
Understanding Red Flags in OB GYN Residency Applications for Non‑US Citizen IMGs
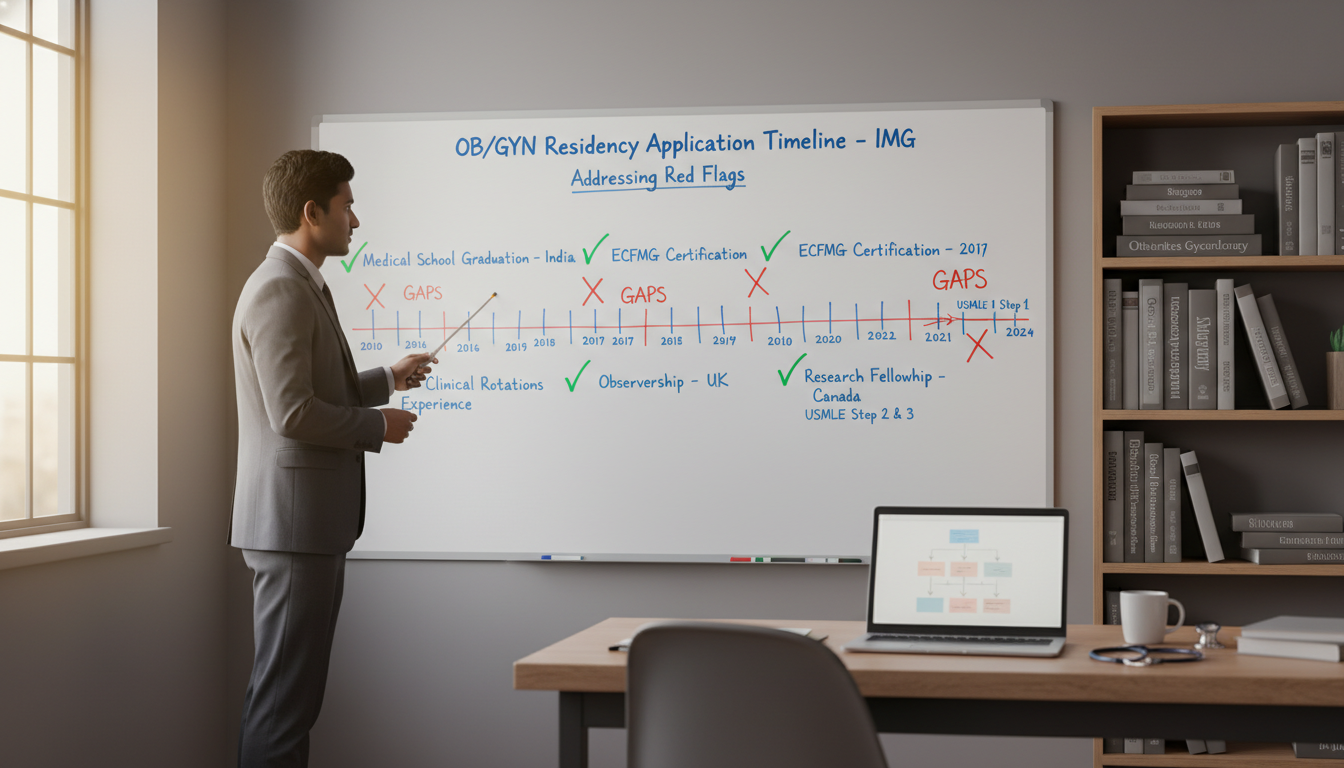
For a non-US citizen IMG (international medical graduate) applying to OB GYN residency, “red flags” can feel like permanent barriers: failed exams, gaps in training, low scores, visa issues, or professionalism concerns. In reality, most red flags can be mitigated—if you understand how programs interpret them and how to explain them strategically.
This article focuses on addressing red flags specifically for the non-US citizen IMG applying to an OB GYN residency in the U.S. You’ll learn how program directors think, how to frame your story, and how to rebuild your candidacy so that one problem does not define your entire obstetrics match journey.
How Program Directors View Red Flags in OB GYN
Residency programs are not only choosing strong applicants—they are also managing risk. A red flag signals potential risk to:
- Patient safety
- Board pass rates
- Team dynamics and professionalism
- Reliability and visa stability
For a foreign national medical graduate in particular, some issues (like visa needs) may automatically trigger closer scrutiny. Understanding this lens helps you plan how to address concerns proactively.
