
Understanding the Landscape of Interventional Radiology Residency
Interventional radiology (IR) is one of the most competitive and rapidly evolving specialties. Because of its hybrid nature—procedural, imaging-based, and clinically focused—choosing the right interventional radiology residency is fundamentally different from picking many other specialties. Effective program research is not optional; it’s a critical strategy for both matching and thriving in training.
Interventional radiology residency in the U.S. typically follows three main pathways:
Integrated IR Residency (IR/DR)
- 6-year program (1 year of clinical internship + 5 years IR/DR residency)
- Leads to dual board eligibility in Interventional Radiology and Diagnostic Radiology
- Highly competitive; requires early and strategic program research
Independent IR Residency
- 2-year program following completion of a diagnostic radiology residency
- Separate match (NRMP) and often highly selective
- Requires long-term program research strategy starting in DR residency
Early Specialization in IR (ESIR)
- A pathway within DR residency that gives you advanced standing for an independent IR residency
- Not a residency by itself, but a track that strongly influences your later options
Because IR training structures and resources vary widely between institutions, you cannot rely on name recognition alone. A systematic, deliberate approach to researching programs will help you:
- Build a more competitive and targeted IR match list
- Avoid programs that don’t fit your procedural or clinical goals
- Maximize your IR training experience and long-term career satisfaction
The rest of this guide outlines how to research residency programs in IR—step-by-step, with concrete tools, questions, and examples.
Step 1: Clarify Your Personal and Professional Priorities
Before diving into program websites or spreadsheets, you need a clear internal compass. The most effective program research strategy starts with understanding what you want from IR training.
A. Clinical and Procedural Interests
Ask yourself:
- Which IR domains excite you most?
- Oncologic interventions (Y-90, TACE, tumor ablations)
- Peripheral arterial disease and complex vascular work
- Venous disease and thrombectomy
- Interventional oncology plus palliative procedures
- Women’s health (fibroid embolization, pelvic congestion)
- Trauma and emergent procedures
- Dialysis access, venous access, IVC filters
- Pediatric IR
- Are you drawn more to:
- High-acuity, emergent IR (trauma, massive bleeding)?
- Longitudinal outpatient care (clinic-heavy, chronic disease)?
- Image-guided oncology and multidisciplinary cancer care?
Your answers will shape what to look for when evaluating residency programs. For example, if you are passionate about interventional oncology, you’ll prioritize centers with high cancer volumes, tumor boards, and dedicated IO faculty.
B. Career Aspirations
Consider your long-term goals:
- Academic vs. community practice
- Desire for research or advanced degrees (MPH, MS, PhD)
- Interest in education, leadership, or administration
- Geographic flexibility and family considerations
This matters because:
- Academic IR careers often benefit from research-heavy training and protected research time.
- Community-focused careers may benefit from broad procedural exposure and earlier autonomy.
- If you want to lead a service line, programs with strong clinic and consultation models are essential.
C. Lifestyle and Location Factors
Be honest about:
- Geographic regions you prefer or must avoid
- Tolerance for call intensity and nights/weekends
- Cost of living and support systems (family, partners)
These are not “soft” factors; they influence burnout, learning, and performance. Your IR match strategy should balance training quality with personal sustainability.
Actionable step:
Write a one-page “training priorities statement” listing:
- 3–5 non-negotiables (e.g., must have robust IR clinic, must be in the Southeast, must have ESIR)
- 5–8 “nice-to-haves” (e.g., strong IR research, level 1 trauma center, high oncologic case volume)
You will use this document as a lens for evaluating residency programs.
Step 2: Build a Structured Program Research Strategy
Once your priorities are clear, you need a systematic approach for how to research residency programs in IR. Avoid aimlessly browsing; treat this like a project.
A. Start With Official Data Sources
For integrated and independent IR programs, begin here:
ACGME Program Search
- Lists accredited IR/DR and independent IR residencies
- Confirms accreditation status, program size, and sponsoring institution
FREIDA (AMA Residency & Fellowship Database)
- Filter for “Interventional Radiology – Integrated” and “Interventional Radiology – Independent”
- Provides basic stats (positions, program type, contact info)
NRMP data & Charting Outcomes
- Gives a macro view of competitiveness, match stats, and applicant characteristics
- Not program-specific, but useful for realistic self-assessment
Create an initial spreadsheet of all programs that are geographically acceptable and fit your basic preferences (university vs community, program size, etc.).
