Applying for residency is one of the highest-stakes transitions in medical education. Your residency applications must showcase your readiness for training, your professionalism, and your potential as a colleague. At the same time, you may be worried about red flags—those elements in an application that could raise questions about your academic record, professionalism, or consistency.
Handled poorly, red flags can derail otherwise strong applications. Handled thoughtfully, they can demonstrate maturity, insight, and professional growth. This guide explains the dos and don’ts of addressing red flags in residency applications, with practical strategies, examples, and language you can adapt.
Understanding Red Flags in Residency Applications
Program directors review hundreds (sometimes thousands) of residency applications each season. They are not only looking for strong metrics; they are also screening for potential concerns that could affect performance, professionalism, or patient care. Recognizing these red flags early allows you to address them directly and strategically.
Common Types of Red Flags in Residency Applications
While every specialty and program weighs issues differently, typical red flags include:
Low or inconsistent USMLE/COMLEX scores
- Step 1/Level 1 significantly below national mean
- Step 2 CK/Level 2-CE lower than Step 1, or large score drop between exams
- Very late Step 2 CK/Level 2-CE scores or no score at time of application
Exam failures or multiple attempts
- Failed Step/Level exams (especially Step 2 CK/Level 2-CE or Step 3)
- Multiple retakes of the same exam
- Delayed progression due to exam performance
Gaps in medical education or training
- Periods of 3+ months not accounted for in medical school
- Time away from medicine (e.g., health issues, family responsibilities, visa problems)
- Extended time to graduate beyond the usual curriculum length
Frequent changes in specialty or training path
- Switching intended specialty late in medical school
- Previous unmatched cycles, especially in a different specialty
- Prior withdrawal from a residency program
Limited or late clinical experience
- Few or no U.S. clinical experiences for international graduates
- Minimal or no sub-internship/acting intern experience
- Gaps between graduation and most recent clinical work
Professionalism or disciplinary concerns
- Academic probation or professionalism probation
- Formal disciplinary actions, suspensions, or leaves of absence
- Unprofessional comments or behavior documented in MSPE or dean’s letter
Inconsistencies in the application
- Conflicting dates between CV, ERAS, and personal statement
- Activities that appear exaggerated, padded, or not credible
- Mismatched content (e.g., personal statement and MSPE telling different stories)
Why Programs Care About Red Flags
Red flags matter because residency is high-pressure training with direct impact on patient care. Program directors are asking:
- Will this applicant pass boards on time?
- Can this person reliably handle clinical responsibilities?
- Are there professionalism risks—lateness, unreliability, interpersonal conflict?
- Has the applicant learned from prior challenges and demonstrated improvement?
Understanding this perspective will help you frame your explanations: you are not just justifying the past—you’re showing why you are now a safe, reliable, and professionally ready trainee.
DOs: Effective Strategies for Addressing Red Flags in Residency Applications
1. Be Honest and Transparent
Programs value integrity more than perfection. If there is a clear red flag in your file, it is almost always better to address it briefly and honestly than to ignore it.
Where to address red flags:
- Personal statement (brief paragraph, not the main focus)
- ERAS “Education/Training” or “Experience” sections (for gaps)
- Additional questions in supplemental applications
- Interviews (if asked directly—answer confidently and consistently)
Example – Gap in training
Instead of:
2019–2020: Personal leave
Try:
From July 2019 to January 2020, I took a leave of absence from medical school due to a family health crisis. During this time, I remained engaged in self-directed study and returned to full-time clinical rotations in February 2020, successfully completing all required clerkships on schedule thereafter.
Honesty should be paired with reassurance: show that the concern has been resolved and that your performance since then supports that.
2. Provide Clear Context and Focus on Resolution
Context is not the same as excuse-making. Your goal is to help the reader understand what happened, see what you learned, and feel confident that the problem will not recur.
