
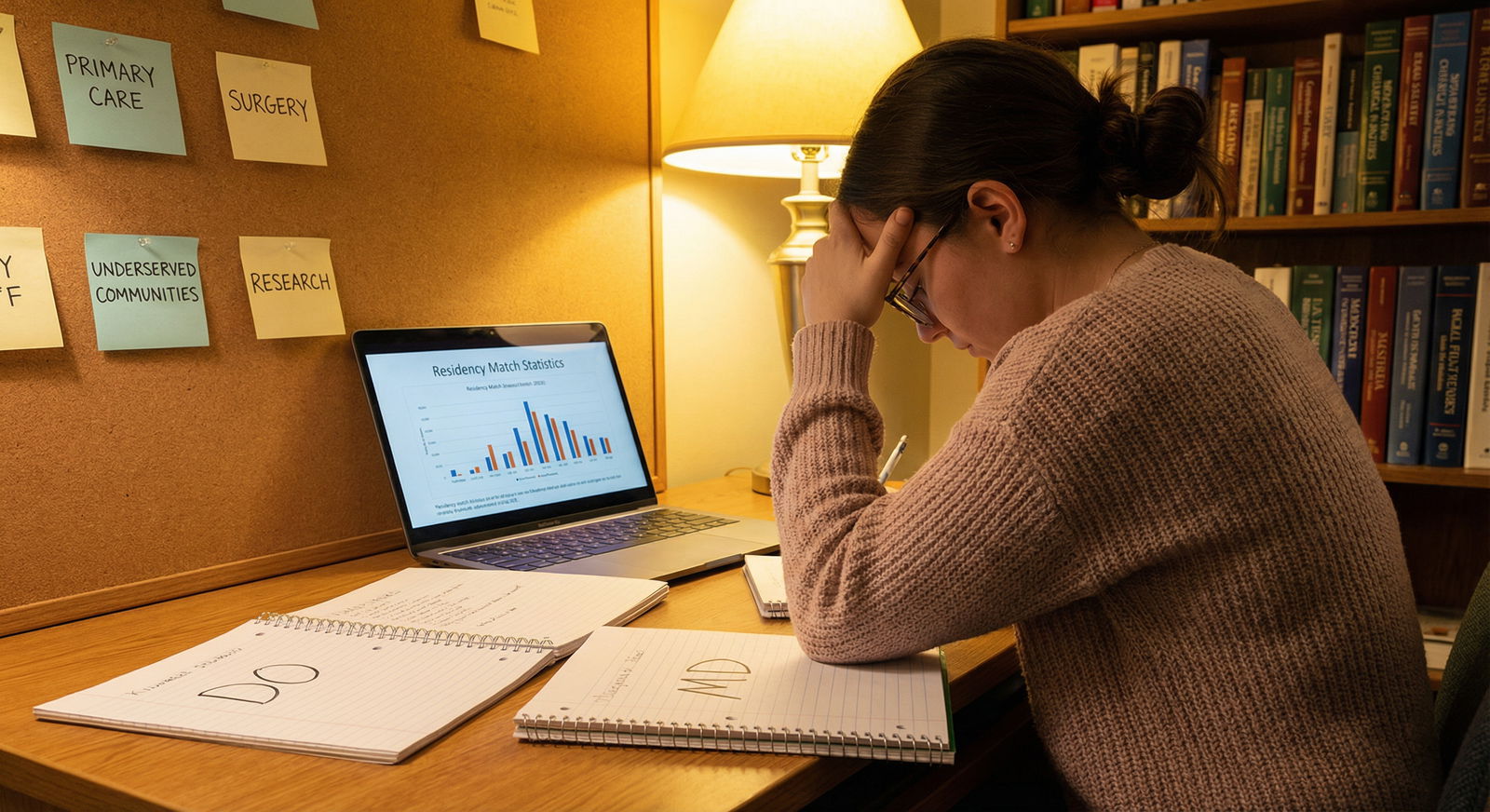
Choosing Between DO and MD: A Detailed Guide for Future Physicians
When planning a career in medicine, one of the earliest and most important decisions is whether to pursue a Doctor of Osteopathic Medicine (DO) or a Doctor of Medicine (MD) degree. Both lead to a full medical license and allow you to practice in every state and specialty, but they differ in philosophy, training emphasis, and sometimes public perception.