B. Use Program Websites Strategically
Program websites are marketing tools, but they still contain valuable data. For each program, systematically capture:
Program structure
- Rotations by year (how much IR vs DR, ICU, surgery, clinic)
- ESIR opportunities if you’re starting in DR
- Call structure (IR call, DR call, night float)
Case mix and volume
- Types of procedures emphasized (e.g., IO vs trauma vs PAD)
- Specialized services (e.g., TIPS, complex aortic interventions, biliary work, transplant-related IR)
- Any mention of annual procedure counts per resident/fellow
Faculty and leadership
- Number of IR faculty
- Subspecialty expertise (IO, pediatrics, neuro-IR, etc.)
- PD and chair backgrounds—academic, research, leadership style (to the extent you can infer)
Clinical model
- IR clinic: frequency, ownership of patients, pre- and post-procedure follow-up
- Inpatient consult service vs primarily procedure-based service
- Participation in multidisciplinary conferences
Research and academics
- Ongoing IR clinical trials and research areas
- Recent IR publications from faculty and residents
- Opportunities for projects, QI, and presentations
Tip: As you go, annotate your spreadsheet with short notes (e.g., “Strong IO; multiple Y-90 physicians,” “No mention of IR clinic,” “Heavy transplant liver volume”).
C. Leverage Databases, Social Media, and Resident-Generated Content
Modern IR programs maintain a presence beyond their official website. These channels often reveal what the program truly values.
Program social media (Twitter/X, Instagram, LinkedIn)
- Look for:
- Resident life posts (camaraderie, social events)
- Case highlights and procedural diversity
- Conferences attended (SIR, RSNA, CIRSE, others)
- Education culture (teaching sessions, journal clubs)
- Look for:
Student and resident forums/blogs
- Specialty forums, Reddit subs, or unofficial resources sometimes discuss culture, workload, and red flags.
- Interpret anecdotally—use as prompts for questions, not as final truth.
SIR (Society of Interventional Radiology) resources
- Medical student and resident sections
- Lists of IR training programs, educational offerings, and mentoring opportunities
- Webinars and panels often include PDs describing their programs’ philosophies
Actionable step:
Create a short “program snapshot” entry (4–6 bullet points) in your spreadsheet for each program summarizing its identity and strengths based on these sources. This will make comparisons easier later.
Step 3: Key Dimensions for Evaluating IR Residency Programs
