
Understanding Red Flags for MD Graduates Pursuing Clinical Informatics
For an MD graduate targeting clinical informatics, red flags in a residency or fellowship application can feel especially intimidating. Clinical informatics is still a relatively small and competitive field, often populated by applicants with strong academic and technical backgrounds. Program directors must trust that you can handle both the clinical and the health IT sides of the work. Any perceived weakness can raise concerns.
Yet many successful clinical informatics physicians have imperfect paths: failed exams, non‑traditional timelines, leaves of absence, or early career pivots from other specialties. What distinguishes a successful candidate is not a flawless record, but a convincing, honest narrative and clear evidence of growth.
This article will help you:
- Recognize common red flags in residency and fellowship applications
- Learn how to explain gaps, failures, or career pivots strategically
- Tailor your story to the expectations of clinical informatics programs
- Frame your health IT experience as a strength—not a detour
Although the focus is clinical informatics, the strategies apply broadly to the allopathic medical school match, transitional year positions, and later clinical informatics fellowships and health IT training pathways.
Common Red Flags for MD Graduates Interested in Clinical Informatics
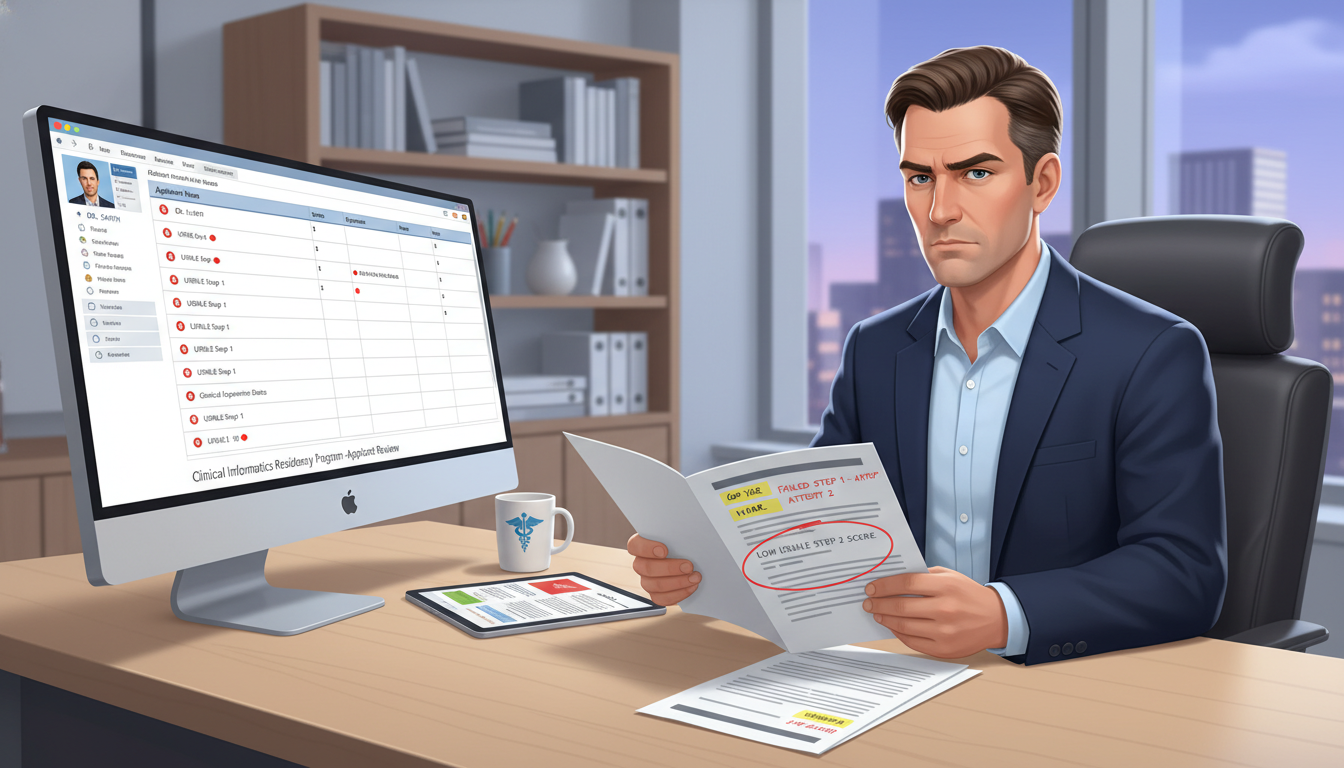
Clinical informatics program directors review your file first as a physician, and second as a tech‑savvy innovator. The usual red flags residency application committees worry about still apply—USMLE performance, professionalism issues, gaps, and so on. Below are the most frequent concerns you should be ready to address.