For premeds and early medical students navigating Medical Education and Healthcare Careers, understanding DO vs MD is critical. This guide expands on the basics and adds context from current trends in physician training, residency placement, and long-term career outcomes.
DO vs MD Fundamentals: Definitions, Philosophy, and Scope
What Is a DO?
A Doctor of Osteopathic Medicine (DO) is a fully licensed physician who can practice in all areas of medicine: primary care, surgery, subspecialties, academic medicine, and more. DOs:
- Complete four years of osteopathic medical school
- Train in the same core biomedical sciences as MDs
- Undergo additional training in osteopathic manipulative treatment (OMT)—hands-on techniques used to diagnose, treat, and support the body’s function
- Are trained from day one to think holistically, considering:
- The interconnection of body systems
- The patient’s lifestyle, mental health, and environment
- Prevention and health promotion, not just disease management
The core osteopathic philosophy is often summarized as:
- The body is a unit of body, mind, and spirit.
- The body is capable of self-regulation and self-healing.
- Structure and function are interrelated.
- Rational treatment is based on these principles.
In practice, many DOs use OMT in primary care, sports medicine, and certain specialties, while others use it rarely or not at all depending on their specialty and setting. However, the holistic mindset typically remains part of how they approach patient care.
What Is an MD?
A Doctor of Medicine (MD) is also a fully licensed physician, trained in what is often called allopathic medicine—the traditional, research-driven, disease-focused approach that most people associate with “medical school.” MDs:
- Complete four years of allopathic medical school
- Focus heavily on:
- Pathophysiology of disease
- Evidence-based use of medications, procedures, and surgery
- Diagnostic reasoning and clinical decision-making
- May or may not explicitly emphasize holistic care in the curriculum, although modern MD programs increasingly incorporate:
- Social determinants of health
- Patient-centered communication
- Wellness and preventive medicine
In practice, many MDs also provide holistic, preventive care; the difference is more about educational emphasis and historical tradition than strict boundaries.
Are DOs and MDs Equal in Practice?
From a legal and functional standpoint in the United States:
- Both are physicians with equivalent rights and responsibilities.
- Both can:
- Prescribe medications
- Perform surgery
- Lead healthcare teams
- Enter any specialty (assuming they match to the appropriate residency)
- Both are recognized by:
- Hospitals and health systems
- Insurance companies
- Licensing boards
- Federal agencies (e.g., VA, military, public health service)
In many clinical settings, patients often don’t recognize or don’t differentiate between DO and MD unless it is explained.
Key Philosophical and Training Differences
Educational Philosophy
- DO programs
- Formal emphasis on holistic care and the musculoskeletal system
- Structured training in OMT
- Often highlight primary care and serving underserved communities, though many DOs go into specialties
- MD programs
- Strong focus on biomedical science and disease mechanisms
- Historically more research-oriented (though this is changing as many DO schools expand research infrastructures)
- Often associated with larger academic medical centers
- DO programs
Clinical Techniques
- Both DOs and MDs use medications, surgery, and standard medical interventions.
- DOs receive 200–400+ hours of OMT training, learning techniques like:
- Muscle energy
- High-velocity low-amplitude (HVLA)
- Myofascial release
- Counterstrain
- Whether and how often OMT is used varies widely by individual physician, specialty, and practice setting.
Perception and Culture
- Historically, MD degrees have been more widely recognized internationally.
- In the U.S., DOs are increasingly represented in academic centers, leadership positions, and competitive specialties.
- Some older misconceptions remain, but among younger physicians and many program directors, DO vs MD is far less of a dividing line than it used to be.

Admissions and Application Process: DO vs MD Programs
For premed students, the admissions journey into Medical School is similar for both degree types, with some important nuances that can influence strategy.