Once you’ve collected raw information, you need to interpret it through the lens of high-yield IR training factors. This is where true evaluating residency programs skill comes in.
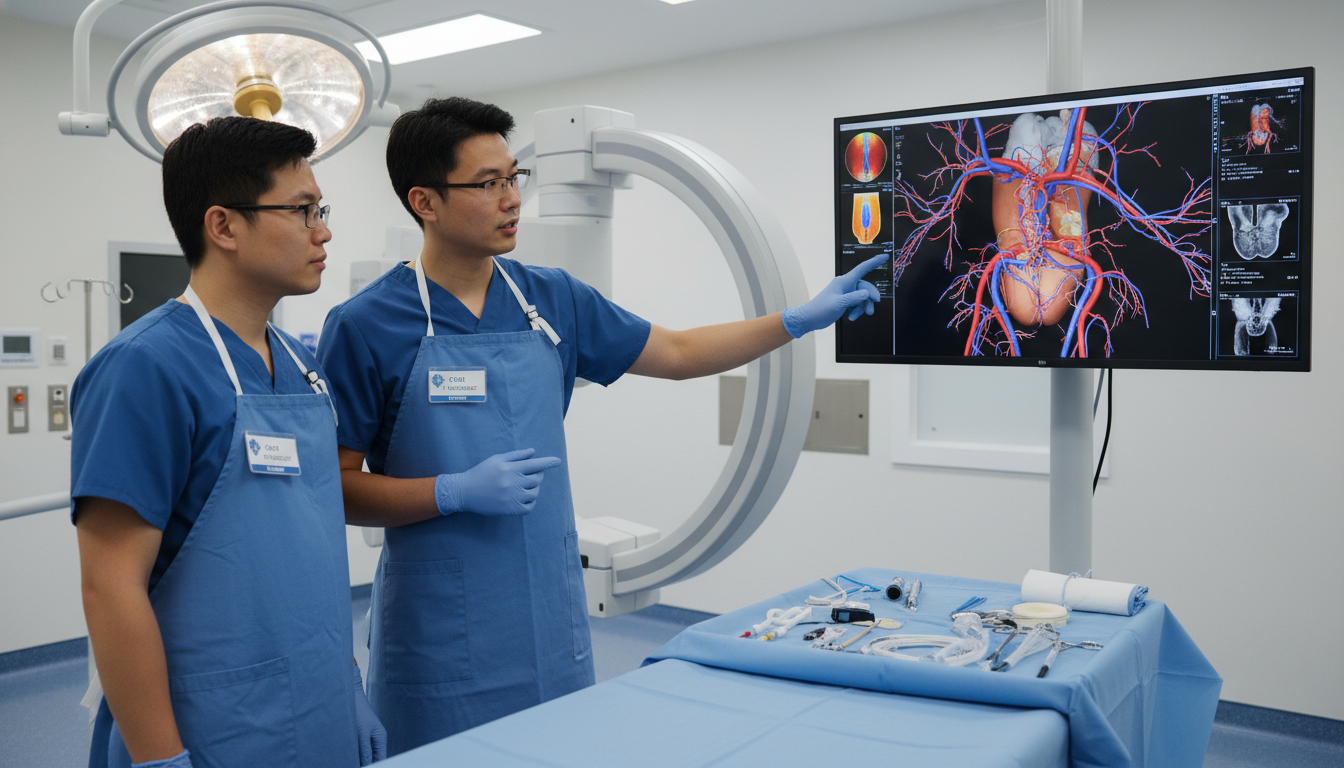
A. Procedural Case Mix and Autonomy
IR is fundamentally procedural; case mix and hands-on experience will shape your career.
Questions to research and later ask:
What is the breadth of procedures?
- Does the program cover:
- IO (ablation, embolization, Y-90)?
- PAD interventions?
- Complex venous interventions and thrombectomy?
- Women’s health procedures?
- Trauma embolization and emergent interventions?
- Biliary, portal, and transplant-related work?
- Does the program cover:
What is the depth and independence?
- Do residents get primary operator experience early?
- Is there a graduated autonomy structure?
- Are certain procedures dominated by attendings or fellows (e.g., highly complex IO)?
Are there fellowships or competing services that limit exposure?
- Vascular surgery, cardiology, neuro-IR, or transplant surgery may overlap with IR procedures
- Ask how cases are divided in practice
Look for programs that both protect core IR procedures for trainees and offer progressive independence while maintaining safety.
B. Clinical Training and IR Clinic
Modern IR is not just a procedural consult service; it’s a clinical specialty.
Key features to identify:
IR clinic structure
- How many half-days per week?
- Are IR residents seeing new patients and follow-ups themselves?
- Is there exposure to longitudinal care (e.g., PAD, oncology follow-up, dialysis access patients)?
Inpatient consults
- Does IR own certain patient populations (e.g., post-TIPS, complex access)?
- How integrated is IR with hospitalist and specialty teams?
Multidisciplinary involvement
- Tumor boards (hepatobiliary, thoracic, GI oncology, etc.)
- PAD or limb salvage conferences
- Complex case conferences and morbidity & mortality (M&M)
You’ll graduate as an IR physician, not just a proceduralist. Programs that emphasize clinic and longitudinal care are increasingly valued in the field and by employers.
C. Diagnostic Radiology Training Quality
For integrated IR/DR:
- Evaluate the DR component just as critically:
- Breadth of imaging rotations (neuro, MSK, body, chest, cardiac, pediatrics)
- Call exposure and imaging responsibility
- Quality of teaching and supervision
You will be a dual IR/DR diplomate; strong DR fundamentals directly improve your procedural planning and complication management.
