
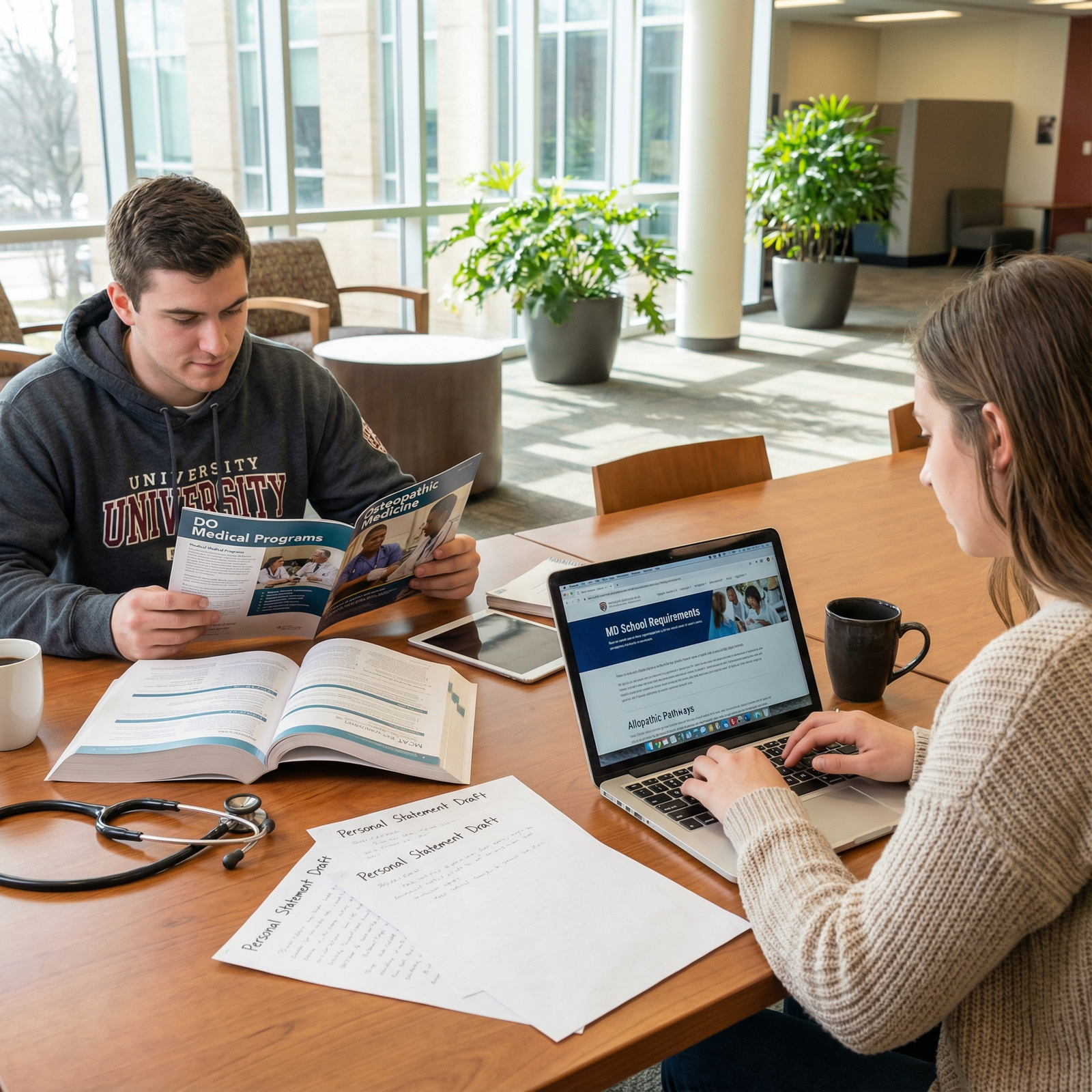
Introduction: Mapping Your DO vs MD Journey from Day One
Choosing between osteopathic medicine (DO) and allopathic medicine (MD) is one of the earliest major decisions in your Medical Education journey. Both degrees lead to becoming a fully licensed physician, eligible for residency, board certification, and independent practice. Yet the pathways differ in philosophy, training emphasis, and—sometimes—how residency programs perceive them.