1. Exam Failures and Low Scores
Examples:
- Step 1 or Step 2 CK failures or multiple attempts
- COMLEX/USMLE score trends that decline over time
- Very low scores that may trigger an automatic screening filter
Why it matters for clinical informatics:
Clinical informatics work is cognitively demanding. Programs assume that if you struggled with standardized exams, you may require extra support with board exams later. However, this is addressable if you can demonstrate insight and improvement.
2. Unexplained Gaps in Training or Employment
Examples of gaps:
- A semester or year off during medical school
- Several months not enrolled or not employed after graduation
- Time spent in non‑clinical roles (industry, research, startup) without clear documentation
Program directors accept that careers are increasingly non‑linear. What worries them is ambiguity: unexplained time that could hide disciplinary issues, immigration problems, or loss of motivation.
3. Course Remediations or Academic Probation
Examples:
- Repeating clerkships
- Failing preclinical courses
- Academic probation or being “out of phase” with your original class
These raise concerns about your consistency and resilience—especially if combined with other issues like exam failures or poor clinical evaluations.
4. Professionalism and Conduct Concerns
This is the single hardest category to overcome.
Examples:
- Formal professionalism citations
- Disciplinary actions (HIPAA violations, unprofessional behavior, academic integrity issues)
- Dismissal or required withdrawal from an allopathic medical school or residency
Clinical informatics often involves broad systems access, sensitive patient data, and cross‑department collaboration with IT and leadership. Any question about your professionalism will weigh heavily.
5. Multiple Specialty Switches or Career Drift
Examples:
- Started and left more than one residency
- Long sequence: MD → research → non‑clinical job → another degree → now applying to residency or clinical informatics fellowship
- Appears to be “shopping” for anything that will take you
For a field like clinical informatics—which values intentionality and long‑term commitment—programs want to know you’re not simply defaulting to informatics after failing elsewhere.
6. Non‑Traditional Pathways and Extended Timelines
Examples:
- Graduated from an allopathic medical school several years ago without completing residency yet
- Long time between MD graduation and first residency application
- MD plus several years in health IT, consulting, or industry, now returning to clinical training
These aren’t inherently negative, especially for clinical informatics, which attracts people with industry experience. But you must connect the dots clearly and convincingly.
How Clinical Informatics Programs View Red Flags
Clinical informatics fellowships and informatics‑oriented residency tracks think differently from purely clinical programs in some key ways.
1. They Value Diverse Backgrounds
If you have:
- Experience with electronic health record (EHR) optimization
- Time in a digital health startup or health IT company
- Work in data analytics, quality improvement, or implementation science
These are strong assets—even if they overlap with “gaps” in traditional training. Programs may see your time outside usual clinical roles as a feature, not a bug, provided your clinical foundation is sufficient.
2. They Weigh Cognitive and Technical Skills Heavily
Scoring concerns are still important, but informatics programs may be more forgiving of an early exam failure if you:
- Show strong later performance (e.g., improved Step 2 CK, relevant board scores)
- Have robust analytical or technical achievements (publications, coding projects, data analytics roles)
- Demonstrate the ability to manage complex systems and long projects
The question becomes: Can this MD graduate succeed in a cognitive, systems‑level discipline that demands sustained attention and problem‑solving?
3. They Scrutinize Professionalism and Trustworthiness
Clinical informatics physicians:
- Have broad EHR configuration access, including sensitive patient information
- Influence workflows that affect safety, billing, and regulatory compliance
- Work with C‑suite leaders, IT departments, and front‑line clinicians
Any history of integrity or professionalism issues is far more concerning here than a test failure. Be prepared to show remediation, oversight, and strong references.
4. They Look for a Coherent Narrative Toward Informatics
Red flags become less problematic when they fit logically into a believable story:
- “I discovered a passion for data and systems through a research year after failing Step 1; I improved my exam approach, passed later exams, and have spent the last two years in health IT training and quality improvement.”
