
- Highly competitive profile
- Above-average scores for ortho, strong ortho research, multiple ortho letters, home ortho program, strong clinical performance.
- Moderately competitive profile
- Solid scores, at least one ortho letter, some research or good clinical performance, maybe no home ortho program.
- At-risk or less competitive profile
- Below-average scores, limited ortho exposure or research, or significant red flags.
Your “tier” will affect how broad your list must be and how heavily you rely on “safety” or less competitive programs, including newer or smaller ones.
Step 2: Build a Master List and Organize Your Research
Now that you know your goals and constraints, you can start assembling a master list of potential programs to investigate.
A. Gathering an Initial List of Orthopedic Programs
Use multiple sources:
ERAS / AAMC / FREIDA Online
- Filter by “Orthopaedic Surgery” and set location filters.
- Note program type (university, community, university-affiliated).
NRMP Charting Outcomes and Program Director Surveys
- Understand average metrics for matched applicants.
- See what program directors value (research, letters, grades, etc.).
AAOS and specialty society resources
- Sometimes list residency programs and fellowships, with links to academic departments.
Your medical school advising office
- Ask for historical match lists for your institution.
- Request feedback from ortho faculty on programs where your graduates have done well.
Word-of-mouth from recent graduates and residents
- Ask graduates who matched orthopedic surgery about where they applied and why.
Aim for an overinclusive master list initially; you will narrow it after deeper research.
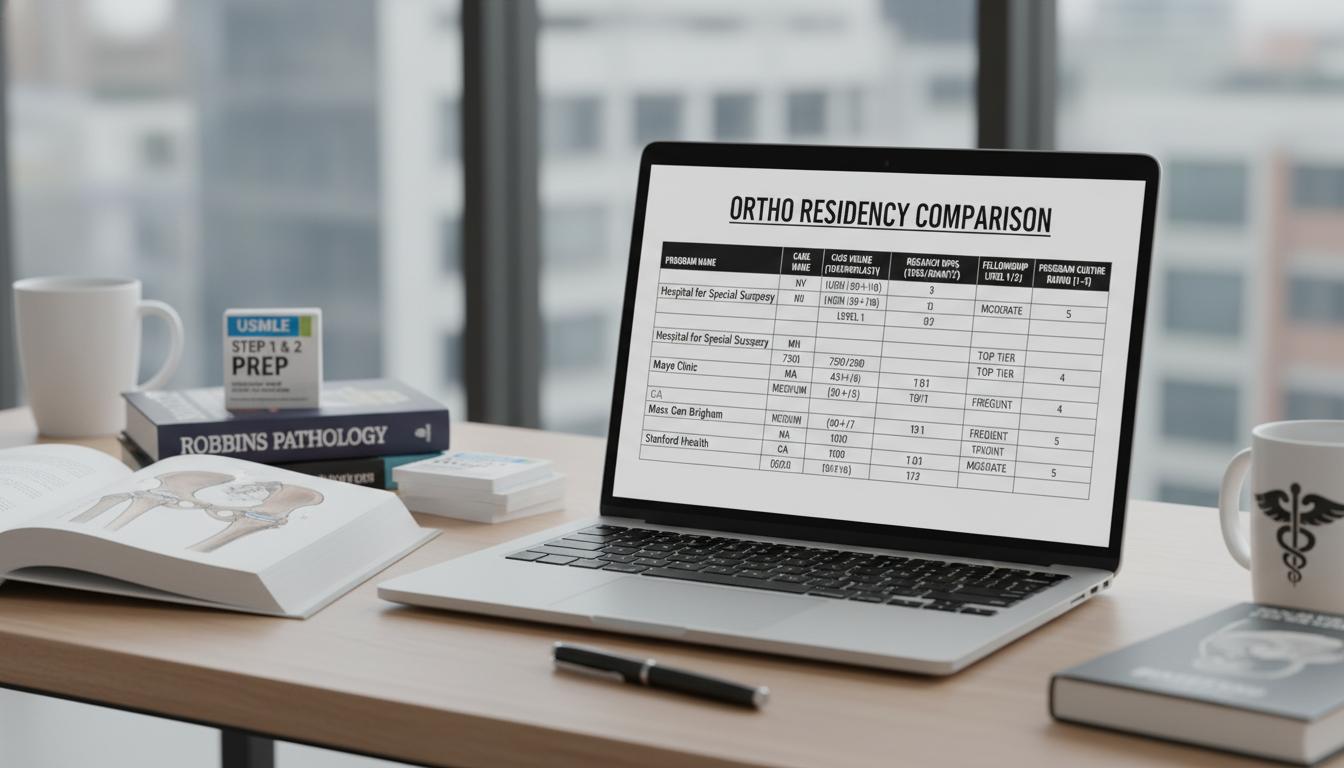
B. Create a Program Research Spreadsheet
To make your program research strategy efficient, build a simple but structured spreadsheet or database. Include columns for:
- Program name and ACGME code
- Location (city, state, region)
- Program type: academic, community, hybrid
- Number of residents per year
- USMLE/COMLEX expectations (if disclosed)
- Presence of a home ortho fellowship programs (sports, joints, trauma, etc.)