If you’re a premed or early medical student wondering how DO vs MD will affect your application strategy, clinical training, Residency Matching, and long‑term career options, this guide walks you step‑by‑step from application to practice. You’ll learn not just “what’s different,” but also how to align each pathway with your values, strengths, and goals.
Core Philosophies: DO vs MD and How They Shape Training
Understanding the philosophical foundations of Osteopathic Medicine and allopathic medicine helps you interpret everything that follows—from curriculum to patient care.
The MD (Allopathic) Perspective: Disease-Focused and Data-Driven
The Doctor of Medicine (MD) degree is rooted in allopathic medicine, which traditionally emphasizes:
- Diagnosis and treatment of disease using medications, surgery, and technology
- Evidence-based practice driven by clinical trials, guidelines, and standardized protocols
- Organ- or system-based thinking, often with a path to early specialization
Key Characteristics of MD Medical Education:
- Strong emphasis on pathophysiology, pharmacology, and diagnostics
- Robust opportunities for laboratory and clinical research
- Early exposure to specialty fields (e.g., dermatology, neurosurgery, cardiology) through electives and interest groups
- Standard timeline: 4 years of medical school, followed by residency (3–7+ years depending on specialty)
In practice, MD and DO training overlap substantially in the modern era. Most MD curricula now include elements of wellness, communication skills, and prevention—but the historical core remains focused on diagnosing and treating disease as efficiently and effectively as possible.
The DO (Osteopathic) Perspective: Holistic, Preventive, and Hands-On
The Doctor of Osteopathy (DO) degree is built around Osteopathic Medicine, which emphasizes:
- The body as an integrated whole—mind, body, and spirit
- The body’s innate ability to heal itself given the right conditions
- Structure and function being interrelated (e.g., how musculoskeletal issues can affect overall health)
- Prevention and lifestyle as central to care
A defining element of DO training is Osteopathic Manipulative Treatment (OMT)—hands-on techniques applied to muscles, joints, and tissues to relieve pain, improve function, and support the body’s natural healing processes.
Key Characteristics of DO Medical Education:
- Holistic, patient-centered care emphasized from day one
- Required training in OMT/OMM (Osteopathic Manipulative Medicine)
- Frequent focus on primary care fields (family medicine, internal medicine, pediatrics, OB/GYN)
- Same timeline as MD: 4 years of medical school plus residency
How Philosophy Translates to Real Practice
In real-world clinical practice, the differences often look like this:
- MD: “How can I diagnose and treat this disease using the best evidence, medications, procedures, or surgeries available?”
- DO: “How can I diagnose and treat this condition while also considering lifestyle, environment, musculoskeletal issues, and the patient’s overall well-being?”
Many MDs provide very holistic, patient-centered care; many DOs use the same medications and surgical interventions as MDs. The philosophies are frameworks—your personal style as a physician will be shaped by both your degree and your individual training, mentors, and values.
Applying to Medical School: DO vs MD Application Strategies
The DO vs MD difference begins well before you put on a white coat. As a premed, your application strategy should consider both sets of programs—even if you are leaning strongly one way.
Shared Foundations: What DO and MD Schools Both Expect
For most applicants, the core requirements for both Physician Training pathways are similar:
1. Undergraduate Education and Prerequisites
- A bachelor’s degree (or near completion) by the time of matriculation
- Standard premed coursework:
- 1 year Biology with lab
- 1 year General Chemistry with lab
- 1 year Organic Chemistry with lab (sometimes replaced/augmented by Biochemistry)
- 1 year Physics with lab
- English/writing, statistics, and social science courses (varies by school)
- Strong GPA (both cumulative and science)
Actionable tip:
Check each target school’s website for specific prerequisite lists, as DO and MD schools can vary slightly in requirements and recommended coursework, especially for humanities / social science content.
2. Entrance Exam: MCAT
- Both DO and MD programs require the MCAT.
- DO schools may be somewhat more flexible in how they interpret scores, often considering upward trends, nontraditional paths, and holistic context.
- Very high MCAT scores remain a competitive advantage for both DO and MD programs.
