
DO vs. MD: What You Need to Know About the Differences
Choosing between a Doctor of Osteopathic Medicine (DO) and a Doctor of Medicine (MD) is one of the earliest major decisions in your journey toward becoming a physician. Both are fully licensed doctors in the United States, both complete rigorous training, and both can pursue any specialty—from family medicine to neurosurgery. Yet there are real differences in history, philosophy, training emphasis, and, in some cases, career trajectory.
Understanding these distinctions helps you:
- Clarify which path aligns better with your values and learning style
- Strategically plan your medical school applications
- Anticipate how your degree may influence residency and career opportunities
- Communicate clearly with patients and colleagues about your professional background
This guide walks through the key differences and similarities between DO vs MD in Medical Degrees, from educational pathways and licensing to philosophy, practice patterns, and evolving trends in Healthcare Education.
Overview of Medical Degrees: MD and DO in the U.S.
What Is an MD? (Allopathic Medicine)
The MD (Doctor of Medicine) is the older and more globally recognized medical degree. Rooted in European medical traditions, MD programs are often described as training in Allopathic Medicine—a system that treats disease primarily through drugs, surgery, and other interventions based on modern biomedical science.
Key Characteristics of MD Training and Practice:
- Centered on evidence-based medicine grounded in biomedical research
- Heavy use of pharmacologic therapies, procedures, and surgery
- Strong emphasis on diagnostic reasoning, imaging, and lab interpretation
- Widely recognized internationally, which can be important if you plan to practice outside the U.S.
In practice, today’s MD training also incorporates prevention, public health, and psychosocial aspects of care. The historical allopathic vs osteopathic divide has blurred considerably—but there are still some philosophical distinctions.
What Is a DO? (Osteopathic Medicine)
The DO (Doctor of Osteopathic Medicine) originates from the late 19th century, founded by Andrew Taylor Still. Dissatisfied with the limited and sometimes harmful treatments of his time, he developed Osteopathic Medicine, emphasizing the body’s inherent ability to heal itself, the interconnectedness of structure and function, and the importance of holistic care.
Key Characteristics of DO Training and Practice:
- Focus on holistic, patient-centered care, addressing mind, body, and environment