Core Admissions Requirements
Most DO and MD schools share the following baseline requirements:
- Bachelor’s degree (or nearly complete):
- Premed prerequisites: general biology, general and organic chemistry, physics, biochemistry, and often statistics and psychology/sociology
- MCAT:
- Required for essentially all U.S. DO and MD schools
- DO programs may sometimes consider slightly lower MCAT scores, but this gap is narrowing as osteopathic schools become more competitive
- GPA:
- Strong science GPA is critical for both
- Successful DO matriculants often have slightly lower average stats than MD matriculants, but there is substantial overlap
- Letters of Recommendation:
- From science faculty, non-science faculty, and often at least one physician
- Some DO schools strongly prefer or require a letter from a DO physician, which means you should plan shadowing or clinical exposure with a DO if you are considering that path
- Clinical, volunteer, and research experience:
- Essential for both pathways
- DO schools may be more forgiving of less research if clinical service and community involvement are strong
- Personal Statement and Secondary Essays:
- Used to assess your motivation, insight, resilience, and fit with the school’s mission
- For DO schools, explicitly articulating interest in osteopathic philosophy and holistic care is important
Centralized Application Services
MD Programs:
Use AMCAS (American Medical College Application Service)- Allows applicants to apply to nearly all U.S. allopathic medical schools
- Common primary application, school-specific secondary essays
DO Programs:
Use AACOMAS (American Association of Colleges of Osteopathic Medicine Application Service)- Centralized application for U.S. osteopathic schools
- Similar structure to AMCAS with primary and secondary components
Many applicants now apply to both DO and MD schools in a single cycle, tailoring their essays and school lists to match their competitiveness and interests.
Strategic Considerations for Applicants
- Competitiveness:
- If your stats are borderline for MD programs, adding DO schools may significantly increase your chances of becoming a physician.
- Mission Fit:
- If you are drawn to primary care, rural medicine, or a biopsychosocial approach to health, DO schools may align strongly with your values.
- Shadowing:
- If you consider DO programs, actively seek out DO physicians to shadow to:
- Understand osteopathic practice
- Secure a potential DO letter of recommendation
- If you consider DO programs, actively seek out DO physicians to shadow to:
- International Plans:
- If you plan to practice outside the U.S., research how DO degrees are recognized in your target country; MD degrees may currently face fewer barriers internationally in some regions.
Medical School Training and Curriculum: How DO and MD Paths Compare
Preclinical Training (Years 1–2)
Both DO and MD schools:
- Cover core foundational sciences:
- Anatomy, physiology, biochemistry
- Pathology, microbiology, pharmacology
- Clinical skills and early patient interaction
- Increasingly use systems-based, integrated curricula and active learning methods (small groups, case-based learning, simulation)
DO programs add:
- Dedicated OMT labs and lectures throughout preclinical years
- Emphasis on:
- Musculoskeletal exam skills
- Palpatory diagnosis
- Integrating manual medicine into standard care plans
MD programs often emphasize:
- Research literacy and critical appraisal of the literature
- Exposure to subspecialties and academic medicine, especially in large teaching hospitals
Clinical Rotations (Years 3–4)
For both DO and MD students, clinical years typically include core rotations in:
- Internal medicine
- Surgery
- Pediatrics
- Obstetrics and gynecology
- Psychiatry
- Family medicine
- Emergency medicine
After core rotations, students pursue electives and sub-internships (sub-Is) in areas of interest, often at institutions that host desired residency programs.
Practical differences can include:
- Affiliated hospitals and networks:
- Some DO schools historically relied more on community hospitals, though many now have strong academic affiliations.
- MD schools are often embedded in large academic centers but also use community sites.
- Use of OMT during clinical years:
- Some DO students use OMT regularly, especially in family medicine, sports medicine, or OMT clinics.
- Others use it selectively, depending on preceptors and patient population.
Exams During Medical School
- DO students:
- Take the COMLEX-USA Level 1, 2-CE, and (optionally) Level 3 as the osteopathic licensing exams.
- Historically, many DO students also took the USMLE Step exams to be competitive for certain residency programs, though this strategy is evolving as more residencies are comfortable with COMLEX alone.
- MD students:
- Take the USMLE Step 1, Step 2 CK, and Step 3 series.
Both sets of exams test similar medical knowledge and clinical reasoning. Step 1 and COMLEX Level 1 are now pass/fail, which slightly shifts emphasis toward Step 2/Level 2, clinical grades, research, and extracurricular achievements.
