
Introduction: DO vs MD and What “Rewarding” Really Means
Choosing a career in medicine is one of the most significant decisions you’ll make—and choosing between a Doctor of Osteopathic Medicine (DO) and a Doctor of Medicine (MD) pathway is often one of the first big forks in the road. Both routes lead to becoming a fully licensed physician, but they differ in philosophy, training emphasis, and sometimes in how others perceive them.
When premeds ask, “Is becoming a DO as rewarding as an MD?” they’re usually thinking about:
- Career satisfaction and fulfillment
- Lifestyle and work–life balance
- Competitiveness for residency and specialties
- Long‑term income and stability
- How their training aligns with their values, especially around holistic medicine
The reality: both DO and MD graduates can build highly rewarding medical careers. The “better” path depends far more on your goals, learning style, and values than on the letters after your name.
This guide breaks down the pros and cons of DO vs MD, clarifies how training and opportunities compare, and gives you practical advice for deciding which path might be more rewarding for you.
DO vs MD: Core Differences in Training and Philosophy
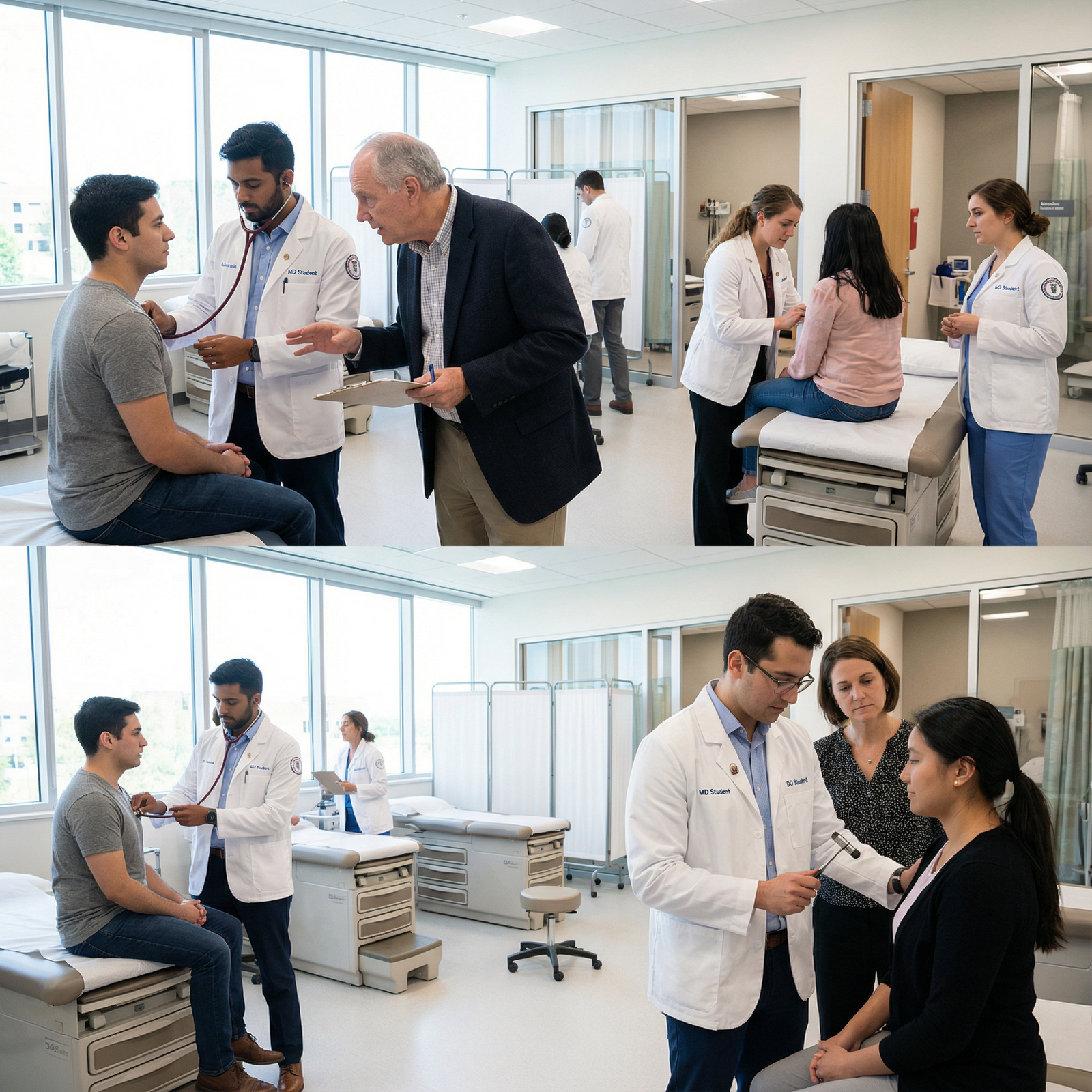
Understanding the distinctions between DO and MD starts with philosophy and education. Both are rigorously trained physicians, but they are shaped by slightly different frameworks.