D. Call, Workload, and Resident Culture
Sustainable, supportive environments enhance learning.
Investigate:
Call structure
- How often are IR residents on call?
- In-house vs home call?
- What is the mix of emergent vs elective cases?
Workload
- Average daily procedure volume per resident
- Expectations for pre-procedure workup and post-procedure notes
- Involvement in admissions and discharges (varies by program)
Culture and wellness
- Resident-to-resident relationships (mentorship, support, inclusivity)
- Faculty accessibility and approachability
- Institutional wellness efforts (counseling, mentorship programs, schedule flexibility)
Talk directly with residents (via emails, virtual meet-and-greets, or away rotations) to validate what you see on paper. Culture is difficult to quantify but profoundly affects your training.
E. Research, Mentorship, and Career Development
For many IR applicants, academic productivity and mentorship are differentiators.
Assess:
Research infrastructure
- Ongoing IR-specific trials or registries
- Availability of statisticians, research coordinators
- Funding support for conference travel
Mentorship structure
- Formal advisor or mentor assignment
- Track record of residents presenting at SIR, RSNA, and subspecialty meetings
- Match outcomes—where graduates go (academics vs community; top fellowships or jobs)
Even if you are not research-oriented, programs with strong mentorship often excel at guiding residents toward the IR match, independent residencies, or jobs that truly fit them.
Step 4: Applying Your Strategy to Different IR Pathways
How you research programs will vary slightly depending on whether you’re aiming for integrated IR, ESIR within DR, or independent IR.
A. Researching Integrated IR Residency Programs
For integrated IR:
Focus on:
- Early IR exposure (how soon do you get into the IR suite?)
- Balance between DR and IR throughout the 5 clinical years
- Whether IR residents have a distinct identity and curriculum vs being “just DR residents who later do IR”
High-yield questions:
- “What does a typical week look like for a PGY-3 integrated IR resident?”
- “When do IR residents first take IR call, and at what level of independence?”
- “How do integrated IR residents coordinate with DR residents for rotations and case sharing?”
B. Researching Diagnostic Radiology Programs with ESIR
If you’re targeting DR with ESIR:
Confirm:
- Is ESIR offered and ACGME-approved?
- How many ESIR slots per year, and how competitive are they?
- Are ESIR slots guaranteed for interested residents or selective?
Evaluate:
- The strength and size of the IR division within the DR program
- Whether ESIR residents get genuinely meaningful IR clinic and consult exposure
- Track record of ESIR graduates successfully matriculating into independent IR residencies
This is where evaluating residency programs becomes nuanced: a DR program with a robust IR presence and well-structured ESIR can be an excellent IR career launchpad.
C. Researching Independent IR Residency Programs
For those already in DR or ESIR:
Prioritize:
- Depth of advanced IR procedures and complexity
- Graduated autonomy and senior-level responsibility
- Exposure to practice-building, billing, and service-line management
Key questions for independent IR:
- “How are responsibilities divided between independent residents and integrated IR residents, if both exist?”
- “What does the typical caseload and call schedule look like for independent trainees?”
- “Where have recent independent IR graduates gone—academics vs community, geographic spread?”
This targeted approach keeps your program research strategy aligned with your training stage and ultimate goals.
Step 5: Using Direct Contact, Rotations, and Interviews to Refine Your List
Paper and web research have limits. To complete your evaluation, you’ll need direct interaction with programs.
A. Away Rotations and Sub-Internships
For competitive fields like IR, away rotations can be invaluable for both learning and program research.
Use them to:
- Observe day-to-day workflow and culture
- Gauge how attendings teach (at the table, in conferences, in clinic)
- Assess how much responsibility residents are given
- Clarify unadvertised details about call, case allocation, and autonomy
Ask residents candid, but respectful, questions:
- “What do you think this program does exceptionally well?”
- “If you could change one thing about the IR training here, what would it be?”
- “How supported do you feel when you want to attend conferences or pursue research?”
B. Virtual Open Houses and Information Sessions
Many IR/DR and independent programs host virtual info sessions, particularly around application season.