Actionable tip:
If you anticipate a modest MCAT score but have strong clinical, volunteer, or nontraditional experiences, consider applying broadly to include a balanced mix of DO and MD schools where your profile fits.
3. Centralized Application Systems
- MD programs: American Medical College Application Service (AMCAS)
- DO programs: American Association of Colleges of Osteopathic Medicine Application Service (AACOMAS)
Both systems include:
- Primary application with personal statement
- Work/activities section (clinical, research, leadership, service)
- Letters of recommendation
- MCAT scores and transcripts
- Secondary applications with school-specific essay prompts
Unique DO vs MD Application Considerations
Applying to DO Programs: Holistic Fit and Osteopathic Interest
DO schools traditionally place high value on:
- Holistic evaluation: They look closely at your story, persistence, and service—not just metrics.
- Evidence you understand Osteopathic Medicine, not just that you “want to be a doctor.”
- Primary care interest (though many DOs match into specialties).
To strengthen a DO application:
- Seek shadowing with a DO physician if at all possible. Some DO schools strongly prefer or even require a letter from a DO.
- Use your personal statement or secondary essays to explicitly discuss:
- Why the DO philosophy appeals to you
- How you value preventive care, whole-person medicine, and OMT (if you’ve experienced or observed it)
- Highlight experiences that show empathy, community service, longitudinal relationships, and interest in underserved communities.
Applying to MD Programs: Academic and Research Emphasis
MD schools, especially more research-intensive ones, often emphasize:
- High academic metrics: GPA and MCAT
- Research experience: basic science, clinical, or translational research
- Strong letters from academic faculty or physicians, especially in academic medical centers
To strengthen an MD application:
- Aim for sustained research involvement, ideally with:
- A poster, abstract, or publication
- A strong letter from a principal investigator (PI)
- Craft your essays to show:
- Scientific curiosity
- Commitment to evidence-based medicine
- Capacity for rigorous academic work
Applying to Both DO and MD: Smart Strategy for Many Applicants
Many successful physicians applied to both DO and MD programs. Reasons to do this:
- Expands total number of possible acceptances
- Helps manage risk if:
- Your MCAT or GPA are borderline for MD
- You are a nontraditional applicant
- Allows you to compare curriculum, culture, and geographic fit across a wider range of schools
Actionable steps:
- Construct a balanced school list:
- “Reach,” “target,” and “safety” programs across both DO and MD.
- Customize:
- Avoid generic essays—specifically reference osteopathic philosophy for DO schools and institutional missions for MD schools.
- Plan letters:
- If possible, secure at least one letter from a DO and one from an MD or academic researcher.
Inside Medical School: Comparing DO and MD Training Experiences
Once you’re admitted, the day-to-day experience of DO vs MD students is more similar than different—but there are meaningful distinctions that can shape your skills and career focus.
Years 1–2: Preclinical Curriculum
DO Medical School Overview
- Basic sciences: Anatomy, physiology, biochemistry, pathology, pharmacology—similar in depth to MD programs.
- Osteopathic Manipulative Medicine (OMM):
- Required OMM labs and courses
- Hands-on training in palpation, musculoskeletal assessment, and OMT techniques
- Holistic and primary care emphasis:
- Early exposure to patient interviews
- Emphasis on social determinants of health, preventive care, and longitudinal relationships
Example:
In a DO anatomy lab, you might discuss not only the structure of the spine but also how dysfunction in certain vertebral segments can affect autonomic nervous system output to organs—and how OMT might help in specific clinical scenarios (e.g., asthma, constipation, headaches).
MD Medical School Overview
- Basic sciences: Same core sciences, often delivered in organ-system–based blocks.
- Early clinical exposure:
- Standardized patient encounters
- Simulation labs
- Interprofessional education
- Specialty awareness:
- Student interest groups (e.g., surgery, radiology, oncology)
- Opportunities to shadow or assist in specialty clinics
- Often stronger integration with research opportunities and academic departments
Example:
In an MD cardiology block, you might engage heavily with ECG interpretation, pharmacologic management of heart failure, and current clinical trials on new cardiac medications.