Residency Training, Licensure, and Practice After Graduation
Unified Residency System and Match
Historically, DO and MD graduates applied to separate residency systems. Now:
- The U.S. has a single, unified accreditation system under the ACGME.
- DO and MD graduates both apply through the NRMP Match and enter ACGME-accredited programs.
- DOs are eligible for all ACGME residencies, and many programs explicitly state they welcome DO applicants.
Match outcomes:
- DOs and MDs both match into:
- Primary care (family medicine, internal medicine, pediatrics)
- Competitive fields (EM, anesthesia, radiology, PM&R, some surgical subspecialties)
- MDs remain somewhat overrepresented in the most competitive specialties and top academic programs, due in part to:
- Historical patterns
- Larger MD applicant pool
- Heavier emphasis on research in many MD programs
However, DO match rates and representation in competitive fields have risen steadily, and many DO physicians hold leadership positions in major hospitals and academic centers.
Licensure Exams and Requirements
To practice independently in the U.S.:
- DOs:
- Must pass COMLEX-USA exams
- Some states and certain employers may still recommend or favor USMLE scores, but this is decreasing
- MDs:
- Must pass USMLE Steps
Both then complete residency (3–7+ years depending on specialty) and may pursue fellowship training.
Scope of Practice and Career Settings
DOs and MDs share a fully overlapping scope of practice in the U.S.:
- Clinical settings:
- Academic medical centers
- Community hospitals
- Private practice
- Telemedicine
- Government/military/VA
- Non-clinical roles:
- Hospital and system leadership
- Public health
- Industry (pharma, biotech, medtech)
- Consulting
- Medical education and curriculum design
- Health policy
DOs are often more visible in primary care and community-based care, largely due to the historic mission of osteopathic medicine, but many now thrive in highly specialized fields.
Lifestyle, Satisfaction, and Compensation: DO vs MD in Real Life
Work–Life Balance and Burnout
Work–life balance for both MDs and DOs is shaped more by specialty and practice setting than by degree type.
- High-intensity specialties (e.g., surgery, EM, critical care) generally have more demanding hours and call, regardless of DO vs MD.
- Primary care, outpatient specialties, and certain subfields often offer more predictable schedules.
Some surveys have suggested:
- DOs report similar or sometimes higher satisfaction with:
- Patient relationships
- Sense of meaning in their work
- This may be linked to:
- Holistic, relationship-centered care models
- Higher proportion in primary care settings
However, burnout is a significant risk for all physicians. Factors that matter more than degree include:
- Practice culture
- Support staff and resources
- Autonomy and administrative burden
- Geographic location
- Personal coping strategies and support systems
Salary and Earning Potential
Compensation differences are driven overwhelmingly by specialty, region, and practice ownership, not by whether a physician is a DO or MD.
General trends:
- Primary care (FM, IM, peds): DOs and MDs in the same role typically earn similar salaries.
- Specialties (cardiology, ortho, derm, radiology, etc.):
Reported averages sometimes show MDs earning more, but this largely reflects:- Higher MD representation in the highest-paying subspecialties and markets
- Academic vs private practice variations
Approximate averages (which change year-to-year):
- MDs (all specialties combined): around $300K+ annually
- DOs (all specialties combined): slightly lower on average, but narrowing each year
Key takeaway:
If a DO and an MD with the same specialty, years of experience, and practice type work in the same region, their compensation is usually quite similar.
Future Trends in DO vs MD and How They Affect You
Several developments are reshaping the DO vs MD landscape:
- Growing number of DO schools and graduates:
- Osteopathic medical schools are expanding, particularly in regions with physician shortages.
- DOs now represent a substantial and growing share of the U.S. physician workforce.
- Increased DO presence in academic medicine:
- More DO faculty, program directors, and department chairs.
- Greater visibility of osteopathic physicians in research and leadership.
- Cultural shift toward holistic and preventive care:
- Public health and policy increasingly emphasize prevention, lifestyle medicine, and social determinants of health—all areas where osteopathic philosophy aligns strongly.
- Convergence of training models:
- Many MD schools teach communication skills, patient-centered interviewing, and integrative care.
- Many DO schools are strengthening research opportunities and academic affiliations.