Make these sessions count:
- Prepare 3–5 program-specific questions aligned with your priorities
- Pay attention not only to what they say, but how they respond—do they acknowledge limitations honestly or oversell?
- Note how residents talk about their experiences—forced or genuine?
Examples of high-yield questions:
- “Can you walk us through how IR clinic is structured and how residents are involved?”
- “How do you support residents who are interested in specific niches like interventional oncology or PAD?”
- “What changes have you made in the last 3–5 years to improve IR resident education?”
C. Interview Season: Deep-Dive Evaluation
Interviews are not just about impressing programs; they are critical opportunities to validate or revise your impressions.
During interviews, focus on:
- asking detailed follow-ups about any unclear aspects from your research
- exploring culture and mentorship chemistry
- observing nonverbal dynamics between residents and faculty on group calls or dinners
Maintain a structured note template for each program, including:
- Strengths (aligned with your non-negotiables)
- Concerns or potential red flags
- “Vibe” fit: did you feel comfortable with the residents and faculty?
After interview season, use your notes plus your original priorities statement to rank programs rationally rather than emotionally.
Step 6: Common Pitfalls and How to Avoid Them
Even strong applicants can undermine their IR match by using a weak program research strategy. Common mistakes include:
A. Overweighting Name Recognition
Large, famous institutions are not automatically the best IR training environments for you.
- Some big names have excellent DR but weaker IR, or vice versa.
- Others may have strong IR but limited resident autonomy due to heavy attending or fellow involvement.
Always cross-check reputation against the concrete training features you care about.
B. Ignoring Fit in Favor of Competitiveness
Targeting only the most competitive interventional radiology residency programs without considering fit can backfire:
- You may struggle in a culture that doesn’t align with your learning style.
- Programs might sense a mismatch and rank you lower.
Better outcomes come from a balanced list where you could genuinely thrive.
C. Relying on One Data Source
No single source (websites, forums, a friend’s opinion) gives the full picture. Triangulate:
- Official data + real-time social media + resident conversations + your in-person/virtual interactions.
- When two or three sources align (e.g., everyone mentions strong mentorship), that signal is more reliable.
D. Underestimating the Importance of Clinical IR Training
Programs that are heavily procedure-centric but neglect clinic, consults, and longitudinal care may leave you underprepared for modern IR practice. Be wary of environments where IR is treated as a purely procedural service with minimal clinical identity.
FAQs: Researching Interventional Radiology Residency Programs
1. How many interventional radiology residency programs should I research and apply to?
There’s no universal number, but many IR applicants start by researching 30–40 integrated programs and then narrowing to 20–30 applications based on fit, competitiveness, and geography. For independent IR, the pool is smaller, so applicants often research nearly all programs that meet their criteria, then apply broadly. Let your competitiveness profile and advisor guidance shape the final number.
2. What’s the best way to compare programs objectively?
Create a standardized comparison spreadsheet with categories tied to your priorities: case mix, call schedule, IR clinic exposure, research opportunities, culture, location, and graduate outcomes. Score or color-code each category (e.g., 1–5 or green/yellow/red). This structure reduces bias and makes it easier to see which programs consistently align with your goals.
3. How do I find out the “real” culture of a program beyond the website?
The most reliable methods are direct resident conversations and away rotations. Attend virtual open houses, ask for resident contact emails if not provided, and have brief, focused chats asking about day-to-day life, mentorship, and support. Use anonymous forum comments only as prompts for questions, not as final verdicts.
4. Should I prioritize programs with ESIR or independent IR positions when I’m still a medical student?
If you know you want IR, integrated IR/DR is the most direct path. However, strong DR programs with robust ESIR can be equally effective routes, especially if integrated spots are limited or you value more flexibility early in training. When evaluating residency programs with ESIR, look at how many residents actually complete ESIR, how competitive entry is, and how successful they are in the IR match for independent positions.
By approaching program research with a deliberate, multi-step strategy—starting from your own priorities, gathering structured data, and validating through real interactions—you’ll be far better equipped to choose interventional radiology residency programs where you can excel, grow, and ultimately practice the kind of IR that inspired you to pursue this specialty in the first place.






