Years 3–4: Clinical Rotations and Electives
Both DO and MD students complete core clinical clerkships in:
- Internal Medicine
- Surgery
- Pediatrics
- Obstetrics & Gynecology
- Psychiatry
- Family Medicine
- Additional required or elective rotations (e.g., emergency medicine, neurology)
Key differences often include:
DO Students:
- Continue to practice and sometimes apply OMT in clinical settings (depending on site and preceptor).
- May rotate through more community-based hospitals or clinics, particularly in primary care–heavy regions.
- Often have an explicit focus on serving rural or underserved populations.
MD Students:
- More likely to rotate at large academic medical centers with tertiary and quaternary care.
- Often greater exposure to highly specialized services (e.g., transplant, complex oncology, advanced surgical subspecialties).
- Research electives in advanced specialties may be more accessible in some MD programs.
Actionable tip:
Whatever your degree, strategically choose 4th-year electives and away rotations in the specialties and institutions where you aim to match for residency.
Residency Matching and Beyond: DO vs MD in Graduate Medical Education
Residency Matching is where many premeds worry that DO vs MD will “make or break” their future. The reality is more nuanced—and more optimistic—than many online myths suggest.

The Modern Match: Single Accreditation System
Historically, there were separate accreditation systems and separate Matches for DO and MD residencies. As of 2020:
- The ACGME (Accreditation Council for Graduate Medical Education) oversees a single accreditation system.
- Both DO and MD graduates apply to the same residencies through the National Resident Matching Program (NRMP).
- Many programs are now explicitly “DO-friendly” and some have required OMT training components.
Applying to Residency as a DO vs MD Graduate
Both DO and MD applicants:
- Take USMLE exams (Step 1, Step 2 CK) if applying broadly to ACGME programs
- DO graduates also take COMLEX-USA exams (Level 1, Level 2 CE; Level 3 during residency)
- Use the Electronic Residency Application Service (ERAS) to apply
- Participate in the NRMP Match and, if necessary, the Supplemental Offer and Acceptance Program (SOAP)
Key nuances:
- Some competitive specialties and certain high-profile academic programs may still prefer or be more accustomed to MD candidates, especially in plastic surgery, dermatology, neurosurgery, and some orthopedic programs.
- Many community and academic programs in a broad range of specialties actively welcome DO applicants and have DO faculty.
Actionable tips for DO applicants interested in competitive specialties:
- Take USMLE Step exams in addition to COMLEX if your target programs expect them.
- Aim for above-average scores and honors in core clerkships.
- Seek research, away rotations, and strong letters of recommendation from faculty in your chosen specialty.
- Use your osteopathic background as a strength (e.g., “I bring a strong musculoskeletal and holistic perspective to orthopedic surgery”).
Fellowship Opportunities for DO and MD Physicians
After residency, both DO and MD physicians can pursue subspecialty training in fellowships, such as:
- Cardiology
- Gastroenterology
- Hematology/Oncology
- Critical Care
- Sports Medicine
- Pain Medicine
- Many others
Fellowship programs evaluate candidates primarily based on:
- Residency performance
- Board exam scores
- Research and scholarly work
- Letters of recommendation
- Fit with the program
Degree (DO vs MD) is generally far less important than your track record during residency.
Real-World Practice: Life as a DO vs MD Physician
By the time you’re practicing independently, day-to-day life as a DO or MD is more similar than different.
Practice Settings for DO and MD Physicians
Both DO and MD physicians practice in:
- Academic medical centers
- Community hospitals
- Private practices and group practices
- Federally qualified health centers and VA systems
- Telemedicine platforms
- Industry (pharmaceuticals, biotech, health tech)
- Public health and policy roles
Licensure and board certification requirements are nearly identical:
- Pass required licensing exams (USMLE or COMLEX)
- Complete accredited residency training
- Achieve board certification in your specialty through ABMS (for MDs and DOs) or AOA boards (for DOs)
Where DO Training May Stand Out in Practice
Many DO physicians incorporate:
- OMT into primary care, sports medicine, pain management, or certain specialty practices
- More frequent attention to musculoskeletal complaints that might otherwise be referred out quickly
- A strong emphasis on counseling for lifestyle modification (nutrition, exercise, stress, sleep)
Some DOs practice almost indistinguishably from MDs, never using OMT in daily practice. Others heavily integrate OMT and osteopathic principles, especially in family medicine, internal medicine, and sports medicine practices.