When explaining a red flag, structure your explanation around four parts:
- Brief description – What happened (1–2 sentences)
- Contributing factors – Context, not blame (1–2 sentences)
- Actions taken – What you changed or did differently (2–3 sentences)
- Outcome and stability – Evidence things are now on track (2–3 sentences)
Example – Failed Step 1, improved Step 2 CK
I did not pass Step 1 on my first attempt, which reflected ineffective study strategies and difficulty adjusting to the volume of material. In response, I met regularly with our academic support team, adopted structured question-based learning, and created a detailed study schedule. I also joined a peer study group with senior students who had performed well. These changes resulted in a significant improvement, and I passed Step 1 on my second attempt and later scored [XXX] on Step 2 CK, reflecting both stronger content mastery and more effective exam preparation.
Note that this explanation:
- States the issue plainly
- Avoids blaming others
- Emphasizes specific, concrete steps
- Ends with objective evidence of improvement
3. Highlight Resilience, Professional Growth, and Insight
Many program directors will tell you: every physician faces setbacks. What differentiates strong residents is how they respond. Use your red flags to demonstrate:
- Self-reflection: “What did I learn about myself from this?”
- Professional growth: “What did I change in my habits or approach?”
- Resilience: “How did I recover and continue forward?”
- Alignment with residency demands: “How will this help me as a resident?”
Example – Professionalism concern turned into growth
During my third-year rotations, I was counseled about late documentation and delayed note completion. Receiving this feedback early in my clinical training was difficult but pivotal. I began using checklists, time-blocking my day, and asking senior residents for strategies to improve efficiency. Over the next few months, I consistently completed notes on time and received positive feedback on both organization and reliability. This experience increased my appreciation for accountability and time management—skills I will carry with me into residency.
When you frame your red flag as a turning point that led to sustainable change, you transform it from a liability into evidence of maturity.
4. Emphasize Your Strengths and Positive Trajectory
Your red flags should be one part of the story, not the center of it. Balance your explanation with strong evidence of your readiness:
- Upward trends in grades or exam scores
- Honors or high marks in core clerkships or sub-internships
- Strong, specific letters of recommendation
- Longitudinal commitment to a specialty or patient population