- Approximate case volume per resident
- Level 1 trauma center vs. other designations
- Pediatric ortho exposure (in-house vs. external rotation)
- Research infrastructure:
- Mandatory research time?
- Research requirement to graduate?
- Dedicated research staff/statisticians?
- Recent fellowship match outcomes
- Program culture notes:
- Resident camaraderie
- Operative autonomy
- Call schedule and work hours
- Diversity and inclusion environment
- Housing cost and cost of living
- Visa sponsorship (if needed)
- Gut impression / “fit” rating (1–5)
- Category: Reach / Target / Safety
This framework turns a vague question—how to research residency programs—into a structured, comparable dataset you can analyze.
Step 3: Deep Dive into Program Information Sources
Once you have your master list, the next step in evaluating residency programs is to gather high-yield, accurate information from multiple sources.
A. Official Program Websites: Read Between the Lines
Program websites are your starting point, but you must interpret them critically.
Key sections to review:
Curriculum and rotation schedule
- How are the 5 years structured?
- Distribution of:
- Trauma
- Joints
- Sports
- Hand
- Spine
- Pediatrics
- Foot & ankle
- Oncology
- Are there outside rotations? Where and how long?
Operative experience
- Any published case numbers per resident?
- Examples:
- “Our graduates average >2,300 primary cases.”
- “High volume in level 1 trauma.”
- Red flags:
- Very vague language like “broad exposure” without numbers.
- Heavy service obligations without clear operative milestones.
Resident roster and alumni outcomes
- Current residents: educational background, diversity, prior research.
- Graduates: Where did they go for fellowship? What subspecialties?
- Look for alignment with your goals:
- If you want sports medicine, do many grads match into top sports fellowships?
Research expectations and opportunities
- Is there protected research time?
- Are residents expected to publish annually?
- Is there an orthopaedic research lab, outcomes center, biomechanics lab, or similar?
Program leadership and faculty
- Program director and chair backgrounds.
- Faculty with national reputations or leadership roles in subspecialty associations.
- Any notable research interests aligned with yours.
Diversity, wellness, and culture statements
- Look for concrete initiatives, not only generic language.
- Are there mentorship programs, wellness days, or resident support resources?
Take structured notes into your spreadsheet, focusing on differences between programs.
B. Databases and Independent Resources
Beyond websites:
FREIDA, Doximity Residency Navigator, AMA resources
- Data on program size, location, and sometimes resident satisfaction.
- Doximity rankings should be one small piece of the puzzle, not your primary filter.
Program-specific social media (Instagram, X/Twitter, YouTube)
- Informal look at:
- Resident camaraderie
- Operative experiences (within HIPAA limits)
- Retreats and social events
- See how they present resident life and accomplishments.
- Informal look at:
Virtual open houses and information sessions
- Many orthopedic programs host these pre-interview.
- Ask practical questions about:
- Call
- Operative autonomy
- Evaluation system
- Take live notes in your spreadsheet.
Resident and alumni perspectives
- If appropriate, contact:
- Graduates of your medical school at that program
- Residents you met at conferences or on away rotations
- Ask specific, respectful questions:
- “What surprised you most when you started?”
- “Do residents feel supported when they struggle?”
- “How is feedback delivered?”
- If appropriate, contact:
C. Clarify What’s Realistic: Step Scores and Filter Culture
Many MD graduate residency applicants worry about hidden “cutoffs.” For orthopedic surgery:
- Some programs disclose minimum USMLE Step 1/2 scores on FREIDA or their websites.
- If not disclosed, use:
- NRMP Charting Outcomes
- Word of mouth from advisors and recent applicants
You’re trying to understand:
- Which programs are very unlikely to consider your application given your metrics.
- Which programs are friendly to late bloomers or non-traditional trajectories.
This helps you fine-tune your reach/target/safety distribution.
Step 4: Key Factors to Evaluate in Orthopedic Surgery Programs
Now let’s talk about how to evaluate residency programs in a way that’s specific and actionable for orthopedic surgery.
A. Operative Volume and Case Mix
You are training to be a surgeon; operative experience is central.