- “I left my initial residency due to misalignment in specialty; during that transition, I worked on EHR optimization and found clinical informatics to be the right intersection of my interests.”
In short: Consistency, insight, and purpose can transform red flags into inflection points.
How to Address Specific Red Flags: Scripts and Strategies
Below are practical approaches and language you can adapt. The principles are the same for the allopathic medical school match, categorical programs, prelim years, or later clinical informatics fellowships.
1. Addressing Failures and Low Scores
Programs want to know:
- What happened?
- What did you learn?
- What changed in your behavior and performance?
General principles:
- Be factual and concise—no long emotional explanations
- Avoid blaming others (school, exam, personal conflicts)
- Emphasize concrete changes in your study methods or support systems
Example paragraph for ERAS “Additional Information” or a personal statement:
During my second year of medical school, I failed Step 1 on the first attempt. I underestimated the volume of material, relied on passive review, and did not adjust my strategy when my practice scores plateaued. With faculty guidance, I transitioned to a structured schedule emphasizing active recall, spaced repetition, and timed practice exams. I also addressed underlying anxiety through counseling. On my second attempt, I passed comfortably and subsequently improved my performance on clerkship shelf exams and Step 2 CK. This experience reshaped how I approach complex learning tasks and has made me more deliberate and data‑driven in my preparation—skills I now apply when analyzing clinical workflows and informatics projects.
For clinical informatics specifically, connect this to your systems thinking:
- Highlight that you used performance data (NBME practice scores, question bank analytics)
- Show how you now use metrics in QI or EHR projects similarly
In interviews, be ready with a short, confident answer:
- 1–2 sentences describing the cause
- 1–2 sentences describing what you changed
- 1–2 sentences on how that change has persisted and benefited you
2. How to Explain Gaps in Training or Employment
How to explain gaps is one of the most searched—and misunderstood—areas. The worst approach is to leave gaps unexplained or vaguely referenced.
Common legitimate reasons for gaps:
- Personal or family health issues
- Visa or immigration delays
- Dedicated research or degree programs
- Work in health IT, informatics, or industry roles
- Caregiving responsibilities or financial necessity
Guidelines:
- Give a brief, truthful reason (you do not need to disclose intimate personal details)
- Show that the situation is resolved or stable
- Emphasize what you did during the gap that is relevant—especially health IT training, research, or informatics projects
Example explanation for an MD graduate residency or fellowship application:
From July 2021 to March 2022, I took a leave from clinical training due to a family health crisis that required my support. During this period, I completed remote coursework in health informatics and volunteered with the quality improvement team at our affiliated hospital, helping to analyze readmission metrics. The family situation has since stabilized, and I have returned to full‑time work with a renewed appreciation for systems‑level interventions that support patients and families.
If your gap was primarily for industry or health IT work, be explicit:
After graduating from an allopathic medical school in 2019, I worked for two years as a clinical analyst with a major EHR vendor. I led projects on order set optimization and clinical decision support. This role clarified my commitment to pursuing clinical informatics fellowship after residency, and my goal now is to integrate rigorous clinical training with my existing health IT experience.
Here, your “gap” becomes targeted preparation.
3. Addressing Academic Probation or Remediation
Programs want reassurance that the issues are not ongoing.
Key elements to cover:
- Context (brief, without blame)
- Concrete steps taken (tutoring, time management changes, counseling if relevant)
- Sustained improvement (no repeat issues, strong later performance)
Example:
Early in my clinical years, I struggled to balance clerkship responsibilities with independent study and fell behind in two core rotations, resulting in temporary academic probation. With guidance from the dean’s office, I adopted a structured weekly schedule, met regularly with a learning specialist, and sought frequent feedback from supervising physicians. I successfully remediated both rotations and have since completed all subsequent rotations on time with strong evaluations. This period helped me build more robust organizational habits, which I now apply to managing multi‑phase informatics projects and residency‑level responsibilities.
Whenever possible, include supporting documentation: a letter from your dean describing how the issue was resolved and your subsequent performance.