- Research, QI projects, or leadership roles demonstrating responsibility
Example – Balancing academic concerns with strengths
Although my Step 1 score is below the national average, my clinical performance and subsequent exam scores better reflect my readiness for residency. I achieved honors in Internal Medicine, Surgery, and my sub-internship, and my attending physicians consistently commented on my clinical reasoning and reliability. My Step 2 CK score of [XXX] further demonstrates my growth and preparation for the demands of residency.
Make it easy for program directors to conclude: “Yes, there were challenges—but this applicant has clearly moved past them and is now performing at a level that will be safe and successful in our program.”
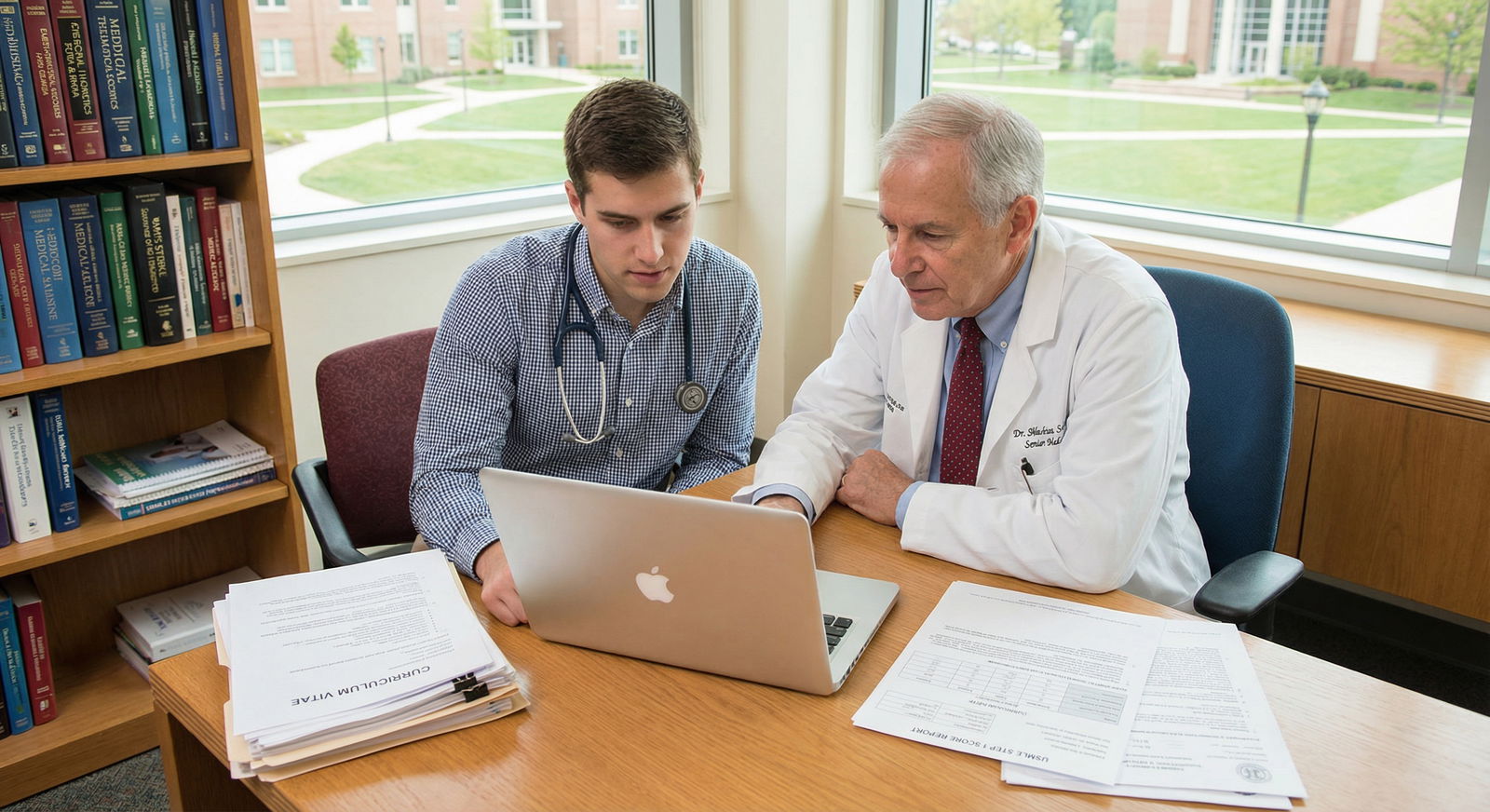
5. Seek Guidance, Feedback, and Mentorship
You are too close to your own story to always see how it will be perceived. Seek input from:
- Academic advisors or deans
- Clerkship directors or specialty advisors
- Residents or fellows in your target specialty
- Mentors who know you and your work well
- Professional application review services (when appropriate)
How mentors can help:
- Determine which red flags must be addressed and which can be left alone
- Edit explanations to be clear, concise, and professional
- Help you choose the best location to address each concern
- Conduct mock interviews focused on difficult questions about your record
Example approach to a mentor:
“I’m concerned about how to address my repeat Step 1 attempt and my leave of absence. Could you help me decide whether to mention these in my personal statement, and review a brief explanation to make sure it sounds professional rather than defensive?”
Their outside perspective can transform your explanations from anxious and apologetic to confident and growth-focused.
DON’Ts: Common Mistakes When Addressing Red Flags
1. Don’t Make Excuses or Shift Blame
Programs understand that life is complicated—health crises, family emergencies, financial pressures, and systemic issues are real. However, they also need residents who can take responsibility and adapt.
Avoid:
- Blaming specific faculty, institutions, or exam boards
- Overemphasizing unfairness or victimization
- Implying the problem was entirely external
Instead, acknowledge the challenge but focus on what you controlled and changed.
Weak framing:
The exam was unfair, and the questions didn’t reflect what we were taught, so I failed Step 1.
Stronger framing:
I struggled to adapt to the style and breadth of Step 1, and my initial study strategies were not effective. I sought guidance from academic support, shifted to more question-based learning, and significantly improved my performance on my second attempt and on Step 2 CK.