Common Red Flag Categories in OB GYN Applications
Below are categories of red flags especially relevant to OB GYN programs:
Academic Performance
- USMLE Step failures
- COMLEX/USMLE score outliers or very low scores
- Multiple exam attempts
- Repeated clerkships or academic probation
- Failed or marginal OB GYN rotations
Timeline & Training History
- Large gaps in medical education or clinical work
- Long time since graduation (YOG)
- Unfinished residencies or dismissed training
- Switching specialties without a clear explanation
Professionalism & Conduct
- Disciplinary actions, probations, or professionalism notes
- Remediation for behavior, communication, or ethics
- Negative comments in MSPE (Dean’s letter)
Application Red Flags
- Very few or weak letters of recommendation (especially no OB GYN letters)
- Inconsistent personal statement or CV
- Mismatched story (e.g., no OB GYN experiences but applying OB GYN)
- Poor interview performance, including unprepared answers about red flags
Visa & Immigration Concerns
- Need for J-1 or H-1B visa without strong scores or profile
- Unclear immigration history or status changes
- Prior visa denials or complex travel histories (if mentioned or implied)
For a non-US citizen IMG, some neutral characteristics become near-red-flags simply because they add risk or complexity, such as graduating >5–7 years ago, limited U.S. clinical experience, or no prior exposure to U.S. OB GYN systems.
How OB GYN Specifically Amplifies Certain Red Flags
OB GYN programs often prioritize:
- Board passage probabilities due to high-stakes surgical and obstetric care
- Team-based communication and professionalism in the OR, L&D, and clinic
- Reliability under stress—emergencies, night shifts, and high-acuity patients
Because of that:
- Failed exams raise concern about CREOG/board success.
- Professionalism issues raise concern about patient safety and liability.
- Gaps or fragmented training raise concern about stamina and consistency.
Your task is to show that what happened is understood, owned, and resolved—and that you are now low-risk and high-value.
Principles for Addressing Any Red Flag as a Non-US Citizen IMG
Regardless of your specific situation (failed exam, gap, professionalism issue), the framework to explain it is similar.
1. Be Honest, Brief, and Direct
Program directors can often see your red flag already:
- USMLE failures appear on the transcript.
- Gaps are visible on your CV timeline.
- Academic probation or professionalism issues may appear in your MSPE.
Trying to hide, minimize, or blame others creates a new, worse red flag: lack of integrity.
Guiding rule:
- One–two sentences to describe what happened
- Two–four sentences to describe what you learned and how you changed
You want clarity, not drama.
2. Shift Focus from Problem to Growth
Programs care less about the mistake and more about your trajectory after the mistake:
- Did you identify what went wrong?
- Did you use resources appropriately?
- Did your performance improve later?
- Are there objective signs of improvement (scores, evaluations, new responsibilities)?
You’re telling a before–during–after story:
- Before – circumstances or context (not excuses)
- During – the red flag event
- After – concrete, measurable growth
3. Take Full Ownership—Without Self-Sabotage
Use language such as:
- “I did not manage my time effectively…”
- “I underestimated the impact of…”
- “I delayed seeking help when I needed it…”
Avoid:
- Blaming others, the exam, or the system
- Emotional oversharing that makes you seem unstable
- Over-justifying with long stories
You are a future OB GYN attending speaking about a past challenge professionally and concisely.
4. Provide Objective Evidence of Improvement
For each red flag, think: What concrete evidence can I present that this is resolved?
Examples:
- After a failed Step 1 → higher Step 2 score, strong NBME or shelf exams, letters mentioning “excellent medical knowledge.”
- After a professionalism incident → continuity of stable work, leadership roles, strong comments about teamwork and communication.
- After a gap → documented clinical or academic activity (research, observerships, teaching, public health work).
Words are important, but evidence convinces.
5. Keep the Story Consistent Everywhere
Your explanation must be aligned across:
- ERAS application
- Personal statement
- Interviews
- Any emails/communications
Inconsistencies trigger suspicion. Decide on a clear, truthful version and stick to it.
Academic Red Flags: Failures, Low Scores, and How to Explain Them
Academic issues are among the most visible red flags in an OB GYN residency application and often feel fatal to applicants. They are not automatically fatal—especially if the rest of your profile is strong and your explanations are thoughtful.