Ask:
- What is the total case volume per resident by graduation?
- Is the case mix balanced?
- Trauma
- Elective arthroplasty
- Sports procedures (arthroscopy)
- Hand and microvascular exposure
- Spine
- Pediatrics
Evaluate alignment with your goals:
- If you want to be a community generalist, a very high-volume, broad case mix may be ideal.
- If you’re focused on highly specialized academic careers, a program with strong subspecialty depth and fellowship-placement track record matters more.
Be cautious of:
- Programs boasting huge service responsibilities but not clear operative autonomy.
- Excessive outside rotations where residents are “assistants” more than primary operators.
B. Autonomy and Graduated Responsibility
Numbers alone don’t capture what you are actually doing in the OR.
Look for signals:
- Do senior residents function as primary surgeons on complex cases?
- Are there fellows in every subspecialty who may compete for cases?
- Do residents speak (publicly or privately) about feeling well-prepared for fellowship and independent practice?
A good pattern:
- Junior years: fundamental fracture fixation, basic arthroscopy, straightforward cases.
- Senior years: complex trauma, revisions, advanced arthroscopy, leadership in OR.
C. Trauma Exposure and Call
Most orthopedic residents develop strong trauma skills; still, there’s wide variation:
- Level 1 trauma center vs. Level 2 or community setting
- Frequency and structure of call:
- In-house vs. home call
- Night float vs. traditional Q4–Q6 call
- How much of your early training is trauma-heavy vs. balanced?
Match this with your preferences:
- Love high-acuity trauma and late-night operating? High-trauma centers with robust call may be attractive.
- Prefer a more elective, outpatient future? You may still want strong trauma training, but you might not want a program that is dominated by trauma year-round.
D. Research Environment and Academic Expectations
For the allopathic medical school match, academic metrics often matter more at research-intensive programs.
Assess:
- Is dedicated research time built into the curriculum?
- Are there:
- NIH-funded investigators?
- Basic science labs?
- Clinical outcomes groups?
- Are residents presenting at AAOS and subspecialty meetings?
Fit this with your goals:
- If you want a highly academic career or competitive fellowship:
- Robust research support is a major plus.
- If research is not a strength or interest for you:
- Look for programs that value clinical skill and are not research-saturated, but still meet minimum scholarly requirements.
E. Fellowship Match and Career Outcomes
Review recent fellowship match lists (often posted on program sites or available by request):
- Are graduates matching into:
- Well-regarded fellowships in joints, sports, trauma, etc.?
- Geographic or institutional areas you value?
- Are some graduates going directly into practice (especially in community-oriented programs)?
Don’t overinterpret a single year, but look for patterns over several years.
F. Program Culture, Mentorship, and Support
This is harder to quantify but often decides whether you thrive.
Consider:
- How do residents describe their experience?
- Collegial vs. hierarchical
- Supportive vs. “malignant”
- Is there visible mentorship:
- Formal mentorship pairings?
- Access to faculty across subspecialties?
- Professional development:
- Teaching on contract negotiation, billing, medico-legal topics?
- Support for attending national meetings?
Red flags:
- High attrition or residents transferring out, especially repeatedly.
- Residents not speaking freely around faculty during open houses or interviews.
- Persistent rumors (from multiple sources) of poor treatment or lack of support.
G. Location, Cost of Living, and Lifestyle
Even in a demanding specialty like orthopedics, life outside the hospital matters.
Evaluate:
- Cost of living and typical resident salary vs. housing costs
- Commute times (especially if rotation sites are spread out)
- Childcare options, schools, support systems
- Fit with your and your family’s lifestyle (outdoors, cultural activities, etc.)
You don’t need to love the city forever—but you should be able to tolerate and function well there for five years.
Step 5: Constructing a Strategic Ortho Match List
Once your data is compiled, you must turn it into a coherent application strategy.
A. Categorize Programs: Reach, Target, Safety
Based on your self-assessment and research, label each program:
- Reach programs
- Historically match applicants with metrics and research above yours.
- Highly prestigious or extremely competitive locations.
- Target programs
- Your profile matches or slightly exceeds typical matched residents.
- Safety programs
- Newer programs, smaller markets, or institutions that have matched applicants with profiles similar to or below yours.
Typical distribution for an MD graduate in orthopedic surgery (adjust based on competitiveness and resources):
- Total programs: 60–80+ (orthopedics is very competitive; some apply to >80)
- ~20–30% Reach
- ~40–50% Target
- ~20–30% Safety
If you’re less competitive:
- Increase safety and modest target programs.