Crafting Your Narrative as an MD Graduate Targeting Clinical Informatics
Beyond explanations, you need a coherent, forward‑looking story that fits the expectations of both:
- The allopathic medical school match and residency programs
- Future clinical informatics fellowships and health IT leadership roles
1. Establish a Clear Arc: From Clinical Foundations to Systems Impact
Your narrative should show:
- Solid clinical training and patient‑centered motivation
- Exposure to systems problems (workflow inefficiencies, data gaps, safety issues)
- Discovery of informatics as a tool to solve those problems
- Concrete steps you’ve taken (projects, coursework, health IT training)
- How residency (and later a clinical informatics fellowship) fits into that plan
Even if your path is winding, make the direction unmistakable.
2. Connect Red Flags to Growth Relevant to Informatics
Every addressed red flag should end with what you gained that’s relevant to informatics:
- Exam struggles → improved data‑driven learning, persistence with complex problems
- Gap for caregiving → empathy for patient experience, interest in telehealth solutions
- Time in industry → understanding of implementation challenges, vendor relationships
Example transformation of a red flag into a strength:
After completing one year of internal medicine residency, I realized my strongest interest lay not in subspecialty practice but in improving the EHR tools my colleagues relied on daily. Stepping away from residency was a difficult decision, but it led me to a role as a clinical informatics associate, where I worked directly with clinicians and IT to redesign admission order sets. This experience confirmed that my long‑term contribution lies at the intersection of clinical medicine and informatics. I am now seeking a residency program that values innovation and will prepare me for a clinical informatics fellowship.
Be sure to show that you understand the necessity of strong clinical training before or alongside informatics work.
3. Use Letters of Recommendation Strategically
For applicants with red flags, third‑party voices are critical.
Aim for letters that:
- Explicitly address prior concerns (e.g., a clerkship director who can attest to your professionalism after a past issue)
- Highlight your reliability, ethics, and teamwork in informatics‑related work
- Come from mixed backgrounds: a clinical supervisor, an informatics mentor, a research PI
For clinical informatics aspirants, at least one letter should speak directly to:
- Your aptitude for systems thinking
- Experience with EHRs, data analysis, quality improvement, or digital tools
- Your potential as a future informatics fellow or health IT leader
4. Align Your Activities and CV with Your Stated Goals
Programs are wary of applications where the personal statement claims a passion for informatics, but the activities list shows nothing related.
If you’re aiming for future clinical informatics fellowship or health IT training, your CV should ideally include:
- EHR optimization work or super‑user roles
- Quality improvement projects with a data or workflow component
- Participation in informatics, data science, or health IT electives
- Hackathons, app development, or related technical projects
- Publications or presentations involving informatics, AI, or data analytics
If you lack these, consider building them now, even during a gap year:
- Reach out to your institution’s informatics department for volunteer or part‑time work
- Take a formal or online course in health informatics, data science, or SQL/R/Python
- Join a registry or quality data project and contribute to analysis or dashboard building
Then, reference these experiences directly when addressing failures or explaining why you took extra time before residency.
Practical Tips for Interviews and Application Documents
1. Anticipate and Rehearse Tough Questions
Classic red‑flag questions you should practice:
- “Can you walk me through what happened with your Step 1/Step 2 attempt?”
- “I see a gap between your MD graduation and this application. How did you spend that time?”
- “Why did you leave your previous residency, and what did you learn from that experience?”
- “Given your interest in informatics, why is residency still important to you?”
Use the 3‑part framework:
- Brief, factual description
- Actions and learning
- Evidence of improvement and alignment with your current goals
2. Maintain a Calm, Non‑Defensive Demeanor
Program directors are assessing not just what happened, but how you talk about it:
- Acknowledge legitimate concerns without becoming defensive
- Avoid oversharing or dramatizing personal difficulties
- Keep the focus on your professional growth and how you’ll excel now
3. Be Consistent Across All Materials
Inconsistencies between:
- ERAS explanations
- Personal statement
- Dean’s letter (MSPE)
- Interview answers
…can be more damaging than the red flag itself. Ensure your story is accurate, consistent, and verifiable.
4. Highlight Successes Since the Red Flag
Whenever you discuss a challenge, quickly pivot to:
- Strong recent clinical evaluations
- Leadership in informatics or QI projects
- New skills in health IT training, data analysis, or programming
- Positive feedback from supervisors and multidisciplinary teams
Your message: “That issue was real, I learned from it, and my recent performance proves it.”