2. Avoid Over-Explaining or Over-Sharing
You do not need to provide intimate personal details or a full emotional narrative. Too much detail can:
- Make the reader uncomfortable
- Sound like justification or defensiveness
- Shift focus away from your qualifications and strengths
Keep explanations brief, factual, and forward-looking.
Example – Personal health issue (appropriate level of detail)
During my second year, I experienced a significant health issue that required surgery and a short recovery period. With support from my school, I took a brief leave, then returned to full-time coursework and subsequently passed all exams and completed clinical rotations on schedule. This experience deepened my empathy for patients and reinforced my commitment to medicine.
Notice that this does not include diagnosis, symptoms, or extensive personal narrative—just enough information to clarify the situation and outcome.
3. Don’t Ignore Obvious Red Flags
If something is clearly visible in your application, programs will notice—even if you avoid it. Ignoring major red flags can be perceived as:
- Lack of self-awareness
- Avoidance or dishonesty
- Inability to reflect and grow
You usually should address:
- Failed Step/Level exams
- Formal leaves of absence or probations
- Extended gaps in education or clinical work
- Withdrawal from a prior residency program
You may not need to address:
- A single lower-than-expected exam score without failure, if everything else is strong
- One or two mid-range clerkship grades amidst generally strong performance
When in doubt, ask a mentor or advisor whether a particular issue rises to the level of requiring explicit explanation.
4. Don’t Compare Yourself to Other Applicants
Your residency application is about your journey, not how you rank socially or statistically against your peers. Comparisons can:
- Sound insecure or resentful
- Draw attention to what you lack instead of what you offer
- Undermine your professional tone
Avoid statements like:
- “Many of my classmates had fewer obstacles than I did.”
- “Compared to other applicants, my scores are not terrible.”
- “Others with similar issues have matched at top programs.”
Instead, focus on your unique path, your growth, and your alignment with the specialty.
5. Don’t Dwell on the Negative or Center Your Application Around Red Flags
Your application should primarily showcase:
- Why you want this specialty
- What you’ve done to prepare
- How you function in teams and clinical environments
- What you bring to a residency program
Red flags deserve brief, thoughtful acknowledgement—not pages of explanation.
Common misstep: Using half of your personal statement to discuss past failures or hardships.
Better approach:
- One concise paragraph (or less) for explanation
- Majority of space devoted to your passion for the specialty, clinical experiences, and future goals
Example – Integrating a red flag into a broader narrative:
Early in medical school, I struggled with the transition to independent learning and did not initially pass Step 1. This challenge prompted me to overhaul my study strategies and seek mentorship, leading to marked improvement on retesting and on Step 2 CK. More importantly, it transformed the way I approach complex material and reinforced my persistence. In my Internal Medicine clerkship, I applied these skills to managing intricate cases, and I found great satisfaction in synthesizing clinical data to guide patient care…
Here, the red flag is addressed, then the narrative quickly returns to your strengths, passions, and readiness.
Putting It All Together: Application Strategies by Red Flag Type
To make this more actionable, here are tailored strategies for some common scenarios.
Low Board Scores (Without Failure)
Where to address:
- Briefly in personal statement only if scores are substantially below average
- Highlight strong clinical performance and upward trends
Key strategies:
- Emphasize Step 2 CK/Level 2-CE if significantly higher
- Showcase honors in core clerkships and sub-internships
- Ask letter writers to comment on your clinical reasoning and reliability
Failed Step/Level Exam
Where to address:
- Personal statement (short paragraph)
- Be prepared to discuss in interviews
Key strategies:
- Highlight concrete changes in preparation methods
- Show improved performance on subsequent exams
- Emphasize consistent performance since the failure
Gaps in Education or Training
Where to address:
- ERAS Education section (accurate dates)
- Personal statement (brief explanation)
- Supplemental applications if asked directly
Key strategies:
- State the reason in broad, professional terms (health, family, research, visa issues, etc.)