What Is a DO (Doctor of Osteopathic Medicine)?
DO programs are built on osteopathic principles, which emphasize:
- Holistic medicine and whole-person care – treating body, mind, and spirit, and understanding how lifestyle, environment, and psychosocial factors affect health.
- The body as an interconnected unit – structure and function are interrelated.
- Inherent self-healing capacity – supporting the body’s natural tendency toward health.
- Preventive care – prioritizing prevention and wellness, not just treatment.
Key features of osteopathic medical education:
Osteopathic Manipulative Treatment (OMT):
DO students receive 200–300+ additional hours in manual diagnosis and treatment techniques. These hands-on skills can help diagnose and treat musculoskeletal problems, headaches, some types of pain, and complement traditional medical care.Curriculum:
DO schools cover the same core biomedical sciences and clinical rotations as MD schools: anatomy, physiology, pharmacology, surgery, internal medicine, pediatrics, OB/GYN, psychiatry, etc. The difference is in the added osteopathic content and emphasis on holistic, patient-centered care.Licensing exams:
DO students take the COMLEX-USA exam series. Many also choose to take the USMLE to maximize residency options.
What Is an MD (Doctor of Medicine)?
MD programs are historically the traditional allopathic route in the U.S. and globally. Their framework emphasizes:
- Disease-focused, evidence-based care – identifying pathology and targeting it with medications, procedures, and surgery.
- Scientific and research-focused training – strong emphasis on biomedical research and clinical trials.
- Diagnostic reasoning and management – often structured around organ systems and disease categories.
Key features of allopathic medical education:
Curriculum:
MD schools cover the same core sciences and clinical rotations as DO schools, generally without formal training in OMT or explicit osteopathic principles.Licensing exams:
MD students take the USMLE Step 1, 2, and 3, which are widely recognized in the U.S. and abroad.
Training Parity: More Similar Than Different
Both DO and MD physicians:
- Complete 4 years of medical school
- Match into ACGME-accredited residency programs (since the 2020 single accreditation merger)
- Are fully licensed physicians in all 50 U.S. states
- Can prescribe medications, perform surgeries, and practice in any specialty, given appropriate residency/fellowship training
From a patient’s perspective, the day-to-day difference between a DO and an MD often comes down to individual physician style and whether the DO uses OMT, rather than radically different capabilities.
The Pros of Becoming a DO: Holistic Medicine and Growing Opportunity
For many students, the DO pathway feels more aligned with how they want to practice medicine. Here are the main advantages of choosing osteopathic medical education.
1. Holistic Care and Patient-Centered Philosophy
If you value seeing patients as whole people rather than as “problems to fix,” osteopathic training may resonate strongly:
- Emphasis on lifestyle, psychosocial factors, and prevention
- Frequent training in motivational interviewing, communication, and patient education
- A framework that encourages asking:
- What’s driving this illness?
- How does this affect the patient’s life, family, work, and mental health?
- How can we prevent recurrence?
This can lead to:
- High career satisfaction for physicians who want deeper relationships with patients
- Strong fit for primary care, sports medicine, and fields where lifestyle and function matter (e.g., PM&R)
2. OMT: A Unique Clinical Skill Set
Osteopathic Manipulative Treatment offers:
- Non-pharmacologic options for pain and musculoskeletal complaints
- Adjunctive treatment for headaches, back pain, some respiratory conditions, and pregnancy-related discomfort
- A differentiator in competitive markets, especially in family medicine, sports medicine, or rural practice
Example:
A DO family physician might use OMT to help a patient with chronic low back pain, alongside exercise prescriptions and medication, potentially reducing long-term dependency on opioids or invasive procedures.