Putting It All Together: Example Profiles and Approaches
Scenario 1: MD Graduate with Step Failure, Now Pursuing Clinical Informatics
- Step 1 failed once, passed on second attempt
- Strong Step 2 CK, honored several clerkships
- Spent a research year in a clinical data science lab
Approach:
- Briefly explain the Step 1 failure as a study‑strategy and preparation issue
- Emphasize improved methods, better scores, and strong clerkship performance
- Highlight your research year as deep, relevant experience leading to an interest in clinical informatics
- In your personal statement, clearly articulate how residency builds the clinical expertise you need before a future clinical informatics fellowship
Scenario 2: MD with Long Gap Working in Health IT, Re‑Entering Clinical Training
- Graduated from an allopathic medical school 4–5 years ago
- Took time for family reasons, then worked in EHR implementation and analytics
- Now applying for a prelim or categorical residency with a plan for clinical informatics fellowship
Approach:
- Clearly describe the non‑clinical period (caregiving, etc.) and when it stabilized
- Detail your subsequent health IT training and work—projects, impact, tools used
- Reaffirm your commitment to hands‑on patient care and why you’re returning to clinical training now
- Obtain strong letters from both your health IT supervisors and any recent clinical supervisors (locums, volunteer clinics)
Scenario 3: Prior Residency Resignation and Pivot to Informatics
- Completed PGY‑1 in another specialty, resigned due to poor fit
- Worked in an informatics role for a year
- Now applying in internal medicine or another core specialty with eyes on informatics
Approach:
- Explain the mismatch as a thoughtful career correction, not a failure of motivation
- Avoid criticizing the prior program; focus on self‑reflection and discovery of informatics interests
- Draw a clear line from PGY‑1 clinical experience → informatics work → chosen specialty → future clinical informatics fellowship
- Demonstrate stability and readiness to complete residency this time, supported by recent performance evaluations and informatics achievements
FAQs: Addressing Red Flags When Aiming for Clinical Informatics
1. Do I need a perfect record to match into a residency and eventually a clinical informatics fellowship?
No. Many current clinical informatics physicians had setbacks—failed exams, late discoveries of their passions, or circuitous paths through health IT roles. What matters is how convincingly you address failures, explain gaps, and show consistent growth. Programs want to see that any past issues are resolved, that you’ve developed mature insight, and that your recent performance is strong and aligned with your goals.
2. How much detail should I share about personal or health‑related reasons for gaps?
You should be honest but not compelled to share intimate details. A good rule is to:
- Name the general category (e.g., personal health issue, family health crisis, immigration delay)
- State that the situation is now stable or well‑managed
- Emphasize productive activities during or after the gap (coursework, research, health IT roles)
Program directors are primarily concerned with whether you’re ready for the demands of residency and future informatics training, not the specific personal details.
3. I have a failed Step exam. Will that automatically exclude me from clinical informatics opportunities later?
Not automatically. A Step failure is a red flag, but it can be mitigated by:
- Strong subsequent scores (especially Step 2 CK and residency in‑service exams)
- Evidence of disciplined, data‑driven learning methods
- Robust clinical and informatics‑related performance during residency
Clinical informatics fellowship directors often review the full trajectory. A single early failure, followed by clear improvement and strong residency performance, is usually not disqualifying.
4. I’ve spent years in health IT and haven’t done full‑time clinical work. How can I reassure programs about my clinical readiness?
Focus on three elements:
- Recency of clinical exposure: Any recent moonlighting, locum work, volunteer clinics, simulation sessions, or refresher courses.
- Ongoing clinical learning: CME courses, board prep, or structured reading that show you’ve maintained medical knowledge.
- Integration with informatics work: Demonstrate that your health IT roles kept you close to real clinical workflows, guidelines, and safety standards.
Frame your industry time as a strength—deep exposure to EHRs, data, and implementation challenges—while clearly affirming your commitment to regaining and advancing your bedside skills through residency, then continuing into clinical informatics fellowship and advanced health IT training.
By anticipating concerns, building a coherent narrative, and aligning your experiences with the values of both residency and clinical informatics programs, you can transform red flags from permanent liabilities into evidence of resilience, insight, and purpose—qualities that strong informaticians share.






