USMLE Step Failure or Multiple Attempts
For many non-US citizen IMGs, a USMLE failure is the biggest concern. Programs worry that:
- You may struggle with CREOG exams and board certification.
- You may not adapt well to U.S. testing and educational expectations.
How to Explain a Failed Step Exam
Your explanation should cover:
- Cause – What specifically led to the failure?
- Response – What concrete actions did you take afterward?
- Result – What improved outcomes followed?
Sample framing (brief, adaptable):
“I failed Step 1 on my first attempt because I underestimated the exam’s breadth and relied too heavily on passive studying while also working part-time. After this result, I completely restructured my preparation: I created a detailed schedule, focused on question-based learning, and sought guidance from senior IMGs who had succeeded. On my second attempt, I passed with a significantly higher score, and subsequently scored [strong/above average] on Step 2 CK. This experience taught me how to build an efficient system for mastering large amounts of material, and since then my exam performance and clinical evaluations have been consistently strong.”
Key points:
- You identify a specific failure in strategy or planning, not vague “stress.”
- You document improved performance on later exams.
- You emphasize skills learned: time management, seeking help, using resources.
If Step scores are no longer numeric, you can emphasize:
- Shelf exam grades
- School exam improvements
- Strong comments about knowledge and judgment in letters
Multiple Low Scores Without Failure
Low but passing exam scores may not be direct “red flags” but can hurt competitiveness, especially for OB GYN. Address them if:
- They are far below your later performance.
- Programs might question your knowledge base.
You could say:
“My early standardized exam scores were modest because I initially studied in a way that prioritized memorization over application. Over time, I shifted to active learning with question banks and spaced repetition. This shift is reflected in my improved performance on [later exams/shelf exams/clinical evaluations], and my faculty have consistently commented on my strong fund of knowledge.”
Then ensure that your recent performance actually supports this statement.
Clerkship Failures, Remediation, or OB GYN Performance Concerns
An OB GYN-specific failure or poor evaluation is particularly sensitive.
Programs need to know:
- Was this an isolated event?
- Was it knowledge, skill, professionalism, or communication?
- What changed afterward?
Example explanation:
“During my OB GYN clerkship, I initially struggled with time management in the operating room and documentation, which resulted in a marginal evaluation. I worked closely with my clerkship director to identify specific behaviors to improve, including pre-reading before cases, better pre-op discussions with patients, and creating templates for notes. In my subsequent surgical rotations and OB GYN electives, I received strong evaluations for punctuality, teamwork, and intraoperative focus, which are reflected in my letters of recommendation.”
Whenever possible, secure a supportive OB GYN letter explicitly stating your improvement.
Gaps, Non-Linear Paths, and Training Interruptions: How to Explain Gaps and Transitions
For a foreign national medical graduate, extended gaps or complex training paths are common—but they must be explained clearly. Programs are asking:
- “Why weren’t you in structured training?”
- “Will this happen again?”
- “Is this person still clinically sharp?”
What Counts as a “Gap”?
3–6 months with no clinical, academic, or relevant professional activity
- Years between graduation and application with little to show
- Time after a previous residency attempt with no clear clinical work
Not all gaps are bad, but unexplained gaps are red flags.
How to Explain Gaps in Medical Training or Timeline
Common reasons:
- Visa or immigration delays
- Family or personal health issues
- Financial constraints requiring work outside medicine
- Military service or national service
- Research-only years without direct clinical work
Your explanation should include:
- Reason for the gap – Stated succinctly and honestly
- Constructive use of time – Even if initially unplanned, what did you eventually do?
- Return to clinical readiness – How did you maintain or restore clinical skills?
Example – Visa and Adjustment Period:
“After graduating medical school in 2017, I had a two-year period where I was unable to participate in direct patient care while resolving immigration and financial challenges. During this time, I supported myself with non-clinical work, but I remained engaged with medicine through online CME courses, USMLE preparation, and volunteer health education in my local community. Once my situation stabilized, I completed multiple U.S. clinical observerships, including OB GYN experiences, and recent attending feedback confirms that I am clinically up to date and capable of functioning effectively in a U.S. hospital environment.”