You don’t have to use OMT in your career, but having the option can be rewarding—both clinically and professionally.
3. Strong Representation in Primary Care and Underserved Areas
DO programs traditionally emphasize:
- Family medicine, internal medicine, pediatrics, and OB/GYN
- Service to rural and underserved communities
This often translates into:
- High demand and job stability in primary care settings
- Opportunities to build long-term patient relationships and see tangible impact on communities
- Loan repayment options through federal and state programs that favor primary care in shortage areas
If your vision of a fulfilling medical career includes being a community doctor, DO training is often particularly well aligned.
4. Supportive, Close-Knit Professional Community
The osteopathic profession is:
- Smaller and more tight-knit than the MD community
- Often marked by strong mentorship networks and alumni connections
- Known for a culture that embraces collaboration, humility, and service
Many DO students and physicians report that this sense of community contributes to career satisfaction and resilience, especially during challenging training years.
5. Growing Recognition and Opportunities
Over the past several decades:
- DOs have become increasingly integrated into major academic centers, competitive residencies, and subspecialties.
- Many program directors now have DO faculty or residents and are more familiar with osteopathic training.
- The single accreditation system for residencies means DOs and MDs now apply to the same ACGME programs.
The result:
While some bias persists in specific niches, the overall recognition and acceptance of DOs is higher than ever and continues to grow.
The Cons of Becoming a DO: Perception, Exams, and Specialty Competition
Despite the many benefits, the DO pathway does come with challenges that you should weigh carefully.
1. Lingering Perception and Bias in Certain Contexts
Although legally equal, DOs can still face:
- Misconceptions among patients: Some assume DOs are “less than” MDs or confuse them with chiropractors or naturopaths.
- Variable exposure among physicians and program directors: In highly competitive, research-heavy specialties (e.g., dermatology, plastic surgery, neurosurgery), some programs may still favor MD applicants, partly due to tradition and familiarity.
Mitigation strategies:
- Take the USMLE in addition to COMLEX to make your application easier to compare.
- Engage in research, strong clinical performance, and mentorship to demonstrate excellence beyond your degree type.
- Choose DO schools with robust match outcomes and specialty pipelines if you’re aiming for competitive fields.
2. Relative Disadvantages in Some Competitive Specialties
DOs can and do match into every specialty, including:
- Dermatology
- Orthopedic surgery
- Neurosurgery
- Plastic surgery
However:
- Overall match rates into these ultra-competitive fields may be lower for DOs compared to MDs.
- Some programs may rarely take DOs, regardless of how strong your application is.
This doesn’t make it impossible—but it does mean:
- You’ll need top-tier board scores (COMLEX and USMLE), strong letters, and significant research.
- You might need to be more flexible geographically or consider a slightly different specialty if doors remain closed.
3. Dual Licensing Exams Can Be Burdensome
Most DO students:
- Must take COMLEX Level 1, 2, and 3 for DO licensure
- Often also choose to take USMLE Step 1 and 2 to remain competitive across all residencies
This can mean:
- Increased exam prep burden
- More stress and financial cost
- A need for meticulous scheduling and time management
If you already know you want a less competitive specialty or plan to stay in DO-friendly fields, you might skip USMLE—but many students prefer to keep doors open.
The Pros of Becoming an MD: Tradition, Networks, and Global Recognition
The MD route remains the most common pathway in U.S. medical education and has its own clear advantages.
1. Broad Specialty Access and Established Networks
Because MDs historically outnumber DOs:
- Academic departments and specialty societies are often MD-dominated.
- Many highly competitive residencies are built around MD pipelines.
Advantages often include:
- Stronger institutional networks in research-heavy fields (e.g., academic cardiology, oncology, surgical subspecialties).
- More mentors and role models in rarer specialties (e.g., pediatric neurosurgery).
For students aspiring to intensely competitive specialties, an MD pathway can be logistically smoother, though still far from guaranteed.