- Specific attention to the musculoskeletal system and biomechanics
- Training in Osteopathic Manipulative Treatment (OMT/OMM)—hands-on techniques to diagnose and treat dysfunction
- Historically strong orientation toward primary care, though DOs now pursue all specialties
Importantly, modern osteopathic schools also heavily emphasize evidence-based medicine and standard biomedical science, just like MD schools. The difference is more about added training and philosophical framing than a completely separate system.
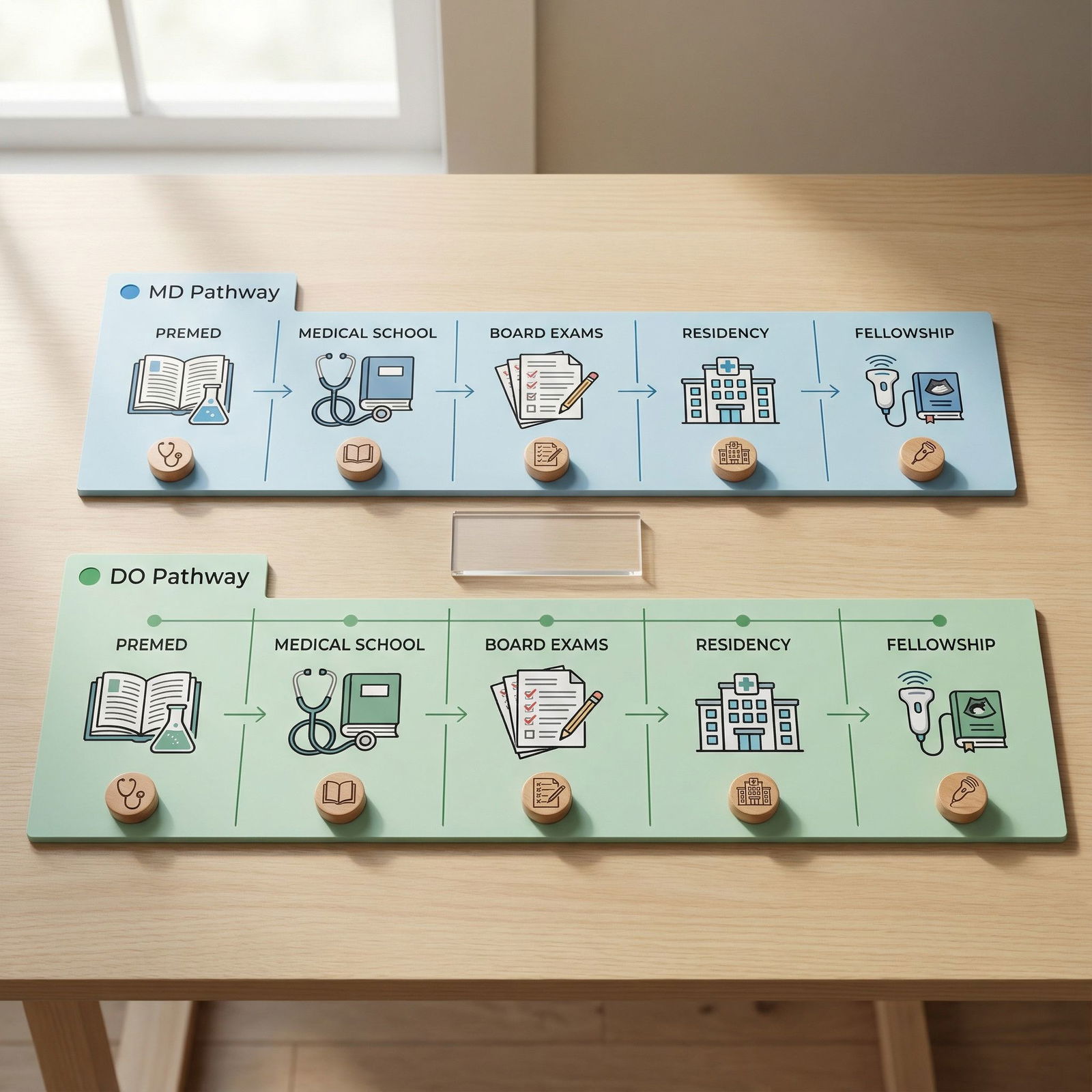
Educational Pathways: How DO vs MD Training Compares
At a high level, the educational timeline for DO and MD students in the U.S. is remarkably similar. Both are rigorous paths in Healthcare Education that require significant academic preparation, resilience, and commitment.
1. Premedical Preparation
Undergraduate Education (or Equivalent):
- Both DO and MD applicants typically complete a bachelor’s degree in the U.S. or equivalent credentials abroad.
- Common majors: biology, chemistry, neuroscience, psychology—but any major is acceptable as long as prerequisites are met.
Core Prerequisites (for most schools):
- General biology with lab
- General and organic chemistry with lab
- Physics
- Biochemistry
- English/writing
- Statistics and/or psychology (varies by school)
Standardized Test: The MCAT
- Almost all MD and DO programs require the MCAT.
- Historically, some DO programs were more forgiving of slightly lower MCAT scores, but this is changing; competitiveness has risen significantly.
Application Services:
- MD programs: primarily via AMCAS
- DO programs: via AACOMAS
- Many applicants apply to both MD and DO schools to maximize options.
2. Medical School Curriculum: MD vs DO
Both MD and DO programs are generally four years in length and follow a similar structure:
Preclinical Years (Years 1–2)
For Both MD and DO Students:
- Intensive classroom and small-group learning in:
- Anatomy, histology, physiology
- Biochemistry, genetics, pharmacology
- Pathology, microbiology, immunology
- Behavioral sciences and ethics
- Increasing use of case-based and team-based learning
- Early clinical exposure and standardized patient encounters
Unique Aspect for DO Students: Osteopathic Manipulative Treatment (OMT)
- DO programs add required coursework and lab time in:
- Osteopathic principles and philosophy
- Hands-on palpation skills
- OMT techniques (e.g., muscle energy, HVLA, soft tissue, myofascial release)
- This can amount to hundreds of additional hours of musculoskeletal and manual medicine training across the curriculum.