For future physicians, the DO vs MD decision is less about what you can eventually do (since both open virtually all doors in U.S. healthcare) and more about:
- Where you see yourself fitting culturally and philosophically
- Which programs best align with your strengths and goals
- How you want to frame your identity as a physician
How to Decide Between DO and MD: Practical Steps and Considerations
Reflect on Your Values and Career Vision
Ask yourself:
- Do you strongly resonate with a holistic, hands-on approach to care?
- Are you passionate about primary care, rural health, or underserved populations?
- Or are you primarily drawn to research-heavy academic medicine or highly competitive subspecialties?
Both paths can get you to almost any destination, but:
- If holistic philosophy, OMT, and primary care appeal to you, DO may feel like a natural fit.
- If your dream is a research-intensive career at a top academic center or a super-competitive subspecialty, you may want to emphasize MD programs while still keeping DO programs in the mix.
Gain Direct Exposure
- Shadow both DO and MD physicians in different settings:
- Community clinic vs academic hospital
- Primary care vs specialty
- Ask them:
- Why they chose their pathway
- How (or whether) their degree matters in day-to-day practice
- What they would recommend to a premed today
Research Schools, Not Just Degree Type
Within both DO and MD categories, schools vary widely in:
- Location and clinical affiliations
- Research opportunities
- Class size and culture
- Primary care vs specialty focus
- Support for wellness and learning differences
Focus on “best fit” schools that match your statistics, mission alignment, and preferred learning environment.
Plan Your Application Strategy
Many successful applicants:
- Apply to a balanced mix of MD and DO schools
- Tailor essays to highlight:
- Interest in osteopathic principles for DO schools
- Fit with institutional missions and programs for MD schools
- Keep long-term goals in mind but remain flexible; interests often evolve during training.
FAQs: DO vs MD for Premeds and Future Residents
1. Is a DO “less than” an MD in terms of training or status?
No. In the U.S., DOs and MDs complete comparable lengths of education and training, are fully licensed physicians, and can practice in all specialties. Some older biases still exist in certain circles, but the gap is narrowing quickly, especially with a unified residency system. Your clinical skill, professionalism, and work ethic will matter far more than the letters after your name.
2. Can DOs get into competitive specialties and top residency programs?
Yes, but it can be more challenging in some fields and institutions. DOs do match into competitive specialties like orthopedic surgery, dermatology, radiology, and anesthesia, but:
- You may need stronger board scores, research, and networking.
- Taking USMLE (in addition to COMLEX) has historically helped DO applicants to certain programs, though some are now more comfortable with COMLEX alone.
- Strong performance in clinical rotations and sub-internships is critical.
If you are targeting a very competitive specialty, talk early with advisors who understand current match dynamics for DO students.
3. Is the DO degree recognized internationally?
Recognition varies by country:
- Many countries recognize DOs from U.S. osteopathic schools as fully qualified physicians.
- Some countries have limited recognition or additional licensing requirements.
- The situation is evolving, generally in a positive direction.
If you plan to practice outside the U.S., check the regulations of your target country in advance and consider whether an MD may be simpler for international mobility.
4. Do patients care whether their doctor is a DO or an MD?
Most patients primarily care about:
- How well you listen
- How clearly you explain diagnoses and treatments
- How effectively you help them feel better
Some patients actively seek DOs for a holistic approach or OMT. Others have no preference or are unfamiliar with the distinction. You can shape patients’ perceptions through clear communication about your training and approach.
5. Which degree should I choose if I’m not sure what specialty I want?
If your main goal is simply to become a physician and you are open-minded about specialty:
- Consider applying to both DO and MD schools.
- Focus on finding schools where:
- You feel you will be supported and challenged
- You have strong odds of admission
- The curriculum and mission resonate with you
Your specialty choice will depend far more on your experiences in clinical rotations and personal reflection than on whether you chose DO or MD at the outset.
Choosing between DO and MD is an important step in your Medical Education journey, but it is only one piece of your overall path in Physician Training. Both routes can lead to deeply fulfilling Healthcare Careers if you choose programs that fit your strengths, stay open to growth, and keep patient-centered care at the heart of your work.





