- Consider also:
- New or recently accredited programs
- Community-based or hybrid programs
- Geographically less popular regions
B. Aligning Applications with Your Story
Your research is not just logistical; it feeds directly into your application materials:
Personal statement
- Highlight experiences and goals that align with the type of programs you’re prioritizing (academic vs. community, trauma-heavy vs. sports-heavy, etc.).
Program-specific signals (if applicable, e.g., signaling systems used by some specialties)
- Use signals on programs where:
- Your interests and their strengths match well
- You’ve done a sub-I, research, or have a personal connection
- Use signals on programs where:
Interview preparation
- Use your spreadsheet notes to generate questions and talking points:
- “I saw that your graduates frequently match into sports medicine fellowships; could you tell me more about your partnerships with those programs?”
- “I noticed you have a dedicated research year. How do residents typically structure this time?”
- Use your spreadsheet notes to generate questions and talking points:
Step 6: Practical Tips, Common Pitfalls, and Example Scenarios
A. Common Mistakes in Program Research
Focusing only on prestige
- A big name does not guarantee strong operative exposure or a healthy culture.
Underestimating safety programs
- You may need them to secure a match, and many produce excellent surgeons.
Ignoring personal fit
- A program’s style (very aggressive vs. more supportive) may not match your learning needs.
Overweighting one data point
- Don’t reject a program solely due to one negative comment or one weaker metric.
Not updating your list
- Programs change: new chair or PD, loss/gain of trauma designation, accreditation changes.
B. Example: Two MD Graduates, Two Strategies
Applicant A: Highly academic, research-heavy
- MD from top-tier allopathic medical school
- High Step scores, 10+ ortho publications, strong letters from academics
- Goal: Academic career in sports medicine
Program research strategy:
- Prioritize large academic centers with:
- Strong sports services and fellowships
- Significant research infrastructure
- Track record of sports medicine fellowship placement
- List might be ~70 programs:
- 25 elite academic/research programs (reach)
- 30 solid academic/hybrid programs (target)
- 15 community/hybrid programs with decent research opportunities (safety)
Applicant B: Solid clinician, modest research
- MD from mid-tier allopathic medical school
- Mid-range scores, limited ortho research, very strong clinical evaluations
- Goal: Community practice with possible trauma or joints fellowship
Program research strategy:
- Focus on:
- Strong operative volume
- Community or hybrid programs
- Solid but not necessarily top-tier academic centers
- List might be ~80 programs:
- 15 highly competitive academic centers (reach)
- 40 mid-tier academic and hybrid programs (target)
- 25 community and newer programs with strong case volume (safety)
Both applicants are competitive in different lanes; thorough, tailored research helps each build a rational list.
Frequently Asked Questions (FAQ)
1. How many orthopedic surgery programs should an MD graduate apply to?
For the allopathic medical school match in orthopedic surgery, many MD graduates apply to 60–80+ programs. The exact number depends on:
- Your competitiveness (scores, research, letters, school reputation)
- Presence of a strong home ortho program
- Willingness to relocate broadly
Less competitive applicants should generally err on more applications and a wider geographic spread, with a higher proportion of safety programs.
2. How important is program prestige compared to operative volume?
Prestige can:
- Help with highly competitive fellowships
- Offer broader academic networking opportunities
However, for most careers, operative volume, case mix, and quality of training matter more for your daily practice. A “mid-tier” program with outstanding surgical exposure and supportive teaching can produce an excellent orthopedic surgeon who is well-positioned for both community and many academic paths.
3. What if I don’t know my subspecialty interest yet?
You do not need to know your exact subspecialty when applying. Look for:
- Balanced exposure across subspecialties (trauma, joints, sports, hand, spine, peds, etc.)
- A diversity of fellowship outcomes among graduates
- Mentorship opportunities that will help you explore different fields
Programs with broad case mix and strong mentorship will support your exploration during residency.
4. How can I research program culture if I can’t visit in person?
Use a combination of:
- Virtual information sessions and open houses
- Program social media posts (pay attention to resident interactions and tone)
- Conversations with:
- Current residents (via email or LinkedIn)
- Alumni of your medical school at those programs
- Pay close attention during interviews:
- How residents talk about each other and their leadership
- Whether they feel comfortable discussing challenges as well as strengths
No single source is perfect, but consistent patterns across multiple perspectives are highly informative.
By approaching your orthopedic surgery residency search with a structured program research strategy, you maximize your chances of not just matching, but matching into a program where you can become the kind of orthopedist you aspire to be. Use your spreadsheet, stay honest about your strengths and needs, and let your research guide a thoughtful, well-balanced application plan.






