Clinical Years (Years 3–4)
Both MD and DO students complete core clinical clerkships in:
- Internal medicine
- Surgery
- Pediatrics
- Obstetrics and gynecology
- Psychiatry
- Family medicine
- Neurology and/or emergency medicine (depending on school)
During these years, you’ll:
- Work directly with patients under supervision
- Develop clinical reasoning, procedural skills, and professional identity
- Take on elective rotations tailored to your specialty interests
- Build the clinical evaluations and letters of recommendation needed for residency
In many hospitals and clinics, MD and DO students rotate side-by-side, following virtually identical expectations and evaluations.
3. Board Exams: USMLE vs COMLEX
A key difference between DO and MD training lies in board examinations:
For MD Students:
- Must take the USMLE series:
- Step 1: basic sciences and pathophysiology
- Step 2 CK: clinical knowledge
- Step 3: taken during residency for full licensure
For DO Students:
- Must take the COMLEX-USA series:
- Level 1: basic science and osteopathic principles
- Level 2-CE: clinical knowledge
- Level 3: during residency
Many DO students also choose to take the USMLE exams in addition to COMLEX, particularly if they:
- Aim for highly competitive specialties or programs
- Want to ensure direct comparability with MD applicants
Program directors are increasingly familiar with COMLEX, but having both score sets can still be advantageous in some settings.
4. Residency Training in the Single Accreditation Era
Previously, MDs and DOs had separate residency accreditation systems (ACGME for MD, AOA for DO). As of 2020, all residency programs are under a single ACGME accreditation system, meaning:
- DO and MD graduates apply to the same specialties through the National Resident Matching Program (NRMP).
- DO graduates can match into any ACGME-accredited residency, including historically “MD-dominated” specialties.
- Some programs may remain more familiar with one set of board exams or one type of degree, but structurally, the doors are now open to both.
After residency, both DO and MD physicians can pursue fellowship training, board certification in subspecialties, and academic careers.
Philosophical and Clinical Differences: How MD and DO Approaches Vary
Although the day-to-day practice of many DOs and MDs looks similar—especially in hospital and specialty settings—the underlying philosophies still influence training and patient care.
Allopathic Medicine (MD): Disease-Oriented, Intervention-Focused
In traditional Allopathic Medicine, the focus starts with identifying a specific pathology and then applying targeted therapies to correct it.
Typical emphases:
- Identifying disease using labs, imaging, and specialized tests
- Using medications, procedures, and surgeries to treat pathology
- Applying evidence-based guidelines derived from clinical research
- Focusing on outcomes such as survival, symptom control, and quality-of-life measures
Modern MD curricula do integrate preventive care, lifestyle counseling, and psychosocial aspects, but the vantage point often begins with the disease process.
Osteopathic Medicine (DO): Holistic, System-Oriented
Osteopathic Medicine shares the same scientific foundation as allopathic medicine, but it adds a layer of guiding principles:
Core osteopathic tenets:
- The body is a unit; the person is a unity of body, mind, and spirit.
- The body is capable of self-regulation, self-healing, and health maintenance.
- Structure and function are reciprocally interrelated.
- Rational treatment is based upon these principles.
Practically, this can translate to:
- More attention to biomechanics and posture, especially in musculoskeletal complaints
- Integrating OMT to improve mobility, relieve pain, or enhance physiologic function
- Placing strong emphasis on preventive care, lifestyle, and social determinants of health
- Spending more visit time on counseling and whole-person care (varies by practice setting)
Patient Experience: Does It Feel Different?