Example – Family or Health-Related Gap:
“In my final year of medical school, I took a leave of absence for nine months to care for a critically ill family member. I chose to prioritize my family during this time, which delayed my graduation. When I returned, I successfully completed my remaining rotations and performed strongly on my Step 2 CK and OB GYN electives. This experience reinforced my commitment to patient-centered care and to supporting families facing difficult medical decisions.”
Unfinished or Dismissed Prior Residency
This is a major red flag but not always disqualifying if addressed correctly and transparently.
Programs will want to know:
- Why did you leave?
- Were there professionalism or performance issues?
- What have you done since?
Example – Specialty Mismatch (no serious misconduct):
“I began a preliminary internal medicine residency in my home country, believing at the time that it was the right path. However, during my rotations, I realized that my strongest interest and sense of purpose were consistently in women’s health, peripartum care, and the OR environment. I completed my year, left in good standing, and then focused exclusively on developing my OB GYN profile through observerships, research in maternal health, and U.S. clinical experiences. My supervisors in these settings describe me as well-suited for OB GYN and fully committed to the specialty.”
If dismissal was related to performance or professionalism, you must acknowledge and show meaningful remediation, not vague statements.

Professionalism, Visa, and Application-Specific Red Flags
Some red flags are less about scores and more about trust, communication, or logistics.
Professionalism Concerns and How to Address Them
Professionalism issues (lateness, conflict with staff, inappropriate communication, boundary issues) are taken very seriously in OB GYN, where patient trust and team dynamics are crucial.
If your MSPE or evaluations hint at professionalism problems:
- Acknowledge the issue clearly – Don’t pretend it was only a misunderstanding.
- Describe specific behavior changes you implemented.
- Present corroborating evidence—strong subsequent evaluations, leadership roles, letters describing your reliability and teamwork.
Example framing:
“Early in my clinical training, I received feedback that I was not always receptive to criticism and at times appeared defensive when corrected. At first, I focused too much on my intentions rather than how I came across to others. With guidance from my faculty advisor, I began to request regular feedback, practice active listening, and restate suggestions before responding. Over the following year, my evaluations improved, and multiple attendings commented on my growth in communication and teamwork. I understand now that part of being a safe physician is being open to learning from every member of the team.”
Avoid blaming cultural differences as the root cause, though you may briefly acknowledge communication style adjustments if relevant.
Visa-Related Concerns for Non-US Citizen IMGs
For a non-US citizen IMG and foreign national medical graduate, visa status is not a “red flag” by itself, but programs may hesitate due to:
- Unfamiliarity with visa processes
- Institutional limits on sponsoring H-1B visas
- Worry about long-term immigration uncertainty
You can’t change institutional policies, but you can:
- Know clearly which visa you are pursuing (J-1 vs H-1B) and state it consistently.
- Demonstrate stability and commitment to U.S. training.
- Highlight any previous legal, successful stays in the U.S. (if relevant).
- Avoid vague or complicated personal immigration narratives unless asked.
If you have previous visa denials, you do not need to proactively discuss them in your personal statement, but be prepared with a brief, factual explanation at interview if required.
Red Flags Within the Application Itself
Some issues are created by the application process:
- No OB GYN-specific letters of recommendation
- Generic personal statements that don’t explain your path
- Poor spelling/grammar raising concern about communication
- Inconsistencies between dates or activities
Action steps:
- Secure at least two strong OB GYN letters, ideally from U.S. or North American faculty if possible.
- Have mentors or advisors review your ERAS, CV, and personal statement for consistency.
- Make sure your explanation of any red flags appears:
- Briefly in ERAS (if appropriate)
- More personally in your personal statement (if central)
- Clearly and calmly during interviews
Putting It Together: Strategy, Storytelling, and Strengthening Your File
Addressing red flags is not only about explanation—it’s about building enough strength around them that programs see you as a net positive.
Build a Coherent Story Around OB GYN
Your narrative should answer:
- Why OB GYN?
- Why now?
- What have you done that proves this is the right specialty for you?
For a non-US citizen IMG, that means emphasizing:
- Hands-on or observership experience in OB GYN
- Research or projects related to women’s health, maternal-fetal medicine, gynecologic oncology, contraception, or global women’s health
- Service to women’s health communities, both locally and in your home country
If your history includes red flags, your story should show that OB GYN was a conscious, mature choice made after growth, not a fallback.