2. Traditional Prestige and Public Recognition
For better or worse, many people still:
- Recognize “MD” instantly as “physician”
- Associate MD with prestige and status
This can translate into:
- Fewer patient questions about your degree
- Slightly easier navigation of non-medical arenas (media, business ventures, consulting, global work), where MD is more universally understood
3. Single Exam Pathway with Global Portability
MD students take only the USMLE series, which offers:
- Streamlined exam scheduling
- Fewer test fees and less duplicated content
- Widely recognized credentials in international medical careers, research, and fellowships
If you’re considering practicing abroad or doing global work long-term, an MD may be marginally simpler from a licensing standpoint (though DOs can also work internationally in many countries).
4. Abundant Residency and Fellowship Role Models
Because MD physicians are more numerous:
- It may be easier to find mentors in niche subspecialties.
- Many major academic centers are historically MD institutions with established research infrastructure and mentorship systems.
This doesn’t make DOs less capable; it simply reflects the current composition of the physician workforce.
The Cons of Becoming an MD: Pressure, Competition, and Burnout Risk
The MD route also has downsides that matter for long-term career satisfaction.
1. Less Formal Emphasis on Holistic Care
While many MD schools now emphasize communication and patient-centered care, the traditional MD curriculum:
- May place more weight on pathology and interventions
- May devote less formal time to lifestyle medicine, psychosocial determinants of health, or hands-on body mechanics
You can absolutely be a holistic MD, but:
- You may need to seek extra training in areas like integrative medicine, lifestyle medicine, or mind–body approaches if those matter to you.
2. Intense Competition and Culture of Performance
The MD track can be:
- Highly competitive for admission
- Focused on grades, test scores, publication count, and ranking
This culture sometimes leads to:
- High stress and anxiety among students
- Imposter syndrome in high-achieving cohorts
- A focus on external validation (class rank, exam percentiles) over intrinsic reward and meaning
If not managed, this can impact mental health and well-being, even before residency.
3. Strong Pull Toward Specialization
The MD environment often:
- Emphasizes specialized, hospital-based careers
- Subtly or overtly undervalues primary care roles
Consequences:
- Some students who might have enjoyed primary care feel pressured toward fields they don’t truly enjoy.
- Persistent primary care shortages and burnout in hospital-based specialties.
If your ideal practice is community-based primary care, you may need to be deliberate about resisting this pressure and staying true to your goals.
4. Burnout Risk and Lifestyle Challenges
Both DO and MD physicians face significant burnout risks, but within MD training environments, factors may include:
- Competitive culture
- High clinical volume and long hours in certain specialties
- Identity strongly tied to academic or career success
Building a rewarding career as an MD requires intentional boundary-setting, self-care, and career design, especially in demanding fields.
Real-World Considerations: Career Satisfaction, Lifestyle, and Finances
Beyond philosophy and training, you should think about how each pathway fits your long-term life and goals.
Career Satisfaction: What Actually Matters in the End?
Research and physician surveys consistently show that career satisfaction is driven more by:
- Specialty choice and practice setting
- Control over schedule and workload
- Quality of team and leadership
- Alignment between values and day-to-day work
…than by DO vs MD.
For example:
- A DO in family medicine in a supportive group practice may be far more satisfied than an MD in a toxic surgical residency—and vice versa.
- Many DOs find profound fulfillment in long-term patient relationships, preventive care, and community impact.
- Many MDs find their calling in academic medicine, cutting-edge research, or procedural specialties.
Key takeaway:
Your fit with specialty and practice environment will likely matter much more for career satisfaction than whether you are DO or MD.
Lifestyle and Work–Life Balance
Lifestyle is less about degree and more about:
- Specialty (e.g., dermatology vs trauma surgery)
- Practice type (academic vs private vs employed)
- Call schedule and clinic structure
That said, trends exist:
- DOs, with their strong representation in primary care, may more often pursue outpatient-focused careers, which can support balanced lifestyles.
- MDs are more common in some high-intensity fields that historically have more challenging hours.
However, a DO anesthesiologist and an MD anesthesiologist in the same practice will have very similar lifestyles. Your degree doesn’t dictate your schedule—your specialty and job contract do.
Financial Considerations and Debt
Factors affecting income:
- Specialty (e.g., orthopedic surgery vs pediatrics)
- Geographic region (urban vs rural, high vs low cost of living)
- Practice model (academic vs private vs corporate-employed)
Historically, MDs had slightly higher odds of entering top-paying subspecialties. As DOs increasingly match into these fields, the income gap has narrowed.