In real clinical environments, the distinctions often come down to the individual physician rather than the degree. However, on average:
DO Physicians
- More likely to practice in primary care (family medicine, internal medicine, pediatrics)
- Sometimes incorporate OMT alongside conventional treatments
- May emphasize lifestyle, function, and long-term relationship-based care
MD Physicians
- More represented in certain procedural and subspecialty fields (e.g., dermatology, some surgical subspecialties—though DO representation is growing)
- Often practice in academic tertiary centers, though many also serve in primary care
Many patients are unaware of the difference or do not distinguish between the two. Others seek out DOs specifically for a holistic approach or OMT services.
Practice Environments, Specialties, and Career Outcomes
DOs and MDs share equivalent practice rights in all 50 states, including:
- Full prescribing authority
- Ability to perform surgery and invasive procedures
- Eligibility for hospital privileges and academic appointments
- Access to all specialties and subspecialties, depending on training
Practice Settings
Both DO and MD physicians work in:
- Academic medical centers
- Community hospitals
- Private practices and group practices
- Federally Qualified Health Centers (FQHCs)
- Telemedicine and non-traditional care models
- Research institutions, leadership, policy, and industry roles
Your eventual practice environment will be shaped more by your specialty, training program, and career interests than by the letters after your name.
Specialization Trends
While there is increasing overlap, some trends still exist:
MDs More Commonly Seen In:
- Surgical subspecialties (e.g., neurosurgery, cardiothoracic surgery)
- Competitive fields (e.g., dermatology, plastic surgery, certain subspecialty fellowships)
- Academic research-intensive positions
DOs More Commonly Seen In:
- Family medicine
- Internal medicine and hospitalist medicine
- Pediatrics
- Some community-based and rural practices
That said, DOs now match into competitive specialties at growing rates. Your competitiveness will depend on:
- Board scores (USMLE and/or COMLEX)
- Clinical performance and letters of recommendation
- Research and scholarly activity
- Leadership, professionalism, and interview performance
The degree type is only one piece of this larger picture.
Acceptance, Recognition, and International Considerations
Public Perception and Professional Respect
Within the U.S. healthcare system, DOs and MDs are increasingly viewed as equivalent physicians:
- In most hospitals, DO and MD physicians work side-by-side with identical responsibilities.
- Many patients never notice or inquire about the distinction.
- Younger generations of physicians, program directors, and administrators are generally very familiar with osteopathic training.
Remaining misconceptions:
- Some people still mistakenly believe DOs are “less qualified” or akin to alternative practitioners. This is incorrect; DOs complete fully accredited medical school and residency training.
- Clarifying that DOs are licensed physicians—not chiropractors, naturopaths, or physical therapists—is sometimes necessary in patient conversations.
Licensing and Board Certification
Both DOs and MDs:
- Are licensed by state medical boards under similar statutes
- Must pass national board exams (USMLE and/or COMLEX)
- Can become board-certified in their specialties through recognized boards (e.g., American Board of Internal Medicine, American Osteopathic Boards, etc.)
International Practice
If you anticipate practicing outside the United States, the MD degree may be more straightforward in some countries, given its global familiarity. However:
- Many countries are becoming more aware of osteopathic physicians (DOs) from the U.S.
- Some locations distinguish between U.S.-trained DO physicians and non-physician osteopaths (manual therapists) from other countries.
- If international practice is a major career goal, research the regulations of your target country and consider discussing with advisors before choosing your path.
How to Choose Between DO and MD: Practical Advice for Applicants
Choosing between DO vs MD is less about which degree is “better” and more about which aligns with your goals, values, and competitiveness.
Reflect on Your Philosophy and Career Goals
Ask yourself:
- Do you strongly resonate with holistic, whole-person care, including body–mind–environment connections?
- Are you interested in hands-on musculoskeletal treatment (OMT) as part of your clinical toolkit?
- Are you drawn to primary care or community-based practice, even if you keep an open mind about specialties?
If yes, a DO program may feel like a strong philosophical fit.