- Emphasize how you maintained or regained clinical knowledge and skills
- Show strong and recent clinical engagement afterward
Professionalism/Disciplinary Issues
Where to address:
- Personal statement (succinctly)
- Interview (expect to be asked)
Key strategies:
- Accept responsibility without defensiveness
- Describe what you learned and specific behavior changes
- Emphasize subsequent clean record and positive evaluations
- Consider a mentor letter directly addressing your growth
Prior Withdrawal from a Residency or Unmatched Cycles
Where to address:
- Personal statement (focused on why you are now prepared)
- Interviews (honest, reflective explanation)
Key strategies:
- Explain circumstances (fit, personal factors, health) without disparaging people or programs
- Highlight what you did with the interim time (clinical work, research, courses)
- Clarify your commitment to the new specialty and what has changed since the prior attempt

Frequently Asked Questions About Red Flags in Residency Applications
1. Should I mention every red flag in my application, or only the major ones?
You do not need to catalog every minor imperfection. Focus on major, objective issues that program directors will clearly see and have to interpret:
- Failed board exams
- Formal leaves of absence, probations, or suspensions
- Extended gaps in education or clinical experience
- Prior withdrawal from a residency program
If something is subtle (e.g., a single mid-range clerkship grade) and your overall record is strong, you generally don’t need to call extra attention to it. When unsure, discuss it with an advisor or mentor who understands residency selection.
2. How detailed should I be when explaining personal or health-related red flags?
Keep personal details limited and professional. You can state that you went through a significant personal, family, or health challenge without providing sensitive specifics. The key points to address are:
- That a legitimate issue occurred
- That it has been appropriately addressed or stabilized
- That your current health and circumstances allow you to meet the demands of residency
- What you learned or how you grew from the experience
If you are comfortable, you may share more detail at the interview stage, but even then, you are not obligated to disclose intimate medical information.
3. What if my red flags are academic and I don’t have a dramatic story—just underperformance?
You do not need a dramatic story to justify every lower grade or test score. For modest academic concerns without failure:
- Acknowledge the challenge briefly (e.g., “I initially struggled to adjust to the pre-clinical curriculum…”)
- Focus on what specific strategies you adopted to improve
- Highlight objective evidence of growth (later grades, exams, sub-internship performance)
Programs often value a clear upward trajectory more than a “perfect” record with no adversity.
4. Can red flags ever become strengths in my residency application?
Yes—when handled thoughtfully, red flags can highlight:
- Resilience – You faced adversity and came back stronger
- Self-awareness – You can recognize and analyze your own limitations
- Professional growth – You changed your behavior in measurable ways
- Empathy – Personal challenges can deepen your understanding of patients’ struggles
The key is not to romanticize the difficulty, but to show how it changed your approach to learning, working in teams, or caring for patients, and how that will make you a better resident and physician.
5. How can I prepare for interview questions about my red flags?
Anticipate and rehearse answers to likely questions, such as:
- “Can you tell me about your Step 1 failure and what changed afterward?”
- “What led to your leave of absence, and how did you use that time?”
- “How have you addressed concerns noted in your dean’s letter?”
Preparation tips:
- Use the same four-part structure: brief description → contributing factors → actions taken → current status and growth
- Practice out loud with a mentor or friend to ensure you sound confident and not defensive
- Keep your answers concise; avoid wandering into unnecessary detail
- End on a forward-looking note, tying your growth to success as a resident
Final Thoughts: Owning Your Story and Demonstrating Professional Growth
Every application to residency is more than a list of scores and rotations; it is a narrative about your professional identity and your path through medical education. Red flags do not automatically disqualify you, but they must be handled thoughtfully.
To summarize the most important strategies:
- Be honest and transparent about significant concerns
- Provide concise, contextual explanations without excuses
- Demonstrate resilience, insight, and concrete changes in behavior or study methods
- Emphasize your current strengths, trajectory, and readiness for residency
- Seek mentorship and feedback to refine your explanations and application strategy
When you approach red flags with professionalism and maturity, you communicate exactly the qualities residency programs value most. Your journey—including its challenges—can still lead to a strong match if you frame it carefully, highlight your growth, and show clearly why you are ready for the next step in your medical career.






