Key financial points:
- Both DO and MD students often graduate with substantial debt.
- Primary care specialties (common among DOs) generally pay less than surgical subspecialties, but:
- Often have more lifestyle flexibility
- May qualify for loan forgiveness programs more frequently
Your long-term financial picture will reflect your specialty, practice choices, and financial habits far more than whether you chose DO vs MD.
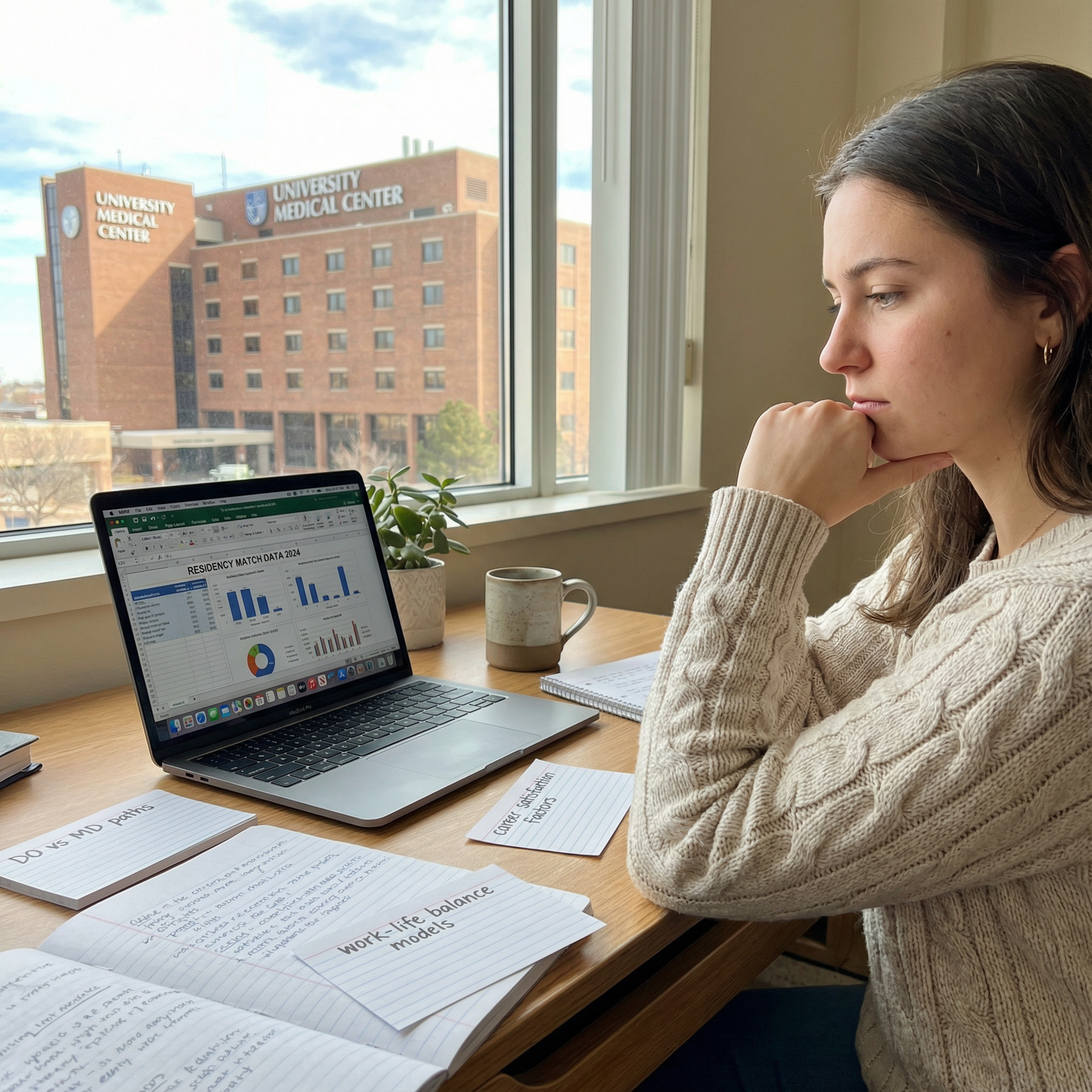
How to Decide: Choosing the Path That’s Most Rewarding for You
When you strip away the noise, the DO vs MD decision is about fit.