On the other hand:
- Are you set on practicing internationally in regions where MD is more established?
- Are you primarily focused on research-intensive academic careers or highly competitive specialties?
- Do you prefer a more traditional allopathic framework and do not feel particularly drawn to OMT?
If so, pursuing an MD program may align better with your long-term vision.
Be Strategic About Competitiveness
In practice, many applicants apply to both MD and DO schools. Consider:
GPA and MCAT:
- MD schools, especially top-tier ones, tend to have higher average metrics.
- DO schools can be a strong option if your stats are slightly below MD medians but still solid.
Experiences and Fit:
- DO schools often value community service, primary care interest, and resilience.
- MD schools may especially value research and broader academic metrics, depending on the institution.
Ultimately, your personal statement, letters of recommendation, and interviews should express why each pathway makes sense for you.
Talk to Both DO and MD Physicians
Before deciding:
- Shadow both DO and MD doctors in various specialties.
- Ask them:
- How (if at all) their degree affects daily practice
- Whether they use OMT (for DOs) and how patients respond
- If their degree impacted residency chances or career progression
Real-world perspectives often demystify the DO vs MD debate more than online discussions alone.

FAQs About DO vs MD Medical Degrees
1. Are DOs and MDs both real doctors with the same rights?
Yes. In the United States, both DOs and MDs are fully licensed physicians. They:
- Complete accredited medical school programs
- Undergo residency and, if desired, fellowship training
- Can prescribe medications, perform surgeries, and admit patients to hospitals
- Are eligible for board certification and academic positions
The main differences lie in training emphasis and philosophy, not legal authority.
2. Can DOs and MDs enter the same specialties and residencies?
Yes. Under the unified ACGME accreditation system, DO and MD graduates apply to the same residency programs through the NRMP Match. DOs and MDs now train side-by-side in:
- Primary care (family medicine, internal medicine, pediatrics)
- Hospital-based specialties (emergency medicine, anesthesia, radiology)
- Surgical fields (general surgery, orthopedics, neurosurgery, etc.)
- Subspecialties (cardiology, oncology, GI, dermatology, etc.)
Competitiveness depends more on your academic record, board scores (USMLE/COMLEX), performance on rotations, and interviews than on whether you hold a DO or MD.
3. Do DOs always use Osteopathic Manipulative Treatment (OMT)?
Not always. While all DOs are trained in OMT during medical school:
- Some incorporate it regularly, especially in primary care, sports medicine, and certain specialty clinics.
- Others use it selectively or rarely, depending on their practice style, patient population, and time constraints.
- In high-acuity or surgical subspecialty environments, the opportunity for OMT may be limited.
If using OMT is important to you, seek mentors and residency programs that actively support its integration.
4. Is one degree (DO or MD) better for patients?
There is no strong evidence that either degree produces “better” doctors in a global sense. Outcomes vary based on:
- Individual physician skill, communication, and judgment
- Quality of residency and fellowship training
- Practice environment and resources
Some patients prefer DOs because of their holistic approach and the option of OMT; others prefer MDs due to familiarity with the degree. Many do not have a specific preference and value access, communication, and trust above all.
5. How should I decide which programs to apply to: DO, MD, or both?
Consider:
- Your academic profile (GPA, MCAT) relative to school medians
- Your interest in Osteopathic Medicine and holistic care
- Long-term goals: primary care vs subspecialty, U.S. vs international practice, research vs clinical focus
- Financial, geographic, and lifestyle factors
Many applicants build a balanced school list that includes both MD and DO programs. Discuss strategy with premed advisors, mentors, and current medical students to tailor an approach that matches your background and aspirations.
By understanding the nuances between DO vs MD degrees—training structure, philosophy, recognition, and practice trends—you can make a more informed, confident decision about your future in Healthcare Education. Whether you choose Osteopathic Medicine or Allopathic Medicine, your commitment to rigorous training and compassionate care will be the foundation of a fulfilling medical career.




