Where MD Training May Stand Out in Practice
Many MD physicians:
- Work in highly subspecialized academic fields or tertiary care centers
- Maintain strong involvement in clinical research, trials, and guideline development
- Take on leadership roles in academic departments, though DO representation is increasing steadily
Ultimately, your specialty, residency, mentors, and professional choices influence your practice far more than the initials after your name.
Key Takeaways for Premeds and Early Medical Students
- Both DO and MD paths lead to full physician status. You can become a surgeon, internist, psychiatrist, or cardiologist with either degree.
- Philosophical differences exist—but training overlap is large. DO emphasizes holistic, osteopathic principles and OMT; MD emphasizes traditional allopathic, disease-focused care. Both use evidence-based medicine.
- Residency Matching is unified. DO and MD applicants now use the same NRMP system; competitiveness depends more on metrics, performance, and experiences than the degree itself.
- Choose based on fit, not prestige myths. Consider:
- Your interest in primary care vs subspecialty focus
- Your appreciation for hands-on musculoskeletal work
- School culture, location, and curriculum style
- Your career will be defined more by your effort than your letters. Work ethic, curiosity, empathy, and professionalism matter at every step.

FAQs: DO vs MD from Application to Practice
1. Can a DO become a specialist or surgeon like an MD?
Yes. DO physicians can enter any major specialty, including:
- General surgery
- Orthopedic surgery
- Emergency medicine
- Dermatology
- Anesthesiology
- Radiology
- Psychiatry
- Cardiology and other subspecialties (via fellowship)
What matters most for competitive specialties is:
- Strong board scores (COMLEX, and often USMLE)
- Excellent clinical evaluations and letters
- Research and specialty-specific experience
- Strategic away rotations and networking
2. Do DOs and MDs work in the same hospitals and clinics?
Yes. DO and MD physicians frequently:
- Work side-by-side in the same departments, residency programs, and practices
- Share call schedules, leadership roles, and academic responsibilities
- See the same types of patients and perform the same procedures
Patients often do not distinguish between DO and MD; they care most about communication, competence, and outcomes.
3. Is it harder for DOs to match into residency than MDs?
It can be more challenging for DOs in certain highly competitive specialties and at some traditionally MD-dominant academic institutions. However:
- Many programs now have DO residents and faculty and are actively DO-friendly.
- DOs match into a wide array of specialties, including competitive ones, every year.
- Strong exam scores, solid clinical performance, and focused preparation can significantly level the playing field.
If you’re DO and aiming high:
- Take USMLE Step exams if recommended by your advisors.
- Target DO-friendly and historically DO-inclusive programs.
- Seek mentorship from DOs and MDs in your desired field.
4. What are the unique advantages of choosing a DO program?
Distinctive potential advantages include:
- Training in OMT, giving you additional non-pharmacologic tools for managing pain, musculoskeletal issues, and certain functional complaints.
- Strong culture of holistic, patient-centered care and prevention.
- Historically greater openness to nontraditional applicants or those with slightly lower metrics but strong experiences and service.
- Many DO schools have a mission focus on primary care and underserved communities, aligning well with students passionate about those areas.
5. Is one path better for getting into medical school or building a career?
Neither DO nor MD is universally “better”; both can support an outstanding career in medicine. The “best” path depends on:
- Your competitiveness as an applicant (GPA, MCAT, experiences)
- Your interest in osteopathic philosophy and OMT
- Your career goals (e.g., primary care vs highly competitive subspecialty)
- Geographic and cultural fit with specific schools
For many applicants, the most effective strategy is to apply thoughtfully to both DO and MD programs, then choose the school that offers the best overall fit—curriculum, culture, support, and alignment with your long-term goals.
Whether you choose Osteopathic Medicine or allopathic medicine, your success will come from consistent effort, openness to feedback, and a genuine commitment to patient care. DO vs MD is the first of many crossroads in your Medical Education—choose based on who you are now, and who you want to become as a physician.




