Reflect on Your Values and Vision of Medicine
Ask yourself:
- How important is holistic medicine and mind–body integration in how I want to practice?
- Am I drawn to primary care and long-term patient relationships, or do I lean toward highly specialized, procedure-heavy fields?
- Do I want the option to use hands-on techniques (OMT), or is that less interesting to me?
If you strongly resonate with whole-person care and may want to practice in primary care or sports medicine, DO can feel particularly rewarding. If you’re laser-focused on a very competitive surgical field and academic medicine, the MD route may offer some structural advantages.
Consider Your Tolerance for Extra Exams and Advocacy
If you choose DO:
- Are you prepared to likely take both COMLEX and USMLE?
- Are you comfortable occasionally explaining your degree to patients or colleagues?
If yes, and you like the osteopathic philosophy, the DO pathway can be an excellent fit.
Research Specific Schools and Outcomes
Not all DO or MD programs are identical. For each school you’re considering:
- Review match lists: Where do graduates go? What specialties?
- Look at board score averages and support for exam prep.
- Check for advising and mentorship infrastructure, especially if you’re aiming at competitive specialties.
- Talk to current students and recent graduates about their experiences.
Choose the individual school that best supports your goals—sometimes a strong DO program may serve you better than a weaker MD program, and vice versa.
Plan for Flexibility
Many students change their minds about specialties during training. To keep doors open:
- Focus on academic excellence wherever you go.
- Engage in research, leadership, and meaningful clinical experiences.
- Build strong relationships with mentors who can advocate for you.
Ultimately, your performance, professionalism, and passion will matter more than DO vs MD.
FAQs: DO vs MD, Holistic Medicine, and Career Satisfaction
1. Can DOs and MDs practice the same medical specialties?
Yes. Both DOs and MDs can enter any specialty—family medicine, surgery, dermatology, cardiology, anesthesiology, etc.—as long as they complete the appropriate residency and fellowship training. However, match rates and competitiveness can differ: some hyper-competitive specialties and programs may historically favor MD applicants. Strong board scores, research, and mentorship are crucial for DOs aiming at these fields.
2. Are DOs and MDs equally respected in the medical field?
Legally, DOs and MDs have the same practice rights in the U.S., and many institutions treat them equivalently. In day-to-day hospital practice, colleagues often judge you more by your competence and teamwork than by your degree. That said, some residual bias and misunderstanding remain, particularly in certain competitive academic environments or in regions less familiar with DOs. This trend is steadily improving as more DOs enter academic medicine and specialty fields.
3. How should I decide between applying to DO vs MD schools as a premed?
Consider:
- How strongly you connect with holistic medicine and OMT
- Your current interest in primary care vs highly competitive subspecialties
- Your willingness to take both COMLEX and USMLE
- The match outcomes and resources of specific schools
Many premeds apply to both DO and MD schools to maximize options, then choose the school that best fits their learning style, values, and long-term goals.
4. Is the quality of education different between DO and MD schools?
Both DO and MD programs are rigorously accredited and must meet high educational standards. You will study the same core sciences and complete similar clinical rotations. The main differences are:
- DO programs add OMT and osteopathic principles
- Individual schools (DO or MD) may vary in research opportunities, reputation, board performance, and match strength
When evaluating “quality,” compare specific schools, not DO vs MD in the abstract.
5. Which degree leads to better work–life balance and less burnout: DO or MD?
Neither degree guarantees balance or protects you from burnout. Work–life balance is driven by:
- Specialty choice (e.g., radiology vs general surgery)
- Practice type and culture
- Your ability to set boundaries and prioritize well-being
Because DOs are more represented in primary care, some DO physicians may have more outpatient-focused, controllable schedules. But an MD in outpatient pediatrics and a DO in outpatient pediatrics can have nearly identical lifestyles. Focus on specialty, practice setting, and personal boundaries rather than assuming one degree is “easier” than the other.
Choosing between DO and MD is not about which path is objectively more rewarding—it’s about which path better matches who you are and the kind of physician you hope to become. If you align your training with your values, stay open to growth, and prioritize both patient care and your own well-being, you can build a deeply fulfilling medical career from either starting point.




