Tactically Addressing Red Flags in Each Application Component
1. ERAS Application
- Use description boxes judiciously to clarify gaps or unusual issues.
- Use factual, neutral language:
- “Leave of absence due to family health emergency; returned to complete final year with strong clinical evaluations.”
- Avoid emotional language or blaming.
2. Personal Statement
- Include one concise paragraph that addresses the main red flag if it is central (e.g., a major failure, a long gap, or a significant professionalism event).
- Integrate it into your growth story, not as a separate confession at the end.
3. Letters of Recommendation
Ask letter writers (only if they genuinely agree) to:
- Comment on your current reliability and professionalism.
- Highlight your academic recovery if they supervised you after a failure.
- Speak to your suitability for OB GYN specifically.
A letter that says, in effect, “this person had challenges in the past, but I have no concerns now” is very powerful.
4. Interviews
You will almost certainly be asked about red flags. Prepare structured, practiced responses:
- Use past–present–future:
- Past: “Here is what happened.”
- Present: “Here is what I changed and how I perform now.”
- Future: “Here is how this will make me a stronger OB GYN resident.”
Practice answering with a mentor, friend, or advisor until you can do it calmly, confidently, and briefly.
Strengthening Your Application Around the Red Flag
You cannot erase a red flag, but you can outweigh it with:
- Strong recent clinical performance in OB GYN
- Meaningful research with abstracts, posters, or publications
- Consistent volunteer work, especially in women’s health or underserved populations
- Excellent English communication skills, demonstrated in interviews and writing
- Evidence of resilience and maturity, such as leadership roles, teaching, or quality improvement projects
For example, if your issue is older year of graduation, you can still compete if:
- You’ve had continuous clinical involvement (even abroad).
- You’ve completed recent U.S. clinical experiences.
- Your letters say you function at or above the level of current graduates.
FAQs: Addressing Red Flags as a Non-US Citizen IMG Applying to OB GYN
1. I am a non-US citizen IMG with a Step 1 failure. Do I still have a chance to match into OB GYN?
Yes, many applicants with a Step 1 failure have matched, including in OB GYN, but your margin is narrower. You will need:
- A strong Step 2 CK score and evidence of academic recovery.
- Solid OB GYN letters, ideally from U.S. faculty.
- A clear, concise explanation of the failure and what changed.
- Realistic expectations about which programs to apply to (some automatically filter out failures, others are more flexible).
Focusing on community programs, university-affiliated community hospitals, and programs with a history of taking IMGs will improve your odds.
2. How much detail should I give when explaining personal or family issues that caused a gap?
Give enough detail to be credible, but not so much that it becomes the center of your application. One–two sentences explaining:
- The nature of the issue in general terms (e.g., serious family illness, personal medical issue).
- That it has been resolved or is stable.
- That you are now fully able to commit to residency.
Avoid describing deeply personal information that may make interviewers uncomfortable or raise new concerns about future reliability.
3. Should I address my red flags in the personal statement or only if programs ask?
If the red flag is obvious and major (failed exams, long unexplained gap, prior dismissal), it is better to briefly address it in your personal statement and be ready to expand in interviews. This shows you are honest, self-aware, and proactive.
Use only a short paragraph, integrate it into your broader growth story, and avoid apologizing repeatedly. The main focus of your statement should remain your motivation and preparation for OB GYN.
4. As a foreign national medical graduate who needs a visa, is that considered a red flag?
Needing a visa is not a red flag in itself, but it is a practical barrier for some programs. Many institutions have policies about which visas they sponsor (often J-1 only, sometimes H-1B), and some avoid visa sponsorship altogether.
To handle this:
- Research programs thoroughly and apply only to those that sponsor your visa type.
- Present a strong, well-rounded application to justify the additional administrative effort.
- Be transparent—but concise—about your visa needs if asked.
If you frame your profile strongly in all other areas, the visa becomes a logistical consideration, not a negative judgment on your candidacy.
By understanding how OB GYN programs assess risk and by owning, explaining, and offsetting your red flags, you can transform past setbacks into evidence of resilience and maturity. As a non-US citizen IMG, your path may be more complex, but with a strategic approach, thoughtful self-reflection, and targeted strengthening of your application, an obstetrics match is still very much within reach.






















